Abstract
Background. Reconstructing a breast mound constitutes the basis of breast reconstruction. The breast can be reconstructed using autologous tissue, implants or a combination thereof. The number of women wishing a breast reconstruction has increased, but evaluation of the results is lacking. The current study examined the long-term results from three methods of breast reconstruction to assess the subjective and the objective outcome. Patients and methods. Patients undergoing first-time post mastectomy reconstruction, selected from the cohort of Danish women in the Central and North Region of Denmark, were evaluated. We included 363 women, reconstructed in 1990–2005. Data was collected from patient charts, a study specific questionnaire (to be found online at http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2011.584554) and a clinical follow-up visit. The questionnaire included questions regarding demographic background and evaluation of the reconstructed breast and donor site. The clinical follow-up visit included an examination of the overall result and donor site. Results. The questionnaire was answered by 263 women, of whom 137 had an implant, 26 had a latissimus dorsi musculocutaneus flap and 100 had a pedicled transverse rectus abdominis musculocutaneus flap. Women reconstructed with autologous tissue were significantly more pleased with the result of the breast reconstruction than women reconstructed with an implant. After a median of seven years, neither the patient's age nor the length of time since the reconstruction significantly affected the patients’ opinion of the overall result. There was no difference in the incidences of minor complications among the different reconstructive methods. BMI, smoking and radiation therapy influenced the risk of complications. Objective evaluation of the 180 women participating in the follow-up visit was in agreement with data from the questionnaire. Conclusion. The type of reconstruction had a significant long-term influence on patient satisfaction and the objective result. Women reconstructed with autologous tissue were significantly more pleased, and the objective outcome was assessed as superior.
Since the beginning of breast reconstructive surgery, the techniques have evolved from being a rarely performed surgical venture into a daily occurrence, now an important part of the rehabilitation process following a mastectomy. Therefore, obtaining more knowledge of the long-term results is important to continue the work of optimizing patient information and surgical procedures.
There are basically two possible ways to reconstruct the breast. One includes the transfer of tissue from a donor site into the area of reconstruction. The other is the use of an implant to create the breast mound. The implant may have to be supplemented with autologous tissue. Initially, all types of reconstructions are considered for the individual woman. But in reality, the decision is influenced by a whole array of considerations which not always gives the woman a choice. How the mastectomy was performed influences the skin quality and the position of the scar. Co-morbidity and the proportions of the opposite breast to be matched are considered. Last, but not least important, are the expectations and preferences of the woman.
Smoking, overweight and radiation therapy (RT) are considered as surgical risk factors [Citation1, p 763–788, Citation2]. Previously published studies have suggested a significantly enhanced risk of complications and adverse outcome for patients undergoing implant reconstruction after radiation therapy, while there is controversy regarding the influence of radiation on autologous reconstructions. Smoking and overweight are reported to increase the complications of autologous breast reconstructions more than breast reconstructions with an implant [Citation3–11].
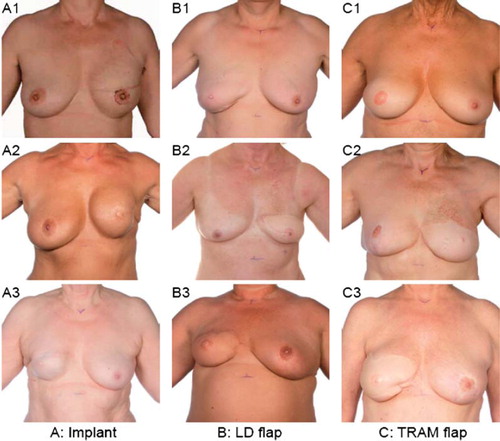
shows frequently used regional pedicled flaps the Latissimus Dorsi flap (LD flap) [Citation12] and the pedicled transverse abdominal muscle flap (TRAM flap) [Citation13].
Figure 1. Three methods of breast reconstruction. A. with a submuscular implant. B. with a latissimus dorsi flap (LD flap). C. with a pedicled transvers rectus musculocutaneous flap (TRAM flap). Courtesy Department of Clinical Photo, Aarhus University Hospital, Denmark.
The TRAM flap has the potential for reconstruction of a fairly large breast. The LD flap is a good breast reconstruction (BR) technique for women with deficient abdominal tissue. Autologous tissue generates a breast mound that resembles the opposite breast with ptosis and a naturally soft feeling. Both the LD flap and the TRAM flap techniques are good solutions for women with insufficient quality skin and muscle because of the mastectomy or after radiotherapy (). The disadvantage of reconstructions with autologous tissue is the necessity of a donor site, with the risk of morbidity and additional scarring. There is a longer hospitalization and sick leave. The skin of the donor site can be different in texture and pigmentation from the breast skin () [Citation1, p 763–788, Citation14, p 177–187]. Reconstruction using an implant requires a shorter hospital stay; it does not generate new scars and the color of the breast skin is not altered (). The method is very useful in bilateral reconstructions and especially for women with a small to moderate breast size. However, breast reconstruction with an implant may require time consuming expansion with a temporary saline implant (expander) in order to match the opposite breast size and achieve a softer breast. The implant lasts a limited time and is a foreign object, thus inducing a tissue reaction that may result in capsular contracture (). There may be difficulties in recreating the infra-mammary fold, the natural breast ptosis and in achieving lasting symmetry in unilateral reconstructions.
The aim of the study was to evaluate the objective and subjective long-term results of different reconstructive procedures (implant, LD flap, TRAM flap) in the cohort of Danish women from the central and northern region of Denmark.
Patients and methods
The Central Denmark Region and The North Denmark Region constitute a geographic area with a population of 1.8 million people representing one third of the Danish population.
displays a flowchart of the cohort identified from the operating room case log, who underwent a BR at the Department of Plastic Surgery Aarhus University Hospital between January 1990 and December of 2005. The department was the only plastic surgery unit servicing the two regions until 2005. Data was collected retrospectively from charts, the Danish Breast Cancer Cooperative Groups database and the Danish Civil Registration System to deselect deceased patients or patients with known recurrence.
Figure 3. Postmastectomy breast reconstruction and common complications. A is reconstructions with implants. A2-3. Capsular contracture and loss of symmetry. B. Reconstructions with the LD flap. B2-3. Inferior color and size match. C. Reconstructions with the TRAM flap. C2-3. Insufficient skin color match and retraction after necrosis. Courtesy Department of Clinical Photo, Aarhus University Hospital, Denmark.
The charts were examined to exclude patients with reconstruction for other reasons than cancer, with cancer relapse, incomplete charts, the first reconstruction performed in other regions of Denmark, males or patients who had emigrated or died.
After this exclusion, 452 women were selected and 363 of the 452 women were included in the current study (). The remaining 89 women were either reconstructed with microsurgical techniques or with an immediate procedure. The 363 women were reconstructed with a delayed reconstruction of pedicled TRAM flap, LD flap or implant. The women were sent a study specific questionnaire and invited to a follow-up visit.
The implant was placed under the pectoral muscle to achieve better coverage ().
In a BR with the LD flap, the skin and muscle from the back with its vessels were tunneled under the skin below the axilla and brought out in the mastectomy defect and shaped into a new breast.
In the TRAM flap reconstruction, most of the rectus muscle on one side of the abdomen was included with the skin island and subcutaneous tissue. The flap was tunneled under the abdominal tissue with the vessels and transposed into the site of the old mastectomy scar as the new breast.
Patient charts from these 363 women were reviewed for associated demographics,-patient age, body mass index (BMI), the prevalence of tobacco use and complications. Pre-reconstruction radiation treatment was in accordance with the national guidelines [Citation15].
Data regarding complications was extracted from the charts if described by the doctor in relation to the first breast reconstructive procedure. Complications were categorized as being minor or major. A minor complication included seroma, clinical signs of infection, asymmetry, displacement of the implant, pain greater than three months, hypertrophic scarring, abdominal bulging/hernia, limited necrosis of the breast and delayed wound healing which was defined as prolonged healing time requiring dressing changes assisted by health personnel.
Major complications comprised necrosis of most of the flap, total flap loss, surgical evacuated hematoma, implant rupture, skin perforation or necrosis leading to implant loss and capsular contracture.
A study specific questionnaire was developed based on questionnaires previously used to asses surgical procedures of the breast, the EORTC QOL BR-23 and the SF-36, supplemented with questions regarding demographics and the outcome of the breast reconstruction [Citation16–24].
This questionnaire was tested with 20 BR women outside the cohort to assess layout and uniformity of questions. The questionnaire was then mailed to the 363 women included in the study. The non-responders were mailed one reminder, as no telephone calls were allowed by the ethical committee in Denmark. The Danish questionnaire is assessable in the online version of the journal.
During the follow-up visit, standardized photographs were taken of each patient at the Department of Clinical Photo, Aarhus University Hospital. The overall aesthetic result of the breast and the color of the flap were scored in four categories; excellent, good, fair, poor. Categorization of the RT induced subcutaneous fibrosis, telangiectasia and pigmentation changes was inspired by Johansen et al., who examined the impact of surgery and adjuvant treatment on the cosmetic outcome of breast-conserving treatment [Citation25]. The degree of capsular formation around the implant was classified according to the Baker classification [Citation26].
The donor site was examined for abdominal laxity, defined as visual bulging of the lower abdomen. As part of the abdominal examination, patients attempted to perform sit-ups using mainly the rectus or oblique muscles. Further, the ability to sit up and stand up from a supine position without using upper limbs was tested.
The women participating in the follow-up visit were examined by the same investigator.
The study followed the Helsinki Declaration and was approved by the Danish Regional Committee on Biomedical Research Ethics, M-20070039. All patients gave their written informed consent.
Statistical considerations
Descriptive statistics were used to compare patient subgroups, including median, 95% confidence interval (CI) and the two-sided Fisher exact test. Missing values were coded as missing and omitted from the analysis. Logistic regression was used to compare the satisfaction level between the groups, adjusting for radiation therapy, age, time since reconstruction, BMI and tobacco use. Comparisons are reported as odds ratios (OR). The women's answers in the questionnaire were dichotomized as pleased or not pleased. The purpose of this dichotomous categorization was to gather several answers into a new variable, thus extracting the essence of the satisfaction level from the questionnaire. The new variable, termed “excellent breast”, was based on several answers to the questionnaire. Only if all of these answers were recorded as “pleased” were they then considered under the new variable “excellent breast”. The questions included in the new variable were breast shape, breast size, softness of the breast, overall satisfaction with the reconstruction and the fulfilment of expectations to the reconstruction. Logistic regression was used to compare the “excellent breast” among the groups.
Statistical analysis was performed using the STATA® software IC10 (Stata Corporation, College Station, USA).
Results
Demographics
In the current study, 363 women were included; the 206 were reconstructed with an implant and 10 bilateral. The 119 were expander implants and 87 were fixed sized implants consisting of a silicone cohesive gel with a rough surface. Thirty-four women were reconstructed with an LD flap of which three had an implant. A total of 123 women were reconstructed with the TRAM flap; of these 44/123 (39%) had their abdomen reinforced with an on-lay mesh. Of the 363 women 14 had undergone a sentinel node procedure and 218 had their axillary lymph nodes removed.
A total of 263 women of the 363 included (73%) answered the questionnaire; of them, 180 also participated in the clinical follow-up visit. summarizes the study populations’ procedure distribution along with the demographic characteristics.
Table I. Patient demographics for women reconstructed with an implant, an LD flap or a TRAM flap at the time of reconstruction.
The 363 women reconstructed with the three techniques were comparable with a median age at reconstruction of 49 in the implant group, 51 years in the LD flap group and 51 years in the TRAM flap group. Of the 263 women answering the questionnaire, the women with an implant reconstruction were significantly younger (p = 0.01), when compared with the women reconstructed with autologous tissue. There was no significant age difference between the three groups at the follow-up visit (p = 0.5).
Information about smoking was missing for 35/206 (17%) women reconstructed with an implant, 2/34 (6%) with a LD flap and 14/123 (11%) for women reconstructed with a TRAM flap.
A BMI below 25 was defined as normal weight. Of the 363 patients, significantly more of the women reconstructed with autolgous tissue had a BMI >25 (p = 0.001).
The 180 women participating in the follow-up visit were very similar regarding weight (p = 0.12). Among the 363 women, there was a significant over representation of known active smokers in the implant group, compared to the women reconstructed with autologous tissue, (p < 0.0001) while previous radiation therapy was more frequent for women reconstructed with autologous tissue (p < 0.0001).
The weight change from the time of reconstruction to the follow-up visit was divided into three, 1–5 kg, 6–10 kg and 11–20 kg. Logistic regression was used to assess the influence of the weight change upon the overall satisfaction with the breast reconstruction among the groups. A weight gain of less than 5 kg did not significantly change the overall satisfaction with the reconstruction, but a weight gain of more than 5 kg did influence the satisfaction negatively (OR = 0.38, p = 0.06 (CI: 0.14; 1.02)).
The median time since the breast reconstruction was seven years (range 3.3–16.8). The women were separated into two subgroups, dependent upon whether their breast reconstruction was performed more than or less than seven years ago. More women reconstructed with implants were reconstructed over seven years ago (p = 0.01).
A review of the charts of the 263 women responding to the questionnaire showed no significant difference between the reconstructive methods regarding minor complications of the breast (p = 0.30). Nor was there any difference in the incidence of major complications between the implant group and the TRAM flap group (p = 0.84). The LD flap group had no major complications ().
Of the 206 women reconstructed with an implant, 48 women had their implant exchanged for a new one.
Logistic regression was used to assess the influence of RT, tobacco and BMI on the complications among the groups. Active smokers reconstructed with an implant had an increased risk of complications (OR = 2.61, p = 0.01 (CI: 1.29; 5.27)). Overweight women reconstructed with a TRAM flap had an increased risk of complications (OR = 3.08, p = 0.01 (CI: 1.29; 7.33)), while women reconstructed with an implant did not (OR = 1.05, p = 0.89 (CI: 0.49, 2.29)). RT increased the risk of the assembled complications for women reconstructed with an implant (OR = 2.53, p = 0.02 (CI: 1.18; 5.40)) while for women reconstructed with a TRAM flap, the RT increased the risk of major complications (OR = 5.1,
Questionnaire
summarizes data from the questionnaire. The results revealed that women with autologous tissue reconstructions were generally more pleased with their reconstruction (p = 0.002). They answered more positively to questions regarding their BR. There was no difference among the groups regarding their self reported overall health.
Table II. Data from questionnaire.
Logistic regression was used to assess the effect of procedure type on the 263 women's opinion, while controlling for the women's age at reconstruction, radiation therapy, tobacco use, time since reconstruction and BMI. The type of breast reconstruction procedure had a statistically significant impact on the “excellent breast” parameter and therefore on the patient's own rating of the BR. Women with an LD flap (OR = 3.71, p = 0.003 (CI: 1.57; 8.75)) or a TRAM flap (OR = 7.71, p < 0.0001 (CI: 4.35; 13.65)) were significantly more pleased than women reconstructed with an implant.
Recipients of an LD flap rated their breast shape (OR = 4.41, p = 0.003 (CI: 1.63; 11.92)) and the softness of the breast (OR = 6.47, p = 0.001 (CI: 2.20; 19.00)) significantly higher than did the women reconstructed with implants. Women reconstructed with a TRAM flap also rated their breast shape (OR = 6.22 p < 0.0001 (CI 3.25; 11.90)), breast size (OR = 3.94, p < 0.0001 (CI: 2.03; 7.63)) and the softness of the breast (OR = 24.73, p = 0.001 (CI: 9.83; 62.27) significantly higher than did women with an LD flap or an implant.
Radiation therapy (OR = 0.49, p = 0.03 (CI: 0.25; 0.94)) and tobacco use at the time of the reconstruction (OR = 0.38, p = 0.003 (CI: 0.20; 0.71)) had a negative influence on how pleased the patient was with breast size, according to the questionnaire. Smoking and RT did not influence the women's opinion of breast shape or the feel of the breast.
Objective assessment
At the follow-up visit (), women reconstructed with autologous tissue had a superior objective overall result (p < 0.0001) and a higher degree of symmetry between the breasts compared to the women reconstructed with an implant. The radiation treatment influenced the overall result negatively (OR = 0.41, p = 0.03 (CI: 0.2; 0.93)). Pigmentation changes, fibrosis, telangiectasia and less sensitivity of the skin were more frequent for the women reconstructed with autologous tissue. A pigmentation alteration was found on 50% of women reconstructed with a TRAM flap while it was 13% on women reconstructed with an implant (). The women without surgery involving the abdomen were not more able to perform sit-ups or rise from a supine position without using their upper limbs.
Table III. Data from follow-up visit.
Baker III-IV () was found in 34% (29/85) of the women reconstructed with an implant. Capsular contracture was found more frequently (48% (11/23)), although not statistically significant, in women previously treated with RT (p = 0.3).
Table IV. Complications after the first reconstructive procedure from the patient chart.
There are several reasons for choosing a BR. The most common reasons listed in the questionnaires were often related to trouble with the external prosthesis, for example with clothing, problems during warm summers and with physical activities, an asymmetry problem with a large and heavy opposite breast, feelings of not being whole and the daily reminder of cancer. A substantial number of the women stated that the need to feel whole was their main reason for having a BR.
The women reconstructed with autologous tissue generally answered more positively in the questionnaire and they also had an overall objectively superior result. RT influenced the objective result negatively. There was no difference in the number of minor complications among the different procedure types. The incidence of necrosis requiring surgery was higher in women treated with RT and autologous tissue. Furthermore they had increased pigmentation changes and telangiectasia compared to women reconstructed with an implant. The women reconstructed with an LD flap had no major complications or necrosis requiring revisional surgery.
Discussion
This study describes, with a median follow-up time of seven years, the outcome of 263 breast cancer patients who underwent BR at our institution between 1990 and 2005.
In a Danish retrospective study of immediate BR with an implant, Strålman et al. [Citation27] reported a capsular contracture rate of 17%. The mean follow-up time was 34 months. According to the Danish Registry for Plastic Surgery of the Breast, more recent data reports a capsular contracture rate of 9.6% within 10 years [Citation28]. At the follow-up visit, 34% had developed a capsular contracture. The degree of capsule was rarely graded in the patient charts. It was often described in words or just mentioned to exist. And consequently, the number of registered complications for reconstruction with an implant may be under-reported. Furthermore implant exchange procedures are done at private hospitals and thus we have no knowledge of the reasons for the renewal. Minor complications and donor site morbidity were in agreement with the numbers reported in the literature [Citation6,Citation29,Citation30].
There is generally an agreement that RT after the BR increases complications and yields a worse outcome, while RT before the reconstruction is subject to debate [Citation5–7,Citation31,Citation32].
We expected that more women previously treated with RT suffered complications, especially among the women reconstructed with an implant. The data from the patient charts confirmed our hypothesis of a higher risk of complications after RT for women reconstructed with an implant. The incidence of severe necrosis negatively influenced the objective result of the TRAM flap reconstruction even years later. The late RT sequelae, such as hyper/hypo pigmentation, subcutaneous fibrosis and telangiectasia detected at the follow-up visit, were more frequent in women reconstructed with autologous tissue (). This might be explained by pre-operative patient selection, although the possible progression of the late sequelae should also be considered.
More than 80% of the women reconstructed with autologous tissue were pleased with the overall result of their BR, compared to 64% of the women with an implant.
In a prospective study of implant, free and pedicled TRAM flap reconstructions Alderman et al. report no immediate objective difference in trunk function among women reconstructed with the free or the pedicled TRAM flap, while they report a long-term deficit in trunk function for women with both the free and the pedicled TRAM flap reconstructions [Citation33]. We did not find any difference in the ability to rise from a supine position among women reconstructed with the different methods, while their ability to perform sit-ups was significantly different. None of the above movements are performed often in daily life, and thus rises the question of what measures should be used to test the influence of donor sites upon daily life. It is a difficult task to differentiate among the multiple different reasons for lower back pain and we did not attempt this. To our knowledge there are no reports about the pedicled TRAM flap should give rise to lower back pain.
The question of how much the donor site sequelae actually influence the daily life of the reconstructed women is relevant to the evolution of reconstruction techniques. Perhaps the different methods to spare abdominal muscle do not result in a major difference in the daily life of the individual women. This could be further examined in a randomized study between pedicled and free TRAM/DIEP flaps. A randomization between more reconstructive procedures as implants or the LD flap would not be ethical.
Today more institutions have the setup and expertise necessary for microsurgical reconstructions which spare the abdominal muscle. They are however often lengthy, costly and may be subject to anatomical variations. The pedicled TRAM flap and the LD flap reconstructions are still good reliable techniques for autologous breast reconstructions.
In conclusion, the majority of the women answering the questionnaire were pleased with their reconstruction after a median of seven years. We found that most of the women had an objective, good overall result of their BR. The incidence of complications did not differ much among the different types of reconstructions. Appropriate considerations should be taken to the opposite breast size, smoking status, BMI and to previous RT. Data from the northern and mid Danish regions indicate that a unilateral BR with autologous tissue, both satisfies more women with the result, and yields an objectively superior result.
http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2011.584554
Download PDF (257.7 KB)Acknowledgements
The authors would like to thank the following for their financial support. None of the foundations had any involvement in the study. The study was financially funded by the Faculty of Health Sciences, Aarhus University, “Snedkermester Sophus Jacobsen og hustru Astrid Jacobsens Fond” and The Danish Cancer Society.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Glat P, Longaker MT, Maxwell GP, Hammond DC. Grabb and Smith's plastic surgery. 5th. Philadelphia: Lippincott-Raven; 1997.
- Saint-Cyr M, Rios JL. Breast. Janis JE. Essential of plastic surgery. 1st. St. Louis: Quality Medical Publishing Inc.; 2007. 365–422.
- Krueger EA, Wilkins EG, Strawderman M, Cederna P, Goldfarb S, Vicini FA, . Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys 2001;49:713–21.
- Chawla AK, Kachnic LA, Taghian AG, Niemierko A, Zapton DT, Powell SN. Radiotherapy and breast reconstruction: Complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys 2002;54: 520–6.
- Bristol SG, Lennox PA, Clugston PA. A comparison of ipsilateral pedicled TRAM flap with and without previous irradiation. Ann Plast Surg 2006;56:589–92.
- Spear SL, Ducic I, Low M, Cuoco F. The effect of radiation on pedicled TRAM flap breast reconstruction: Outcomes and implications. Plast Reconstr Surg 2005;115:84–95.
- Carlson GW, Page AL, Peters K, Ashinoff R, Schaefer T, Losken A. Effects of radiation therapy on pedicled transverse rectus abdominis myocutaneous flap breast reconstruction. Ann Plast Surg 2008;60:568–72.
- Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: Two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002;109:2265–74.
- Williams JK, Bostwick J, III, Bried JT, Mackay G, Landry J, Benton J. TRAM flap breast reconstruction after radiation treatment. Ann Surg 1995;221:756–64.
- Lin KY, Johns FR, Gibson J, Long M, Drake DB, Moore MM. An outcome study of breast reconstruction: Presurgical identification of risk factors for complications. Ann Surg Oncol 2001;8:586–91.
- Tran NV, Evans GR, Kroll SS, Baldwin BJ, Miller MJ, Reece GP, . Postoperative adjuvant irradiation: Effects on tranverse rectus abdominis muscle flap breast reconstruction. Plast Reconstr Surg 2000;106:313–7.
- Schneider WJ, Hill HL, Jr., Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg 1977;30:277–81.
- Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg 1982;69:216–25.
- Kuokkanen H, Holmstrom H, Åbyholm F, Drzewiecki K. Scandinavian Plastic Surgery. 1st. 2008.
- Overgaard M, Christensen JJ. Postoperative radiotherapy in DBCG during 30 years. Techniques, indications and clinical radiobiological experience. Acta Oncol 2008;47:639–53.
- Alderman AK, Wilkins EG, Lowery JC, Kim M, Davis JA. Determinants of patient satisfaction in postmastectomy breast reconstruction. Plast Reconstr Surg 2000;106: 769–76.
- Andrade WN, Baxter N, Semple JL. Clinical determinants of patient satisfaction with breast reconstruction. Plast Reconstr Surg 2001;107:46–54.
- Bonde C. Breast reconstruction using autologous tissue, current status and perspectives. 2006. The dep of plastic surgery and burns unit Copenhagen University Hospital, rigshospitalet.
- Brandberg Y, Malm M, Blomqvist L. A prospective and randomized study, “SVEA,” comparing effects of three methods for delayed breast reconstruction on quality of life, patient-defined problem areas of life, and cosmetic result. Plast Reconstr Surg 2000;105:66–74.
- Ching S, Thoma A, McCabe RE, Antony MM. Measuring outcomes in aesthetic surgery: A comprehensive review of the literature. Plast Reconstr Surg 2003;111:469–80.
- Edsander-Nord A, Brandberg Y, Wickman M. Quality of life, patients’ satisfaction, and aesthetic outcome after pedicled or free TRAM flap breast surgery. Plast Reconstr Surg 2001;107:1142–53.
- Henriksen TF, Holmich LR, Friis S, McLaughlin JK, Fryzek JP, Pernille HA, . The Danish Registry for Plastic Surgery of the Breast: Establishment of a nationwide registry for prospective follow-up, quality assessment, and investigation of breast surgery. Plast Reconstr Surg 2003;111:2182–9.
- Mizgala CL, Hartrampf CR, Jr., Bennett GK. Assessment of the abdominal wall after pedicled TRAM flap surgery: 5- to 7-year follow-up of 150 consecutive patients. Plast Reconstr Surg 1994;93:988–1002.
- Sacchini V, Luini A, Tana S, Lozza L, Galimberti V, Merson M, . Quantitative and qualitative cosmetic evaluation after conservative treatment for breast cancer. Eur J Cancer 1991;27:1395–400.
- Johansen J, Overgaard J, Rose C, Engelholm SA, Gadeberg CC, Kjaer M, . Cosmetic outcome and breast morbidity in breast-conserving treatment – results from the Danish DBCG-82TM national randomized trial in breast cancer. Acta Oncol 2002;41:369–80.
- Spear SL, Baker JL, Jr. Classification of capsular contracture after prosthetic breast reconstruction. Plast Reconstr Surg 1995;96:1119–23.
- Stralman K, Mollerup CL, Kristoffersen US, Elberg JJ. Long-term outcome after mastectomy with immediate breast reconstruction. Acta Oncol 2008;47:704–8.
- Dansk Plastikkirurgisk Mammaregister. Plastic Surgery. 2006. The Danish registry for plastic surgery of the breast. www.mammaregisteret.dk
- Ascherman JA, Seruya M, Bartsich SA. Abdominal wall morbidity following unilateral and bilateral breast reconstruction with pedicled TRAM flaps: An outcomes analysis of 117 consecutive patients. Plast Reconstr Surg 2008;121:1–8.
- Ducic I, Spear SL, Cuoco F, Hannan C. Safety and risk factors for breast reconstruction with pedicled transverse rectus abdominis musculocutaneous flaps: A 10-year analysis. Ann Plast Surg 2005;55:559–64.
- Albino FP, Koltz PF, Ling MN, Langstein HN. Irradiated autologous breast reconstructions: Effects of patient factors and treatment variables. Plast Reconstr Surg 2010;126:12–6.
- Tran NV, Chang DW, Gupta A, Kroll SS, Robb GL. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg 2001;108:78–82.
- Alderman AK, Kuzon WM, Jr., Wilkins EG. A two-year prospective analysis of trunk function in TRAM breast reconstructions. Plast Reconstr Surg 2006;117:2131–8.