To the Editor,
A 20-year-old male was initially diagnosed with classical seminoma with para-aortic lymphadenopathy and pulmonary metastasis. Post-orchidectomy staging was T1 N2 M1a S1, good risk stage III disease with persistently elevated lactate dehydrogenase (LDH) and beta-human chorionic gonadotrophin (βHCG), based on International Germ Cell Consensus Classification Group (IGCCCG) classification and was treated with four cycles of cisplatin and etoposide. βHCG level normalised after Cycle 2 but began rising after Cycle 3. Post-treatment computed tomography (CT)-scan showed new abdominal lymphadenopathy. The patient was deemed platinum refractory and was treated with two cycles of paclitaxel and infosfamide followed by three cycles of high-dose carboplatin and etoposide with growth factor support and stem cell rescue. Tumour markers normalised and there was no radiographic evidence of disease following salvage chemotherapy.
A follow-up surveillance CT-scan five years later showed newly-developed bulky mediastinal lymphadenopathy measuring up to 3 cm (Figure 1a and b). Tumour markers were all within normal range. Clinical assessment showed that patient continued to be free of focal and constitutional symptoms, with normal physical examination. After a presentation of the case at our multi-disciplinary team meeting it was felt that this new radiologic finding was suspicious of disease recurrence and an endoscopic transbronchial needle biopsy was recommended. Cytological evaluation revealed multiple non-caseating granulomata on a background of inflammatory cells, with no evidence of malignant cells (Supplementary Figure 1a and b to be found online at http://www.informahealthcare.com/doi/abs/10.3109/0284186X.2012.689854). Serum angiotensin converting enzyme (ACE) level was 150U/l (normal range: 40–135U/l). These findings were consistent with sarcoidosis. The patient was commenced on high dose oral prednisolone and after three months of tapering steroids a repeat CT-scan showed complete resolution of his mediastinal lymphadenopathy (Figure 2a and b). Testicular tumour markers remain within normal limits.
Figure 1a and b. Axial and coronal cuts of CT-scans of thorax showing multiple enlarged mediastinal lymph nodes
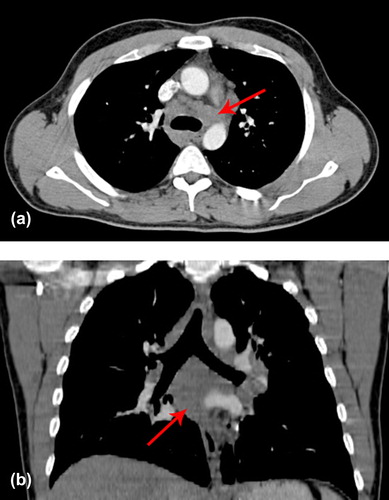
Figure 2a and b. Axial and coronal cuts of CT-scans showing resolution of mediastinal lymphadenopathy
Germ cell tumours are considered a model for curable cancer, with excellent survival outcome. Up to 90% of seminoma falls into the good prognosis group at initial presentation, with five-year survival over 90% [Citation1]. However, survival of patients with relapsed disease after first-line chemotherapy is less favourable. Platinum-refractoriness has been identified as a poor prognostic indicator [Citation2]. In relapsed seminoma, a response rate of up to 83% is seen with salvage chemotherapy with vinblastine, ifosfamide and cisplatin (VeIP), but only 54% maintain long-term survival [Citation3]. High-dose chemotherapy with autologous stem cell support could potentially confer cure in the second- and third-line setting, with overall survival of 75% for relapsed pure seminomas [Citation4]. Disease relapse after high-dose treatment is associated with a poor prognosis and the chance of prolonged remission is small, with response rates in the range of 18–36% [Citation5,Citation6].
Sarcoidosis is a multi-organ granulomatous disease of uncertain aetiology. It is proposed that the underlying aetiology is due to a T-helper cell-1- mediated immune response to an unidentified antigen in a genetically susceptible host [Citation7]. The controversial link between sarcoidosis or sarcoid-like reactions and malignancy was first made in the 1970s and linkage analysis has suggested an association in at least a quarter of all malignancies. This association is thought to be due to soluble antigenic factors shed by tumour cells or released by the tumour as a result of tumour necrosis. An increased incidence of sarcoidosis in patients with testicular cancer has been observed [Citation8] at the time of and up to five years after diagnosis of seminomas [Citation8–10]. Isolated recurrence of testicular cancer in the mediastinum is uncommon. In the Spanish Germ Cell Cancer Group study investigating chemotherapy in stage IIA and IIB seminoma, all relapses involved the retroperitoneum [Citation11], whereas more than 90% of cases of sarcoidosis involve the mediastinal lymph nodes or lungs [Citation12]. Neither positron emission tomography (PET)/CT nor tumour markers are of benefit in differentiating between sarcoidosis and malignant processes [Citation13]. Non-caseating granulomata can be seen in cancer specimens and placental alkaline phosphatise (PLAP) staining has been shown to cross-react between seminoma and sarcoidosis [Citation13].
There are few reports describing the development of sarcoidosis or sarcoid-like reactions following stem cell transplantation. Four cases describe the development of sarcoidosis following allogeneic stem cell transplantation for non-Hodgkin lymphoma and chronic myeloid leukaemia, respectively [Citation14–17]. Three cases of sarcoidosis following autologous stem cell transplant for breast cancer have also been reported [Citation18].
Haematopoietic stem cell transplantation has been postulated to reset the adaptive immune system. Transplantation restores previously-impaired T-cell responsiveness and alters the balance between T-helper-pathways [Citation19]. Reconstituted T-cells also demonstrate an overall broader clonal diversity and extensive renewal of clonal specificities, with profound qualitative immunological changes and reconfiguration [Citation20]. Autoimmune diseases such as acquired factor VIII inhibitors and autoimmune cytopaenias have been reported to develop in 2–5% of haematologic malignancies and 3–4% of autoimmune conditions, e.g. systemic lupus erythematosus and multiple sclerosis following transplantation [Citation21]. Most cases have been attributed to immunologic imbalances following transplantation [Citation22]. It is uncertain whether similar mechanisms contribute to the development of sarcoidosis.
As far as we are aware, our case is the first report of sarcoidosis on a background of disseminated seminoma treated with high-dose chemotherapy plus autologous stem cell support. Also, to our knowledge there are no reports of sarcoidosis following similar treatment for non-seminomatous germ cell tumours. The exact correlation between sarcoidosis and pathogenesis on a background of stem cell transplantation remains to be fully elucidated. In clinical practice, tissue biopsy is crucial prior to determining a relapse of testicular cancer especially in those cases many years out from the initial diagnosis.
A heightened physician awareness of sarcoidosis is appropriate in those patients with testicular cancer who present with enlarged lymph nodes, especially in the thorax, and normal tumour markers.
Supplementary Figure 1.
Download PDF (899.9 KB)Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- International Germ Cell Consensus Classification: A prognostic factor-based staging system for metastatic germ cell cancers. International Germ Cell Cancer Collaborative Group. J Clin Oncol 1997;15:594–603.
- Beyer J, Kramar A, Mandanas R, Linkesch W, Greinix A, Droz JP, et al. High-dose chemotherapy as salvage treatment in germ cell tumors: A multivariate analysis of prognostic variables. J Clin Oncol 1996;14:2638–45.
- Miller KD, Loehrer PJ, Gonin R, Einhorn LH. Salvage chemotherapy with vinblastine, ifosfamide, and cisplatin in recurrent seminoma. J Clin Oncol 1997;15:1427–31.
- Agarwala A, Perkins S, Abonour R, Brames M, Einhorn L. Salvage chemotherapy with high-dose carboplatin and etoposide with peripheral blood stem cell transplant in patients with relapsed pure seminoma. Am J Clin Oncol 2011;34: 286–8.
- Pont J, Bokemeyer C, Harstrick A, Sellner F, Greinix H, Stoiber F. Chemotherapy for germ cell tumors relapsing after high-dose chemotherapy and stem cell support: A retrospective multicenter study of the Austrian Study Group on Urologic Oncology. Ann Oncol 1997;8:1229–34.
- Porcu P, Bhatia S, Sharma M, Einhorn LH. Results of treatment after relapse from high-dose chemotherapy in germ cell tumors. J Clin Oncol 2000;18:1181–6.
- Ali MM, Atwan AA, Gonzalez ML. Cutaneous sarcoidosis: Updates in the pathogenesis. J Eur Acad Dermatol Venereol 2010;24:747–55.
- El-Gammal A, O’Keefe M, O’Driscoll M, O’Reilly S, O’Connor T. Association of testicular neoplasia and sarcoidosis. Respir Med Extra 2007;3:182–5.
- Jegannathen A, Taylor M, Jones M, Logue J. Testicular seminoma with mediastinal lymphadenopathy – a diagnostic pitfall. Br J Radiol 2009;82:e85–6.
- Tjan-Heijnen VC, Vlasveld LT, Pernet FP, Pauwels P, de Mulder PH. Coincidence of seminoma and sarcoidosis: A myth or fact? Ann Oncol 1998;9:321–5.
- Garcia-del-Muro X, Maroto P, Gumà J, Sastre J, López Brea M, Arranz JA, et al. Chemotherapy as an alternative to radiotherapy in the treatment of stage IIA and IIB testicular seminoma: A Spanish Germ Cell Cancer Group Study. J Clin Oncol 2008;26:5416–21.
- Costabel U. Sarcoidosis: Clinical update. Eur Respir J Suppl 2001;32:56s–68s.
- Karapetis CS, Strickland AH, Yip D, van der Walt JD, Harper PG. PET and PLAP in suspected testicular cancer relapse: Beware sarcoidosis. Ann Oncol 2001;12:1485–8.
- Heyll A, Meckenstock G, Aul C, Söhngen D, Borchard F, Hadding U, Mödder U, et al. Possible transmission of sarcoidosis via allogeneic bone marrow transplantation. Bone Marrow Transplant 1994;14:161–4.
- Schattenberg AV, Baynes C, van Dijk MC, Koster A, van Cleef PH, Preijers FW, et al. A mediastinal mass after donor lymphocyte infusion for relapse of chronic myeloid leukemia after allogeneic stem cell transplantation. Leukemia Lymphoma 2006;47:1188–90.
- Sundar KM, Carveth HJ, Gosselin MV, Beatty PG, Colby TV, Hoidal JR. Granulomatous pneumonitis following bone marrow transplantation. Bone Marrow Transplant 2001;28: 627–30.
- Tauro S, Mahendra P. Resolution of sarcoidosis after allogeneic bone marrow transplantation with donor lymphocyte infusions. Bone Marrow Transplant 2001;27:757–9.
- Bhagat R, Rizzieri DA, Vredenburgh JJ, Chao NJ, Folz RJ. Pulmonary sarcoidosis following stem cell transplantation: Is it more than a chance occurrence? Chest 2004;126:642–4.
- Traynor AE, Schroeder J, Rosa RM, Cheng D, Stefka J, Mujais S, et al. Treatment of severe systemic lupus erythematosus with high-dose chemotherapy and haemopoietic stem-cell transplantation: A phase I study. Lancet 2000;356:701–7.
- Muraro PA, Douek DC, Packer A, Chung K, Guenaga FJ, Cassiani-Ingoni R, et al. Thymic output generates a new and diverse TCR repertoire after autologous stem cell transplantation in multiple sclerosis patients. J Experiment Med 2005;201:805–16.
- Loh Y, Oyama Y, Statkute L, Quigley K, Yaung K, Gonda E, et al. Development of a secondary autoimmune disorder after hematopoietic stem cell transplantation for autoimmune diseases: Role of conditioning regimen used. Blood 2007;109:2643–648.
- Sherer Y, Shoenfeld Y. Autoimmune diseases and autoimmunity post-bone marrow transplantation. Bone Marrow Transplant 1998;22:873–81.
