Abstract
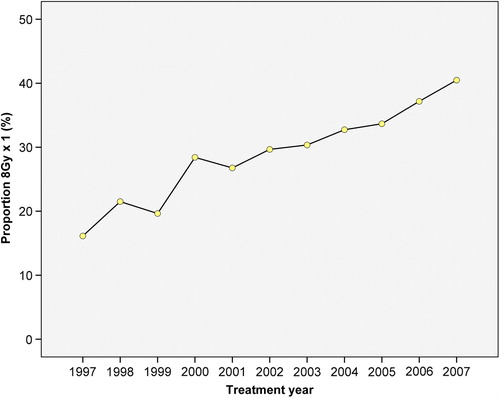
Numerous randomised clinical trials have shown that the efficacy of single fraction radiotherapy for metastatic bone pain corresponds to that of multiple fractions of radiotherapy for the majority of patients. It is not clear to which extent single fraction radiotherapy has been implemented into clinical practice. Material and methods. A Norwegian national registry-based study was conducted, including all radiotherapy schedules of 8 Gy × 1 and 3 Gy × 10 delivered to bone metastases in 1997–2007. Binomial regression analyses were used to study whether treatment centre, primary diagnosis, anatomical region irradiated, age, sex, and travel distance, were associated with the choice of fractionation. Results. A total of 14 380 radiotherapy episodes were identified. During the period 31% of the treatments were delivered as 8 Gy × 1. The proportion of single fraction treatments increased from 16% in 1997 to 41% in 2007. There were substantial differences in the proportion of single fraction treatments between the treatment centres (range 25–54%). These differences persisted after adjustment for sex, age, primary diagnosis, anatomical region, and travel distance. Conclusions. The study demonstrates an underutilisation of single fraction treatment for bone metastases in Norway during the study period.
Implementation of new methods in daily radiotherapy (RT) practice is usually not accompanied by a formal or legal approval of the method. This is in contrast to medical oncology, where implementation of new treatment is more strictly formalised.
The optimal RT dose for painful bone metastases has been investigated in numerous large scale randomised trials and meta-analyses. They have shown that multiple fractions of RT (schedules studied varying from 2 Gy × 15 to 5 Gy × 3) and single fraction RT (varying from 8–15 Gy × 1) have similar effect on pain relief and the need for analgesics [Citation1–7]. A greater need for re-irradiation has been identified for single fraction RT as compared to fractionated RT (11–42% vs. 0–24%) [Citation8]. Single fraction treatment is, however, recommended as the treatment of choice for most patients with bone metastases, except for the cases of pathological fractures, nerve root compressions and spinal cord compressions [Citation1,Citation6].
Since the randomised trials were published, several authors have evaluated whether single fraction RT has become the new standard of care for patients with painful bone metastases. Most of these studies have applied questionnaires to investigate the practice of radiation oncologists in treating these patients [Citation9–14]. Some studies have investigated the RT doses delivered during a limited period of time or at a small number of treatment centres [Citation15–19]. A Swedish trial reported 37% single fraction RT during 12-weeks follow-up in 2001 [Citation15], while a single centre study reported an increase in single fraction RT from 51% in 1999 to 66% in 2005 [Citation18].
In order to evaluate the transition from multiple fractions of radiotherapy to single fraction radiotherapy in Norway, we raised the following research question: What were the proportions of 8 Gy × 1 and 3 Gy × 10 delivered for bone metastases in Norway during 1997–2007?
Materials and methods
Study design and patients
Data were extracted from the Cancer Registry of Norway (CRN) in 2010. At this time, 2007 was the last year with complete data available at the registry. Of all patients that had been diagnosed with cancer from 1985 to 2007 we included the cohort that had received RT of 8 Gy × 1 or 3 Gy × 10 for bone metastases during 1997–2007. Only patients over the age of 18 were included. The following data were collected: age, sex, primary diagnosis, date of primary diagnosis, anatomical region irradiated, treatment regimen received, date for start of RT, treatment centre, the travel distance for treatment, vital status (dead, alive or emigrated), and the time of death or date of emigration. End of follow-up was defined as the last review of vital status, 31 March 2010.
The travel distance for treatment was derived from the county where the patient was settled at the time of treatment start. Google Maps© was used to evaluate the distances and the shortest possible distance by road (in some cases combined with car ferry) was chosen, given in the closest kilometer.
Statistics
Descriptive statistics was employed to estimate the frequencies of single fraction treatment according to sex, primary diagnosis, anatomical region irradiated, and treatment centre. Crude differences in age and travel distance according to treatment schedule were evaluated using the t-test for independent groups. Binomial regression analyses were used to calculate the relative risk (RR) of single fraction treatment. The variables age, sex, primary diagnosis, anatomical region irradiated, mean travel distance, and treatment centre were evaluated in crude and multivariable adjusted models. Time dependent Cox regression analyses stratified on primary diagnosis and adjusted for treatment centre, age, and sex were applied to explore the relations between treatment regimen received and prognosis. Patients still alive at the end of follow-up and patients that had emigrated were censored on the date for these events. Treatment episode was used as the observation unit in the analyses. Therefore the same individual could contribute with more than one observation, due to re-irradiations or concurrent RT to several sites coded separately. Ninety-five percent confidence intervals as well as p-values were reported. Two-sided p-values < 0.05 were considered statistically significant. The statistical software Stata version 10.1 for Windows (Stata Corp., College Station, TX, USA) was used for the binomial regression and Cox regression analyses. SPSS version 16.0 for Windows (SPSS INC., Chicago IL, USA) was used for the other analyses.
Ethics
The study was accomplished in accordance with the Helsinki Declaration. The protocol was approved by the Regional Ethical Committee, The Norwegian Social Science Data Services, and The Directorate for Health and Social Affairs.
Results
Baseline characteristics are presented in . The 14 380 treatment episodes included were delivered to 8685 patients, 40.7% (n = 3535) women. Mean age at the time of the first treatment episode was 63.2 years (range 18–95). At the end of follow-up, 94.8% (n = 8232) of the patients were dead. Single fraction treatment was given in 31.3% (n = 4494) of the overall treatment episodes during 1997–2007. displays the 16 groups of primary cancer diagnoses and the 11 groups of anatomical regions irradiated. It also lists the treatment centres delivering RT in Norway during the study period.
Table I. Baseline characteristics.
illustrates the proportion of the RT delivered as single fraction treatments during the study period. An almost linear increase in single fraction treatments was observed nationally, from 16.1% (n = 110) in 1997 to 40.5% (n = 868) in 2007.
Four treatment centres had a statistically significant increased multivariable adjusted RR of single fraction treatment compared to Oslo University Hospital, the Norwegian Radium Hospital as demonstrated in . Trends over time were studied for each treatment centre by dividing the study period into time intervals of three years (). There was an overall increase in the use of single fraction treatments (8 Gy × 1) over time at all the treatment centres except for Oslo University Hospital, Ullevål, which after an initial increase showed decreasing proportions of single fraction treatments.
Table II. The distribution of single fraction treatment regarding sex, treatment centre, primary diagnose and region irradiateda crude relative risk of 8 Gy × 1 and relative risk of 8 Gy × 1 adjusted for other variablesb.
Table III. Proportion of treatment episodes of 8 Gy × 1 according to treatment centre and time interval.
Mean travel distance was statistically significant different between the two treatment regimens, with 152 km for the single fraction treatments and 114 km for the fractionated treatments (p < 0.001). The multivariable adjusted RR of single fraction treatment was 1.05 (95% CI 1.03–1.07) per 100 km increase in travel distance ().
displays the variation in treatment schedules according to anatomical region irradiated. Some of the multivariable adjusted RRs of single fraction treatment showed statistically significant difference, with 3.46 (95% CI 2.67–4.49) for pelvis, 4.62 (95% CI 3.53–6.06) for the upper limbs, and 3.38 (95% CI 2.61–4.38) for the lower limbs, compared to the cervical column. There were also statistically significant differences in treatment schedule employed according to primary diagnoses. Comparing the most prevalent primary diagnoses, the multivariable adjusted RR of single fraction treatment was 1.71 (95% CI 1.48–1.97) for lung cancer and 1.55 (95% CI 1.33–1.81) for prostate cancer, compared to breast cancer ().
Mean age at start of treatment was statistically significant different between the two treatment regimens, with 63.4 years of age for the single fraction treatments and 61.2 years for the fractionated treatments (p < 0.001). The multivariable adjusted RR of single fraction treatment was 1.07 (95% CI 1.04–1.10) per 10 years increase in age (). In the multivariable adjusted models the RR of single fraction treatment was similar for males and females, RR of 1.04 (95% CI 0.93–1.16) for females compared to males ().
Cox regression analyses stratified on primary diagnosis and adjusted for treatment centre, age, and sex demonstrated a 1.36 times higher risk of death in the patients treated with 8 Gy × 1 compared to the patients treated with 3 Gy × 10 [Hazard Ratio (HR) = 1.36; 95% CI 1.29–1.43].
Discussion
This study demonstrates a substantial underutilisation of single fraction treatment for bone metastases in Norway between 1997 and 2007. One would expect to find a potential change in the patterns of practice in RT for bone metastases after 1999, when several of the largest studies recommending single fraction treatment were published. The use of single fraction treatment showed an overall increase during the study period, in accordance with the increasing evidences for equal effects from single fraction treatment. At the study end, the level of single fraction treatment was not higher than 40.5%. One might speculate that the use of single fraction RT has increased further after our study end, however our data material can obviously not resolve this, and whether a further increase has taken place is merely of speculative nature.
A major strength of this study is the use of the national database of the CRN. All Norwegian RT departments are obliged to report clinical and administrative data on RT to the CRN, and the CRN has documented a high degree of data quality including key aspects such as comparability, completeness and validity [Citation20]. The present study is thus based on large and reliable data of actual clinical management. To our knowledge the present study is unique reporting the actual delivered RT for bone metastases with complete data from an entire country over several years. During the planning of the present study we decided to include only the treatment schedules 3 Gy × 10 and 8 Gy × 1. These treatment schedules have been most commonly applied for fractionated treatment and single fraction treatment of bone metastases in Norway. Alternative schedules, i.e. 4 Gy × 5, have also been practiced, often delivered as a compromise between the clinician's intention and the patient's health situation. We chose to exclude these alternative schedules in order to do the analyses exclusively on the two fractionation patterns most often applied. The alternative schedules would probably be considered as multiple fractions of RT, and as a consequence of their exclusion, the proportion of single fraction treatments in our data material was increased.
Anatomical region irradiated was found to influence the choice of fractionation regimen. During the entire study period, multiple fractions of RT were the standard treatment for spinal cord compressions, nerve root compressions, fractures and postoperatively. These complications to bone metastases were not registered at the CRN. This may partly explain the low multivariable adjusted RR of single fraction treatment found for the column region in this study, and represents a limitation.
The multivariable adjusted overall risk of death was 1.36 times higher in the patients treated with 8 Gy × 1 compared to the patients that received 3 Gy × 10. Major randomised controlled trials have confirmed that there is no statistically significant difference in overall survival between single and multiple fractions of RT [Citation1,Citation4]. Patients with a long life expectancy therefore seem to have been selected for multiple fractions of RT. For years it has been discussed whether patients with prolonged survival should be offered fractionated RT in order to increase the duration of response [Citation4,Citation21]. In a trial by Hartsell et al. comparing 8 Gy × 1 and 3 Gy × 10, both regimens were equivalent in terms of pain at three months, while acute toxicity was more frequent in the multiple fractions arm [Citation22]. Time to first increase in pain has earlier been found equal in patients receiving single fraction treatment or multiple fractions of treatment [Citation1]. In a study published in 2006, at least 50% of the patients who survived for more than one year were adequately palliated with just one course of RT, and it concluded that single fraction RT should be the standard treatment also in patients with a favourable survival [Citation23]. Other studies have found the retreatment rates higher in the patients receiving single fraction treatment compared to multiple fractions [Citation1,Citation3,Citation4], but the choice to retreat has been found highly subjective and cannot be interpreted directly as a difference in duration of pain relief [Citation4,Citation6]. These evidences were published during our study period, and can therefore only have had an influence on the treatments delivered at the very last part of this period.
Age was also found to influence the choice of fractionation pattern, with the multivariable adjusted RR of single fraction treatment increasing by 7% for each 10 years increase in age. Younger patients may have been prescribed more fractionated treatments because the clinicians have continuously considered multiple fractions of RT the treatment of best quality. The older patients may have been prescribed more single fraction treatment because they have been considered frail and in benefit of limited hospital consultations.
Although an overall increase in the use of single fraction treatment during the study period was demonstrated, there were considerably differences between the treatment centres. Some of the largest university hospitals had delivered the smallest amounts of single fraction treatments, and one of the large centres had even reduced the proportion of single fraction treatments when comparing the time periods 2000–2002 versus 2006–2007. This finding is contrary to what is suggested in other studies, where the university centres and the large centres serving most patients have been suggested to deliver the largest parts of single fraction treatments [Citation24]. In Norway the reimbursement is based on diagnosis-related groups and regular financial budgeting. The reimbursement is similar for all the treatment centres, and cannot explain the differences.
The multivariable adjusted RR of single fraction RT increased 1.05 times for each 100 km increase in travel distance. This implies that patients living far from the treatment centre were more often given single fraction RT. This could have influenced on the observed differences in RR of single fraction RT between treatment centres, however, the differences between centres were sustainable in the multivariable adjusted analyses including adjustment for travel distance. We therefore believe the observed differences between centres are the results of local traditions.
The conservative approach to single fraction treatment revealed in this study may have had several negative consequences. First of all, multiple fractions of RT increase the load on the patients. This particular patient group comprises many frail patients, with a limited life expectancy. They benefit from a minimum of travelling and limited time spent hospitalised. Secondly, the treatment centres’ capacity is limited, and multiple fractions of RT may have longer waiting times as a consequence. Thirdly, in most cases the healthcare system spends more money than needed when multiple fractions of RT is practiced [Citation25].
The present results demonstrate that evidence-based changes in the field of RT are challenging. Even in a small country such as Norway it seems that the choice of treatment has been based on past teaching, local traditions and local opinion leaders rather than scientific evidence.
Acknowledgements
We thank Olaug Talleraas for assistance in extracting data from the Cancer Registry of Norway. We thank Oslo University Hospital, The Norwegian Radium Hospital; St. Olavs Hospital, University Hospital of Trondheim; Oslo University Hospital, Ullevål; University Hospital of North Norway, Tromsø; Stavanger University Hospital; Haukeland University Hospital, Bergen; Ålesund Hospital; Nordland Hospital, Bodø; Innlandet Hospital Trust, Gjøvik; and Sørlandet Hospital Kristiansand, for entering data to the Cancer Registry of Norway. The project was funded by the Faculty of Medicine at the Norwegian University of Technology and Science in Trondheim, Norway.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Yarnold JR. 8 Gy single fraction radiotherapy for the treatment of metastatic skeletal pain: Randomised comparison with a multifraction schedule over 12 months of patient follow-up. Radiother Oncol 1999;52:111–21.
- Wu JS, Wong R, Johnston M, Bezjak A, Whelan T. Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J Radiat Oncol Biol Phys 2003;55:594–605.
- Chow E, Harris K, Fan G, Tsao M, Sze WM. Palliative radiotherapy trials for bone metastases: A systematic review. J Clin Oncol 2007;25:1423–36.
- Steenland E, Leer JW, van Houwelingen H, Post WJ, van den Hout WB, Kievit J, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: A global analysis of the Dutch Bone Metastasis Study. Radiother Oncol 1999;52:101–9.
- Sze WM, Shelley MD, Held I, Wilt TJ, Mason MD. Palliation of metastatic bone pain: Single fraction versus multifraction radiotherapy – a systematic review of randomised trials. Clin Oncol 2003;15:345–52.
- van der Linden YM, Lok JJ, Steenland E, Martijn H, van Houwelingen H, Marijnen CA, et al. Single fraction radiotherapy is efficacious: A further analysis of the Dutch Bone Metastasis Study controlling for the influence of retreatment. Int J Radiat Oncol Biol Phys 2004;59:528–37.
- McQuay HJ, Collins SL, Carroll D, Moore RA. Radiotherapy for the palliation of painful bone metastases. Cochrane Database Syst Rev 2000:CD001793.
- Culleton S, Kwok S, Chow E. Radiotherapy for pain. Clin Oncol 2011;23:399–406.
- Chow E, Danjoux C, Wong R, Szumacher E, Franssen E, Fung K, et al. Palliation of bone metastases: A survey of patterns of practice among Canadian radiation oncologists. Radiother Oncol 2000;56:305–14.
- Hartsell W, Shah A, Graney M, Kun L. Palliation of bone metastases in the USA: A survey of patterns of practice. Support Care Cancer 1998;6:175.
- Maher EJ, Coia L, Duncan G, Lawton PA. Treatment strategies in advanced and metastatic cancer: Differences in attitude between the USA, Canada and Europe. Int J Radiat Oncol Biol Phys 1992;23:239–44.
- Roos DE. Continuing reluctance to use single fractions of radiotherapy for metastatic bone pain: An Australian and New Zealand practice survey and literature review. Radiother Oncol 2000;56:315–22.
- Fairchild A, Barnes E, Ghosh S, Ben-Josef E, Roos D, Hartsell W, et al. International patterns of practice in palliative radiotherapy for painful bone metastases: Evidence-based practice? Int J Radiat Oncol Biol Phys 2009;75: 1501–10.
- Lievens Y, Kesteloot K, Rijnders A, Kutcher G, Van den Bogaert W. Differences in palliative radiotherapy for bone metastases within Western European countries. Radiother Oncol 2000;56:297–303.
- Moller TR, Brorsson B, Ceberg J, Frodin JE, Lindholm C, Nylen U, et al. A prospective survey of radiotherapy practice 2001 in Sweden. Acta Oncol 2003;42:387–410.
- Stevens G, Firth I. Patterns of fractionation for palliation of bone metastases. Australas Radiol 1995;39:31–5.
- Williams MV, James ND, Summers ET, Barrett A, Ash DV. National survey of radiotherapy fractionation practice in 2003. Clin Oncol 2006;18:3–14.
- Bradley NM, Husted J, Sey MS, Sinclair E, Li KK, Husain AF, et al. Did the pattern of practice in the prescription of palliative radiotherapy for the treatment of uncomplicated bone metastases change between 1999 and 2005 at the rapid response radiotherapy program? Clin Oncol 2008;20:327–36.
- Haddad P, Wong RK, Pond GR, Soban F, Williams D, McLean M, et al. Factors influencing the use of single vs multiple fractions of palliative radiotherapy for bone metastases: A 5-year review. Clin Oncol 2005;17:430–4.
- Larsen IK, Smastuen M, Johannesen TB, Langmark F, Parkin DM, Bray F, et al. Data quality at the Cancer Registry of Norway: An overview of comparability, completeness, validity and timeliness. Eur J Cancer 2009;45:1218–31.
- Kaasa S, Brenne E, Lund JA, Fayers P, Falkmer U, Holmberg M, et al. Prospective randomised multicenter trial on single fraction radiotherapy (8 Gy × 1) versus multiple fractions (3 Gy × 10) in the treatment of painful bone metastases. Radiother Oncol 2006;79:278–84.
- Hartsell WF, Scott CB, Bruner DW, Scarantino CW, Ivker RA, Roach M, 3rd, et al. Randomized trial of short-versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst 2005;97:798–804.
- van der Linden YM, Steenland E, van Houwelingen HC, Post WJ, Oei B, Marijnen CA, et al. Patients with a favourable prognosis are equally palliated with single and multiple fraction radiotherapy: Results on survival in the Dutch Bone Metastasis Study. Radiother Oncol 2006;78:245–53.
- Bradley NM, Husted J, Sey MS, Husain AF, Sinclair E, Harris K, et al. Review of patterns of practice and patients’ preferences in the treatment of bone metastases with palliative radiotherapy. Support Care Cancer 2007;15: 373–85.
- Konski A, James J, Hartsell W, Leibenhaut MH, Janjan N, Curran W, et al. Economic analysis of radiation therapy oncology group 97-14: Multiple versus single fraction radiation treatment of patients with bone metastases. Am J Clin Oncol 2009;32:423–8.