Abstract
Background. Patients with head and neck squamous cell carcinoma (HNSCC) and a low level of hemoglobin often have a poor response to radiation that may be related to hypoxia-induced radioresistance. We have previously published the importance of hemoglobin level and the effect of transfusion by the results from the randomized DAHANCA 5 trial, including 414 patients in the analysis. Aim of the current analysis was to gain additional power by adding patients from the continued subrandomization in the DAHANCA 7 trial, now including a total of almost 1200 patients. Material and methods. Patients were randomized to treatment in the DAHANCA 5 and 7 study (nimorazole vs. placebo and five fx/week vs. six fx/week), and in addition, patients with “low” pre-irradiation hemoglobin values (females <13 g/dl; males <14.5 g/dl) were subrandomized to plus or minus transfusion. Transfusion was given with packed red blood cells with the aim to achieve a hemoglobin level in the “high” value range. Results. A total of 1166 patients were included, 701 patients had high hemoglobin levels and 465 had low hemoglobin levels. Among the low hemoglobin patients, 235 were randomized to receive transfusion. Patient characteristics and treatment arms were well balanced. In the majority of patients, transfusion resulted in increased hemoglobin levels although this decreased slightly throughout treatment as in the non-transfused patients. Overall, the patients with low hemoglobin level had a significant reduced probability of locoregional control, disease-specific and overall survival. In the low hemoglobin group, transfusion did not improve the outcome in locoregional control, disease-specific or overall survival. In multivariate analyses, HPV/p16 status, T and N classification were significant factors for all outcome measures, whereas there was no significant influence of transfusion or hemoglobin level on endpoints. Conclusion. Transfusion prior to and during radiation treatment did not improve the outcome in patients with HNSCC and low hemoglobin values, but may have a negative impact on survival.
In a recent publication from the Danish Head and Neck Cancer Group (DAHANCA), the hemoglobin level and transfusion results from the randomized DAHANCA 5 trial has been described [Citation1]. That study showed a prognostic significance of high hemoglobin level in patients with HNSCC (head and neck squamous cell carcinomas) treated with radiotherapy (RT). However, transfusion prior to and during treatment did not improve the outcome in patients with low hemoglobin values. Since the DAHANCA 5 study lacked power to draw final conclusions regarding the effect of transfusion, this subrandomization was continued in the DAHANCA 7 protocol [Citation2]. The purpose of the present analysis is a combined analysis of DAHANCA 5 and DAHANCA 7 results to add knowledge to the conclusions regarding transfusion prior to and during treatment in HNSCC patients with low hemoglobin values. The overall hypothesis was that in head and neck cancer patients with low hemoglobin level, an increase in hemoglobin level by transfusion may improve the effect of radiotherapy.
The background for the hypothesis is that HNSCC patients with a low level of hemoglobin often have a poor response when treated with radiation [Citation3–6]. A relationship between hemoglobin level and hypoxia has been shown both experimentally and clinically, but the mechanisms linking these conditions are uncertain [Citation6–10]. Head and neck tumors often present hypoxic radioresistant cells and are heterogeneous as a group [Citation11,Citation12]. Radiosensitivity has been regained in tumor-bearing anemic mice by giving transfusions [Citation13–16] and a correction of anemia in clinical studies has resulted in improvement in tumor oxygenation and a subsequent increase in the therapeutic efficacy of irradiation [Citation4,Citation17–25]. The adverse effects and outcome in this setting when administrating erythropoietin stimulating agents (ESA) [Citation26–32], has reopened the possible advantage of using transfusion to raise hemoglobin levels before and during treatment.
Methods
Patients and treatment
As part of two randomized trials, DAHANCA 5 & 7 evaluating the role of nimorazole as a hypoxic radiosensitizer and accelerated fractionated RT, respectively, the data to evaluate the importance of hemoglobin level in patients and the modification with transfusion were collected. The protocols have previously been described [Citation2,Citation33–35] and the current evaluation is almost identical to what was done in the previous DAHANCA 5 hemoglobin publication [Citation1].
Patients were prior to randomization stratified according to sex, institution, tumor site, tumor stage and hemoglobin concentration. In DAHANCA 5, the patients were randomized to radiotherapy with nimorazole or placebo, in DAHANCA 7 to nimorazole treatment and radiotherapy with five or six fractions/week. Patients with low pre-irradiation hemoglobin (females <13.0 g/dl; males <14.5 g/dl) were offered subrandomization to receive or not to receive transfusion. Transfusions were given with packed blood cells (one unit approximately equivalent to 500 ml full blood, leukocyte depletion of the units was not standard) to achieve a hemoglobin concentration in the “high” value range. Transfusion was given before radiotherapy and if during treatment the hemoglobin fell below the values indicated above, the transfusion was repeated. The hemoglobin level was measured at least every two weeks.
Treatment was given according to DAHANCA and protocol guidelines as previously described [Citation2,Citation33–35]. Both studies were performed in accordance with the Helsinki declaration and approved by relevant ethics committees. All patients gave written informed consent [Citation2,Citation33–35].
Statistical analyses
The endpoints used were locoregional control after radiotherapy, disease-specific survival and overall survival. Locoregional control was defined as complete and persistent disappearance of the disease in the primary tumor (T-site) and regional lymph nodes (N-site) after radiotherapy. The evaluation was done by clinical examination and supplemented with relevant tests in case of doubt. Failure was recorded in case of recurrent tumor, or if the primary tumor never completely disappeared. In the latter situation, the tumor was then assumed to have failed at the time of randomization. The endpoint did not include the effect of a successful procedure with salvage surgery. The definition of disease-specific survival was death from or with the actual cancer. The endpoint for overall survival was any death, irrespective of cause. All time estimates were done using the date of randomization as the initial value. Follow-up was completed in connection with the original study [Citation2,Citation33–35].
The treatment effect was evaluated using the intention to treat principle and patients were included in their randomization group irrespective of whether or not they had completed the planned treatment. Time for evaluation of locoregional control, disease-specific survival and overall survival was five years after randomization, since patients were followed regularly only for that period [Citation1].
Patients with high hemoglobin (high) and patients with low hemoglobin, regardless of transfusion status (low all), were compared to determine the effect of hemoglobin level. In addition to this, a comparison between high and low patients without transfusion (low-t) has been done. The effect of transfusion was evaluated by comparing the two low groups with and without transfusion (low+t, low+t), respectively. Patients were defined as having received transfusion during treatment if they received a transfusion in a period of 4–45 days after start of radiotherapy. This subgroup of patients does not include patients receiving transfusion prior to and during the first few days of radiotherapy.
Positive HPV/p16 status was defined retrospectively by positive p16 staining in tumors and compared to tumors with negative staining or unknown status and included due to the positive effect on the outcome of radiotherapy treatment [Citation36,Citation37].
Statistical analyses were done using the STATA 11 software package. Patient characteristics were compared with χ2-test and a two-sided significance level was chosen at 0.05. The actuarial values of end-points were evaluated by the Kaplan-Meier plots and compared with the log-rank test for equality of survivor functions. The p-values estimated are those for a two tailed test and the significance level was chosen to be 5%. A multivariate Cox proportional hazards analysis was used to evaluate prognostic factors and treatment with respect to the risk of locoregional failure, disease-specific survival and overall survival. Variables included in the model were selected prior to analysis and included age, gender, site, p16 status, T-classification, N-classification, treatment, protocol, hemoglobin level and transfusion. Data are presented as five-year actuarial hazard ratios (HR) with 95% confidence intervals, unless otherwise mentioned.
The randomized studies were not dimensioned in regard to the present transfusion analysis, but with 230 events in each of the low groups and an expected locoregional control of 70%, we expected to be able to detect a difference of 15% with alpha 0.05 and a power of 0.9.
All diagnostic, therapeutic, and follow-up data were validated and processed by the DAHANCA data centre.
Results
A total of 1200 patients were eligible; 414/1200 (34.5%) from the DAHANCA 5 and 786/1200 (65.5%) from the DAHANCA 7 study. Of the 1200 patients, 708/1200 (59%) were in the high hemoglobin group and 492/1200 (41%) in the low hemoglobin group. Twenty-six were not randomized to transfusion and therefore excluded from the analysis. Further, eight patients were excluded for having their initial hemoglobin value in the wrong strata. The final analysis included 1166/1200 (97%) patients; 230/1166 (20%) in the low hemoglobin without transfusion (low+t) group, 235/1166 (20%) in the low plus transfusion (low+t) group and 701/1166 (60%) in the high hemoglobin (high) group ( and ).
Table I. Patient and tumor characteristics.
Statistically significant differences were found between the high and low hemoglobin groups (high and low all) regarding age, gender, site, T- and N-classification and stage (), i.e. high hemoglobin was associated with more favorable prognostic factors.
Compliance to radiotherapy was high and in both studies, 97% of patients completed the planned radiation treatment [Citation2,Citation33].
Pretreatment hemoglobin was in the low level for 465/1166 (40%) patients; 75/1166 (6%) females and 390/1166 (33%) males. These patients were randomized to transfusion (235/465, 51%) or no transfusion (230/465, 49%). The group given transfusion consisted of 40/235 (17%) females and 195/235 (83%) males.
There was no difference in the distribution of hemoglobin levels in the transfused and non-transfused group prior to treatment, nor were there any significant differences in distribution of patient and tumor characteristics between the two groups (low+t and low+t) before treatment ().
The patients randomized to transfusion received 0–14 units (median two units) of blood. Very few patients received more than eight units and 95/235 (40%) patients received two units of blood (Appendix 1 to be found online at http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2011.592650).
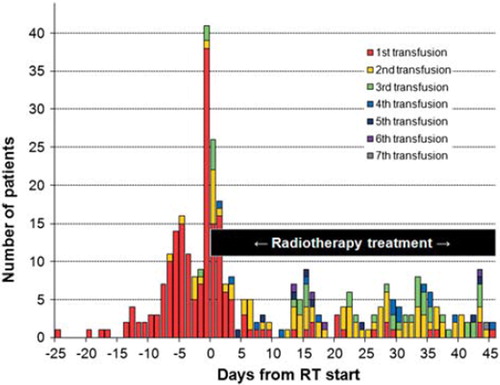
A total of 210/235 (89%) received transfusion on at least one occasion, 87/235 (37%) at two occasions and 41/235 (17%) at three or more occasions (). Transfusion was never received despite randomization in 25/235 (11%) patients.
Most patients 142/235 (60%) received their first transfusion before or on the day of the first radiation fraction; 174/235 (74%) before or within the first week of radiotherapy (). Transfusions were with few exceptions given as two units of packed red blood cells.
In patients randomized to transfusion, the first transfusion was on median given one day (range −25–40 days) before start of radiotherapy. In patients receiving their first transfusion prior to radiotherapy, this happened on median four days (range −25–0 days) before start of radiotherapy ().
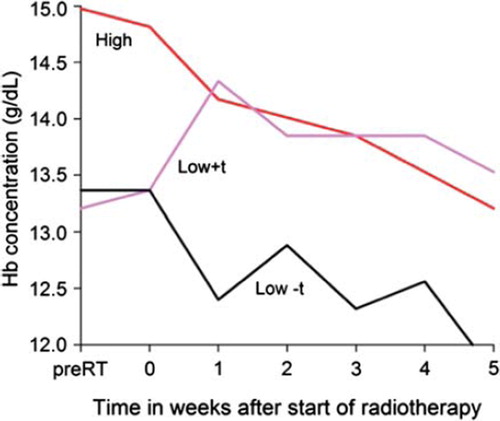
The benefit of transfusion is seen in : Measurements of hemoglobin level during radiotherapy showed that the median value increased within the first week in the transfused group. The median hemoglobin level was raised to the same level as the high hemoglobin group. However, after this increase there was a continuous drop throughout the course of radiotherapy for all hemoglobin groups, low+t, high and low+t, respectively ( and Appendix 2 to be found online at http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2011.592650). Only 4/40 (10%) females and 76/195 (39%) males had low hemoglobin level after treatment. No cases of venous thromboembolism were found in connection to treatment with transfusion.
Of the 1166 evaluable patients a total of 549 (47%) experienced locoregional failure; 517 (44%) had died of disease and 745 (64%) had died overall ( and Appendix 3 to be found online at http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2011.592650).
Distant metastases was experienced in 117/1166 (10%) patients. Twenty three (10%) failures in the low+t group, 31 (13%) in the low+t group and 63 (9%) in the high group, respectively. However, only 48/1166 (4%) patients experienced an isolated distant failure, with 6/230 (3%) low+t, 15/235 (6%) low+t and 27/701 (4%) high events in the three groups.
Univariate analysis showed statistical significance of low age on overall survival. Female gender, supraglottic location, positive HPV/p16 status, low T-classification, low N-classification and low stage were statistically significant for locoregional control, disease-specific survival and overall survival. When analyzing the treatment groups there was a significant benefit of adding nimorazole to the regimen for both locoregional control and disease-specific survival. There were no differences in outcome measurements when going from the DAHANCA 5 to the DAHANCA 7 protocol. The addition of accelerated radiotherapy did not reach statistical significance, but a tendency towards better outcome measurements was seen.
High hemoglobin level was statistically significant better than low hemoglobin level for locoregional control (HR 0.83; CI 0.70–0.98; p = 0.03), disease-specific (HR 0.77; CI 0.64–0.91; p = 0.003) and overall survival (HR 0.77; CI 0.67–0.89; p = 0.0004). However, analysis of the three hemoglobin groups showed no statistically significant difference between the two non-transfused groups (high vs. low+t) on outcome measurements. No benefit of transfusion (low+t vs. low−t) was observed on locoregional control (HR 1.06; 0.82–1.38; p = 0.7), disease-specific (HR 1.27; CI 0.97–1.65; p = 0.1) or overall survival (HR 1.24; CI 0.99–1.54; p = 0.08) ( and , and ).
Figure 4. Locoregional control (a), disease-specific (b) and overall survival (c) probability curves (Kaplan-Meier method) according to hemoglobin group.
Table II. Univariate and multivariate analysis.
When looking only at the patients randomized to transfusion, transfusion during treatment did not turn out significant for survival measurements when comparing with patients not receiving transfusions during treatment; locoregional control (HR 1.14; CI 0.78–1.67; p = 0.5), disease-specific survival (HR 1.35; CI 0.94–1.95; p = 0.1) and overall survival (HR 1.18; CI 0.86–1.61; p = 0.3). However, this subgroup of patients tends to have a worse prognosis than patients not receiving transfusions during radiotherapy.
The patients received four different treatments defined by their original DAHANCA study, placebo vs. nimorazole and five fx/week vs. six fx/week. In the subgroup analysis it is shown that hemoglobin level is of importance irrespective of hypoxic modification with nimorazole and fractionation schedule (Appendix 3 to be found online at http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2011.592650).
Multivariate Cox proportional hazards analysis confirmed the statistical significance of low age on overall survival. For locoregional control, disease-specific and overall survival, the statistical significant prognostic effect of positive HPV/p16 status, supraglottic location, low T-classification and low N-classification was also confirmed. The addition of nimorazole and accelerated radiotherapy to treatment protocol was significant for locoregional control when using patients from DAHANCA 5 treated with nimorazole and five fx/week as reference group ().
High hemoglobin level was statistically significant for overall survival, but no positive effect of transfusion was seen on outcome measurements ().
Transfusion during radiotherapy was evaluated in a separate model and patients receiving transfusions during radiotherapy had a statistically significant worse prognosis in disease-specific and overall survival than patients not receiving transfusions during radiotherapy when correcting for other relevant factors (Appendix 4).
Discussion
In squamous cell head and neck cancer patients with a low hemoglobin level; transfusion was able to raise the hemoglobin level during radiotherapy, however this increase in hemoglobin level was not able to improve the effect of the radiotherapy treatment. This is in accordance with what was shown in the analysis of the DAHANCA 5 study [Citation1]. The addition of the DAHANCA 7 patients and the total number of almost 1200 patients gives stronger evidence, that transfusion is unable to improve the effect of radiotherapy, but instead, in survival outcome measurements, showing a tendency towards worsening the prognosis.
The tendency to worsening the prognosis when receiving transfusion during radiotherapy could be explained by patients with low hemoglobin levels during treatment, having a worse overall condition and is not necessarily a cancer related transfusion risk.
The known poor prognostic effect of low hemoglobin prior to radiotherapy treatment was confirmed for overall survival in multivariate analysis [Citation6]. This difference in outcome was, however not found when analyzing only the non-transfused patients and comparing the low non-transfused group and the high hemoglobin group. The addition of the low hemoglobin patients receiving transfusion reduced outcome measurements, since these patients have the worst probability for locoregional control, disease-specific and overall survival.
The prognostic effect of low hemoglobin prior to radiotherapy treatment was more pronounced with overall survival as endpoint than with disease-specific survival and locoregional control. This indicates that there may other factors related to hemoglobin level, e.g. comorbidity and overall condition, influencing the prognosis. Work at clarifying the importance of comorbidity in head and neck cancers is currently being done [Citation38].
In addition to what was shown in the DAHANCA 5 analysis, the transfused patients follow the same hemoglobin level pattern as the non-transfused patients throughout the course of radiotherapy. The low patients are by transfusion shifted into the high level, but all groups decrease during treatment. There could be a benefit if this drop was avoided by using erythropoietin stimulation agents, but studies published so far are not encouraging [Citation26–32].
The fact that transfusion have been shown to lower the immune system in patients with kidney transplants may also relate to the poor survival in transfused cancer patients. The immune system have functions towards the growing cancer, these not fully evaluated, but existing. The beneficial effect of blood transfusions prior to transplantation on graft survival is used. However, in cancer patients this immune regulatory effect may be all but beneficial. It has been shown that allogenic transfusions might affect the overall survival in patients undergoing curative cancer surgery [Citation39]. In a study involving colorectal cancer blood transfusion was shown to be a univariate prognostic negative factor, but when adjusting with well-established prognostic factors in a multivariate prognostic model the negative effect of transfusions disappeared [Citation40].
Even when accomplishing the wanted effect of transfusion by giving the patients the same start values as the high hemoglobin patients, the mechanisms are more complex than just high and low hemoglobin values, and more is needed than “just” raising hemoglobin level by transfusion and probably ESAs. Development of a hypoxia profile, which will be able to single out patients in need of hypoxic modification and offer a more individualized treatment, is ongoing.
There are limitations to the analysis and conclusions drawn from this study, especially in reference to explaining the connection between hypoxia, low hemoglobin levels and transfusion.
We can however conclude that in a large patient material with squamous cell head and neck cancer with a low hemoglobin level; transfusion were able to raise the hemoglobin level during radiotherapy, however this increase in hemoglobin level were not able to improve the effect of the radiotherapy treatment.
Supplementary material available online at http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2011.592650.
Appendix 1. Units of blood.
Appendix 2. Hemoglobin level during RT treatment
Blue = males
Red = females
Showing median Hb level during radiotherapy as a function of hemoglobin group.
Appendix 3. Subgroup analysis by treatment group in the original DAHANCA 5 and 7 trials.
Appendix 4. Multivariate model including transfusion during RT variable.
Supplementary Material
Download PDF (235.5 KB)Acknowledgements
Supported by CIRRO – The Lundbeck Foundation Center for Interventional Research in Radiation Oncology, the Danish Council for Strategic Research and The Danish Cancer Society. No conflicts of interest declared by the authors.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Hoff CM, Hansen HS, Overgaard M, Grau C, Johansen J, Bentzen J, . The importance of haemoglobin level and effect of transfusion in HNSCC patients treated with radiotherapy – results from the randomized DAHANCA 5 study. Radiother Oncol 2011;98:28–33.
- Overgaard J, Hansen HS, Specht L, Overgaard M, Grau C, Andersen E, . Five compared with six fractions per week of conventional radiotherapy of squamous-cell carcinoma of head and neck: DAHANCA 6 and 7 randomised controlled trial. Lancet 2003;362:933–40.
- Overgaard J, Hansen HS, Jorgensen K, Hjelm HM. Primary radiotherapy of larynx and pharynx carcinoma – an analysis of some factors influencing local control and survival. Int J Radiat Oncol Biol Phys 1986;12:515–21.
- Overgaard J. Sensitization of hypoxic tumour cells – clinical experience. Int J Radiat Biol 1989;56:801–11.
- Grau C, Overgaard J. Significance of hemoglobin concentration for treatment outcome. Molls M, Vaupel P. Blood perfusion and microenvironment of human tumors, implications for clinical radiooncology. Berlin: Springer; 1998. 101–12.
- Nordsmark M, Overgaard J. Tumor hypoxia is independent of hemoglobin and prognostic for loco-regional tumor control after primary radiotherapy in advanced head and neck cancer. Acta Oncol 2004;43:396–403.
- Nordsmark M, Bentzen SM, Rudat V, Brizel D, Lartigau E, Stadler P, . Prognostic value of tumor oxygenation in 397 head and neck tumors after primary radiation therapy. An international multi-center study. Radiother Oncol 2005;77: 18–24.
- Stadler P, Becker A, Feldmann HJ, Hansgen G, Dunst J, Wurschmidt F, . Influence of the hypoxic subvolume on the survival of patients with head and neck cancer. Int J Radiat Oncol Biol Phys 1999;44:749–54.
- Evans JC, Bergsjo P. The influence of anemia on the results of radiotherapy in carcinoma of the cervix. Radiology 1965; 84:709–17.
- Vaupel P, Mayer A, Hockel M. Impact of hemoglobin levels on tumor oxygenation: The higher, the better? Strahlenther Onkol 2006;182:63–71.
- Horsman MR. Measurement of tumor oxygenation. Int J Radiat Oncol Biol Phys 1998;42:701–4.
- Overgaard J. Hypoxic radiosensitization: Adored and ignored. J Clin Oncol 2007;25:4066–74.
- Hirst DG, Wood PJ. The adaptive response of mouse tumours to anaemia and retransfusion. Int J Radiat Biol Relat Stud Phys Chem Med 1987;51:597–609.
- Hill RP, Bush RS, Yeung P. The effect of anaemia on the fraction of hypoxic cells in an experimental tumour. Br J Radiol 1971;44:299–304.
- Hewitt HB, Blake ER. Effect of induced host anaemia on the viability and radiosensitivity of murine malignant cells in vivo. Br J Cancer 1971;25:323–36.
- Hirst DG, Brown JM. The influence of hemoglobin level on radiobiological hypoxia in tumors. Adv Exp Med Biol 1986; 200:603–8.
- Sealy R, Jacobs P, Wood L, Levin W, Barry L, Boniaszczuk J, . The treatment of tumors by the induction of anemia and irradiation in hyperbaric oxygen. Cancer 1989;64: 646–52.
- Levine EA, Vijayakumar S. Blood transfusion in patients receiving radical radiotherapy: A reappraisal. Onkologie 1993;16:79–87.
- Lee WR, Berkey B, Marcial V, Fu KK, Cooper JS, Vikram B, . Anemia is associated with decreased survival and increased locoregional failure in patients with locally advanced head and neck carcinoma: A secondary analysis of RTOG 85–27. Int J Radiat Oncol Biol Phys 1998;42: 1069–75.
- Dische S, Anderson PJ, Sealy R, Watson ER. Carcinoma of the cervix – anaemia, radiotherapy and hyperbaric oxygen. Br J Radiol 1983;56:251–5.
- Varlotto J, Stevenson MA. Anemia, tumor hypoxemia, and the cancer patient. Int J Radiat Oncol Biol Phys 2005;63: 25–36.
- Fortin A, Wang CS, Vigneault E. Effect of pretreatment anemia on treatment outcome of concurrent radiochemotherapy in patients with head and neck cancer. Int J Radiat Oncol Biol Phys 2008;72:255–60.
- Bush RS, Jenkin RD, Allt WE, Beale FA, Bean H, Dembo AJ, . Definitive evidence for hypoxic cells influencing cure in cancer therapy. Br J Cancer Suppl 1978;3: 302–6.
- Fyles AW, Milosevic M, Pintilie M, Syed A, Hill RP. Anemia, hypoxia and transfusion in patients with cervix cancer: A review. Radiother Oncol 2000;57:13–9.
- Grogan M, Thomas GM, Melamed I, Wong FL, Pearcey RG, Joseph PK, . The importance of hemoglobin levels during radiotherapy for carcinoma of the cervix. Cancer 1999;86: 1528–36.
- Henke M, Laszig R, Rube C, Schafer U, Haase KD, Schilcher B, . Erythropoietin to treat head and neck cancer patients with anaemia undergoing radiotherapy: Randomised, double-blind, placebo-controlled trial. Lancet 2003;362:1255–60.
- Machtay M, Pajak TF, Suntharalingam M, Shenouda G, Hershock D, Stripp DC, . Radiotherapy with or without erythropoietin for anemic patients with head and neck cancer: A randomized trial of the Radiation Therapy Oncology Group (RTOG 99-03). Int J Radiat Oncol Biol Phys 2007;69:1008–17.
- Hoskin PJ, Robinson M, Slevin N, Morgan D, Harrington K, Gaffney C. Effect of epoetin alfa on survival and cancer treatment-related anemia and fatigue in patients receiving radical radiotherapy with curative intent for head and neck cancer. J Clin Oncol 2009;27:5751–6.
- Barbera L, Thomas G. Erythropoiesis stimulating agents, thrombosis and cancer. Radiother Oncol 2010;95: 269–76.
- Overgaard J, Hoff CM, Hansen HS, Specht L, Overgaard M, Grau C, . Randomized study of darbepoetin alfa as modifier of radiotherapy in patients with primary squamous cell carcinoma of the head and neck (HNSCC): Final outcome of the DAHANCA 10 trial. J Clin Oncol 2009;27: 15s Abstract 6007.
- Bohlius J, Schmidlin K, Brillant C, Schwarzer G, Trelle S, Seidenfeld J, . Recombinant human erythropoiesis-stimulating agents and mortality in patients with cancer: A meta-analysis of randomised trials. Lancet 2009;373: 1532–42.
- Lambin P, Ramaekers BL, van Mastrigt GA, Van den Ende P, de JJ, De Ruysscher DK, . Erythropoietin as an adjuvant treatment with (chemo) radiation therapy for head and neck cancer. Cochrane Database Syst Rev 2009; CD006158.
- Overgaard J, Hansen HS, Overgaard M, Bastholt L, Berthelsen A, Specht L, . A randomized double-blind phase III study of nimorazole as a hypoxic radiosensitizer of primary radiotherapy in supraglottic larynx and pharynx carcinoma. Results of the Danish Head and Neck Cancer Study (DAHANCA) Protocol 5-85. Radiother Oncol 1998; 46:135–46.
- Overgaard J, Eriksen JG, Nordsmark M, Alsner J, Horsman MR. Plasma osteopontin, hypoxia, and response to the hypoxia sensitiser nimorazole in radiotherapy of head and neck cancer: Results from the DAHANCA 5 randomised double-blind placebo-controlled trial. Lancet Oncol 2005;6: 757–64.
- Eriksen JG, Steiniche T, Overgaard J. The influence of epidermal growth factor receptor and tumor differentiation on the response to accelerated radiotherapy of squamous cell carcinomas of the head and neck in the randomized DAHANCA 6 and 7 study. Radiother Oncol 2005;74: 93–100.
- Lassen P, Eriksen JG, Hamilton-Dutoit S, Tramm T, Alsner J, Overgaard J. Effect of HPV-associated p16INK4A expression on response to radiotherapy and survival in squamous cell carcinoma of the head and neck. J Clin Oncol 2009;27:1992–8.
- Lassen P. The role of human papillomavirus in head and neck cancer and the impact on radiotherapy outcome. Radiother Oncol 2010;95:371–80.
- Boeje CR, Dalton SO, Kristensen CA, Andersen E, Johansen J, Andersen LJ, . Comorbidity among 13651 head and neck cancer patients from the DAHANCA-database. Radiother Oncol 2011;98:S1–3.
- Blajchman MA, Bordin JO. The tumor growth-promoting effect of allogeneic blood transfusions. Immunol Invest 1995; 24:311–7.
- Bentzen SM, Balslev I, Pedersen M, Teglbjaerg PS, Hanberg-Sorensen F, Bone J, . Blood transfusion and prognosis in Dukes’ B and C colorectal cancer. Eur J Cancer 1990;26: 457–63.