To the Editor,
A 47-year-old male with no significant past medical history presented with a gradually progressive right neck mass over a period of 18 months. Initial evaluation by an otolaryngolosit revealed a proliferative lesion of size 2 cm at the right base of tongue and a 3 cm to 4 cm right cervical lymph node which was non-tender and mobile involving level II. He underwent flexible laryngoscopy that also showed a 2 cm proliferative lesion at the base of tongue, not crossing the midline, but no other additional findings. Biopsy from the base of tongue lesion reported poorly differentiated squamous cell carcinoma. A neck computed tomography scan with contrast confirmed a 2 cm enhancing lesion at the base of tongue and a 4 cm right cervical lymph node involving level IIA. The tumor was staged as a T1N2aM0 squamous cell carcinoma. He was treated with intensity modulated radiation therapy to a total dose of 70 Gy delivered in 5 fractions per week over seven weeks concurrently with weekly cisplatin of 40 mg/m2. Maximum spinal cord dose was limited to 44.8 Gy. He was immobilized using an S-frame, head, neck and shoulder mask. Daily set-up verification for radiation therapy was performed using on board KVCT volumetric imaging.
Seven months after completion of chemoradiation therapy he presented with a recurrent right cervical lymphadenopathy and underwent right modified radical neck dissection.
After surgery, he shortly developed sensory loss from the nipples down bilaterally, and over a two-month period his symptoms worsened. In addition, he also developed bowel and bladder incontinence, gait instability, and mild weakness of all four extremities. His physical exam was remarkable with mild weakness in the upper extremities and decreased sensation to light touch, pin-prick, and temperature from the C4 down. Additionally, he had markedly reduced vibratory and position sense in all four extremities. He could walk, but his gait was wide-based and required assistance.
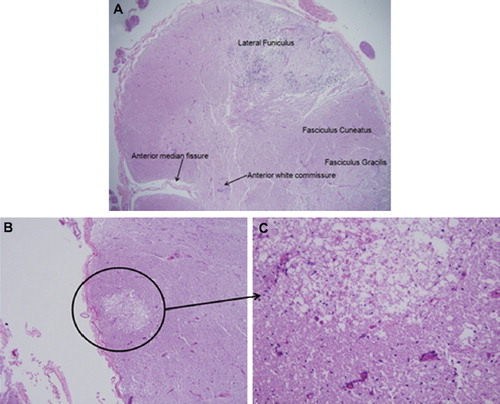
His laboratory studies including vitamin B12 level were unremarkable. His CSF revealed a negative cytology and no oligoclonal bands were detected. In addition, gram stain, fungal, and bacterial cultures, VZV, CMV, and EBV testing were negative from the CSF. Magnetic resonance imaging of his spinal cord revealed a T2 bright () and T1 post-gadolinium enhancing lesion () in the cervical spinal cord. He underwent a C2-C4 laminectomy for biopsy. He was eventually discharged to home with a percutaneous gastrotomy tube and continued physical therapy. The next month, he was hospitalized for right lower lobe pneumonia and methicillin resistant staphylococcus aureus (MRSA) bacteremia then unfortunately rapidly deteriorated and became unresponsive. He was not intubated in accordance with his prior decision, and he eventually expired. An autopsy was performed and the histopathology of the cervical spinal revealed significant damage particularly prominent in some areas of the lateral funiculi (), which normally carry corticospinal, rubrospinal, spinocerebellar and reticulospinal fibers. The presence of spheroids (, circles) was indicative of an axonal type injury compatible with myelopathy. In addition, specific staining of myelin revealed demyelination in that area (). Other important findings included vascular damage which was suggestive of radiation myelopathy. The small vessels had lost their endothelial lining, which was replaced by hyaline material (, arrows). The surrounding skeletal muscle also showed signs of damage from the radiation ().
Figure 1. MRI of cervical spine, T2 weighted (A) and post-gadolinium T1 weighted (B) showing the bright lesion.
Figure 3. Histopathology of spinal cord showing spheroids (A), demyelination (B), hyalinization of small vessels (C) and significant damage to adjacent skeletal muscle (D), all indicating radiation effects.
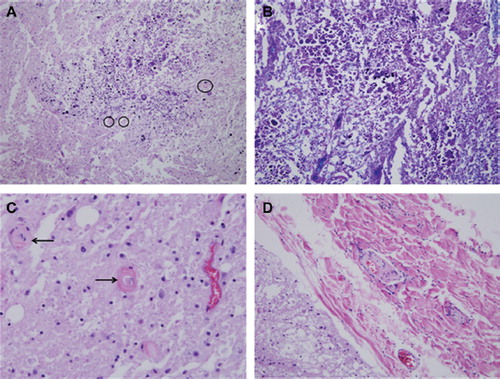
Radiation myelopathy (RM) mostly occurs between six months to three years after ionizing radiation therapy for tumors in the area in which some parts of the spinal cord are inevitably exposed. The clinical manifestation is usually variable and includes pain, sensory or motor dysfunction and bowel/bladder incontinence. Most cases are mild to moderate; however severe and progressive forms have been rarely reported in the literature [Citation1,Citation2]. The risk of RM is dose dependent and the chance of RM significantly increases with doses higher than 61 Gy. The cervical spine is more susceptible to RM than the thoracic spine [Citation1]. Besides radiation dose, other factors like dose per fraction, overall exposure time, volume, host factors such as history of diabetes or any vascular diseases, simultaneous use of medications and finally individual sensitivity to radiation play a role in development of RM [Citation3]. From a histopathological perspective, radiation myelopathy mostly affects white matter involving myelinated fibers, blood vessels and particularly lateral funiculi as was evident in our patient. Glial and endothelial cells are known as the main targets for RM. White matter changes usually precede vasculopathies. The characteristic histopathology findings include foci of demyelination, necrosis, altered vascularity, hyaline or fibrinoid degeneration and vascular thickening [Citation4]. Neuroimaging findings of RM are non-specific. The most common reported pattern in cervical cord RM is a long segment of low signal intensity on T1- weighted and high signal intensity on T2- weighted images plus variable edema and enhancement [Citation5,Citation6].
Corticosteroids may play a role in treatment of RM and sometimes the response is dramatic with complete radiologic resolution of the lesions [Citation6]. To the best of our knowledge, herein we reported the first case of tongue squamous cell carcinoma that developed a severe and rapidly progressive type of RM and eventually succumbed to its complications.
Acknowledgements
This work was supported in part by grants from NIH 3P30CA023100-25S8 to S. Kesari.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Kirkpatrick JP, van der Kogel AJ, Schultheiss TE. Radiation dose-volume effects in the spinal cord. Int J Radiat Oncol Biol Phys 2010;76(3 Suppl):S42–9.
- Schultheiss TE, Kun LE, Ang KK, Stephens LC. Radiation response of the central nervous system. Int J Radiat Oncol Biol Phys 1995;31:1093–112.
- New P. Radiation injury to the nervous system. Curr Opin Neurol 2001;14:725–34.
- Okada S, Okeda R. Pathology of radiation myelopathy. Neuropathology 2001;21:247–65.
- Wang PY, Shen WC, Jan JS. MR imaging in radiation myelopathy. AJNR Am J Neuroradiol 1992;13:1049–55; Discussion 1056–8.
- Genc M, Genc E, Genc BO, Kiresi DA. Significant response of radiation induced CNS toxicity to high dose steroid administration. Br J Radiol 2006;79:e196–9.