To the Editor,
We read the paper by Valachis et al. [Citation1] which included 10 randomized controlled trials (RCTs) of low activity versus high activity radioiodine ablation after thyroidectomy. This is an interesting paper, and it concluded that a lower activity of radioiodine ablation is as effective as higher dose after surgery in patients with differentiated thyroid cancer (DTC) with lower toxicity. However, the results of this meta-analysis might be biased.
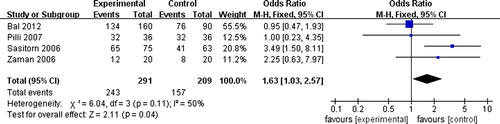
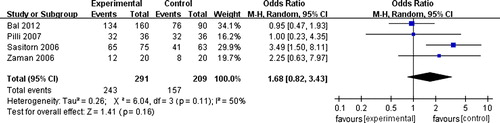
First, this study aimed to estimate the effectiveness and toxicity of low activity radioiodine ablation versus high activity in patients with DTC. Low activity was defined as activity lower than 1100 MBq and high activity as any activity higher than 1100 MBq. They also claimed that they excluded randomized trials that used activities higher or lower than 1100 MBq as low activities. Obviously in this study 1100 MBq is of low radioiodine activity and 1850 MBq and 3700 MBq are of high radioiodine activity. However, 1850 MBq is not a high dose when compared with 3700 MBq or based on clinical experience. Recent guidelines for radioiodine therapy of DTC reported that the ‘optimal’ activity for radioiodine ablation of post-surgical thyroid residues macroscopic disease was generally a single administration of 1000–5000 MBq, but within that range, remains controversial, with different centers advocating the use of 1110, 1850 or 3700 MBq [Citation2,Citation3]. For all of these reasons, it is necessary to compare 1850 MBq as low activity versus 3700 MBq as high activity in patients with DTC. Based on my knowledge and searching in Pubmed, Embase and Cochrane Central Register of Controlled Trials (2012-12-30), there were four randomized trials [Citation4–7] that compared 3700 MBq with 1850 MBq. After pooling them using different analysis methods (fixed-effect methods if we ignore the heterogeneity, or random-effects models if we incorporate heterogeneity), the results were not the same which suggested the conclusion was not stable ( under fixed-effect method, under random-effects models). In a word, the definition of high or low activity in this meta-analysis is improper, which would lead to missing relevant RCTs. In the future, what we should do is to define high or low radioiodine activity.
Second, this meta-analysis conducted a subgroup analysis of the method for TSH stimulation and sensitivity analysis of surgical procedure. However, clinical heterogeneity still existed among these studies, as the definition of successful ablation and tumor histology (papillary, follicular or mixed) could affect the results of successful ablation and they would be sources of between-study heterogeneity. So pre-specified subgroup analyses of definition of successful ablation and tumor histology should also be conducted, although sometimes it was impossible to conduct such analyses due to the lack of data. This might be the reason why statistical heterogeneity was high (I2 = 69%, p = 0.002) in this meta-analysis.
Third, another issue in this meta-analysis is how to deal with the substantial heterogeneity. This meta-analysis used random-effects models to incorporate heterogeneity. However, it is always advisable to explore possible causes of heterogeneity [Citation8]. It is not hard to find that the source of the statistical heterogeneity was due to the presence of the study by Fallahi [Citation9] with results that conflicted with the rest of the studies. In this condition, Cochrane Handbook [Citation8] suggests performing analyses both with and without this study as part of a sensitivity analysis. Therefore, this study [Citation1] should conduct meta-analyses with and without this study, even though the result with this study was as same as that without this study.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Valachis A, Nearchou A. High versus low radioiodine activity in patients with differentiated thyroid cancer: A meta-analysis. Acta Oncol Epub 2012 Nov 29.
- Luster M, Clarke SE, Dietlein M, Lassmann M, Lind P, Oyen WJ, et al. Guidelines for radioiodine therapy of differentiated thyroid cancer. Eur J Nucl Med Mol Imaging 2008; 35:1941–59.
- Hackshaw A, Harmer C, Mallick U, Haq M, Franklyn JA. 131I activity for remnant ablation in patients with differentiated thyroid cancer: A systematic review. J Clin Endocrinol Metab 2007;92:28–38.
- Sasitorn S, Vacharee B, Panya P, Supatporn T, Supot B. Prospective randomized trial for evaluation of efficacy of low versus high dose I-131 for post operative remnant ablation in differentiated thyroid cancer. Chula Med J 2006; 50:695–706.
- Zaman M, Toor R, Kamal S, Maqbool M, Habib S, Niaz K. A randomized clinical trial comparing 50mCi and 100mCi of iodine 131 for ablation of differentiated thyroid cancers. J Pak Med Assoc 2006;56:353–6.
- Pilli T, Brianzoni E, Capoccetti F, Castagna MG, Fattori S, Poggiu A, et al. A comparison of 1850 (50 mCi) and 3700 MBq (100 mCi) 131-iodine administered doses for recombinant thyrotropin-stimulated postoperative thyroid remnant ablation in differentiated thyroid cancer. J Clin Endocrinol Metab 2007;92:3542–6.
- Bal C, Chandra P, Kumar A, Dwivedi S. A randomized equivalence trial to determine the optimum dose of iodine-131 for remnant ablation in differentiated thyroid cancer. Nucl Med Commun 2012;33:1039–47.
- Higgins JP, Green S. Investigating heterogeneity in Cochrane Handbook for Systematic Reviews of Interventions 5.1.0. [updated 2011 Mar; cited 2012 Dec 30]. Available from: http://www.cochrane-handbook.org/
- Fallahi B, Beiki D, Takavar A, Fard-Esfahani A, Gilani KA, Saghari M, et al. Low versus high radioiodine dose in postoperative ablation of residual thyroid tissue in patients with differentiated thyroid carcinoma: A large randomized clinical trial. Nucl Med Commun 2012;33:275–82.