To the Editor,
Solid organ transplants have an increased risk of malignancy. Post-transplant lymphoproliferative disorders (PTLDs), associated with viral reactivation, are the most frequent malignancy, often seen within the first two years after transplantation. Solid tumors are seen later and are normally not virus associated.
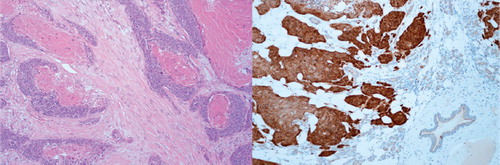
We describe a lung-transplant patient with many simultaneous human papilloma virus (HPV) positive squamous cell carcinomas (SCCs) in the skin and lungs that developed after the immunosuppressive treatment regimen was altered. A Caucasian 54-year-old man received a bilateral lung transplant in 1994 due to emphysema and α1-antitrypsin deficiency. The initial immunosuppressive treatment included cyclosporine, azathioprine and prednisolone. The first 12 years were unremarkable, with no severe rejections or infections. In 2006, the patient was admitted to our hospital due to recurrent lower respiratory tract infections (LRTI). High resolution computed tomography (HRCT) was compatible with bronchiolitis obliterans syndrome (BOS), as confirmed by a decrease in pulmonary function to forced expiratory volume in 1 s (FEV1) 1.7 l (best FEV1 3.25 l after transplantation). Also, progressive renal insufficiency with a low glomerular filtration rate was diagnosed, and the immunosuppressive treatment was changed from cyclosporine to combination therapy with low-dose cyclosporine and everolimus. Hereafter, the patient developed several leukopenic LRTIs and scabies. Five months later, a basal cell carcinoma on the nose was diagnosed and removed along with another malignant tumor, which was considered a sweat-gland tumor. A parotidectomy was performed due to SCC. A chest CT-scan showed several small nodular infiltrates in close relation to the bronchiectasis, and a PET-CT scan showed uptake in the small foci in the lungs as well as in the thoracic lymph nodes. A repeated chest CT-scan () showed progression of the pulmonary infiltrates in both number and size, and a percutaneous lung biopsy confirmed p-16 positive SCC.
Morphological and immunohistochemical similarities between biopsies were observed for all tumors, although the growth patterns were different. The expressions of p16 were analyzed using immunohistochemical staining of formalin fixed paraffin embedded tissue. We used a standard protocol with microwave retrieval. The primary antibody used was monoclonal p16 antibody (ab54210, Abcam) whereas EnVisionTM + Dual Link System-HRP (DAKO, Denmark) and 3, 3- diaminobenzidine tetrahydro-chloride (Kem-En-Tek, Denmark) was used as secondary reagent and visualization, respectively.
Due to the occurrence of multiple SCCs in the skin and parotic gland, and at multiple sites in the lungs, we considered the tumors as simultaneous cancers instead of metastasis (a diagnostic tonsillectomy revealed no malignancy). The patient died a few months later due to uremia. Unfortunately, an autopsy was not allowed by the relatives.
The association between HPV infection and carcinomas of the lung is well described. HPV infections are not only related to lung SCC but also to adenocarcinomas. Both high- and low-risk HPV types exist. Furthermore, 24.5% of patients with lung cancer are HPV positive, although the incidence varies with geography [Citation1,Citation2].
Immunosuppression in solid organ transplants increases the risk of infections. In long-term transplant survivors, the incidence of HPV infection in the skin ranges between 24% and 53%, dependent on the level of immunosuppression [Citation3].
PTLD are primarily seen in the first years after transplantation [Citation4], but skin cancers comprise the second largest group and are the most significant cancer form in long-term survivors. Organ transplants have a 60–100 times greater risk of inducing SCC in the skin as compared to the immunocompetent population [Citation5].
M-tor inhibitors such as everolimus are new immunosuppressant agents, chosen primarily due to the lack of nephrotoxicity. Everolimus is an antiangiogenic drug with an anti-tumor effect. Previous studies have described the regression of non-melanoma skin cancer after a shift in treatment from calcineurin inhibitors to everolimus [Citation6]. Our patient displayed no such effect, as he developed cancer that also progressed intensely after this change in therapy.
The association between HPV and lung cancer is well described, but not always well recognized among physicians including ourselves. To our knowledge this is the first case to describe the relation in a lung transplanted patient. HPV associated cancers should be taken into consideration when examining malignancies in head and neck and lung cancer in transplanted patients.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Klein F, Amin Kotb WF, Petersen I. Incidence of human papilloma virus in lung cancer. Lung Cancer 2009; 65:13–8.
- Koshiol J, Rotunno M, Gillison M, Doorn LJ, Chaturvedi A, Tarantini L, . Assessment of human papillomavirus in lung tumor tissue. J Natl Cancer Inst 2011;103:501–7.
- Ulrich C, Hackethal M, Meyer T, Geusau A, Nindl I, Ulrich M, . Skin infections in organ transplant recipients. J Dtsch Dermatol Ges 2008:6:98–105.
- Evens AM, Roy R, Sterrenberg D, Moll MZ, Chadburn A, Gordon LI. Post-transplantation lymphoproliferative disorders: Diagnosis, prognosis, and current approaches to therapy. Curr Oncol Rep 2010;12:383–94.
- Hofbauer GFL, Bavinck JN, Euvrard S. Organ transplantation and skin cancer: Basic problems and new perspectives. Exp Dermathol 2010;19:473–82.
- Zwald F, Brown M. Skin cancer in solid organ transplant recipients: Advances in therapy and management. J Am Acad Dermatol 2011;65:253–61.