To the Editor,
Stage IVB head and neck cancer represents an unresectable disease with some chance of cure. Treatment of this extensive malignant tumor using a combination of chemotherapy and radiotherapy has resulted in complete tumor response rates of 40–71%, with survival at three years seen in approximately one third of cases (and up to 56% with follow-up of 29–45 months) and grade 2 or 3 toxicity experienced by 36–89% of patients [Citation1–3]. People with human papillomavirus (HPV) positive oropharyngeal squamous cell carcinomas (OPSCC) have a significantly better response and improved survival after aggressive therapy compared to those with HPV-negative OPSCC [Citation4–6]. We report a case of stage IVB HPV-positive OPSCC which exhibited a sustained response to induction and then concurrent chemotherapy with conservative, de-escalated dose radiotherapy (ICCR).
Case report
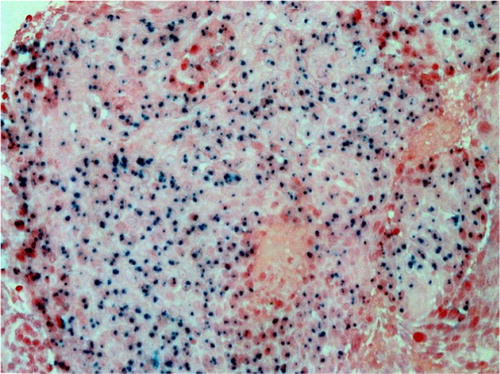
A 49-year-old man was referred in July 2001 for management of histologically-proven OPSCC (the diagnosis was established a month prior). The patient's medical history showed that he was not a smoker or an alcoholic. Physical examination revealed a reddish tumor in the right tonsil extending into the nasopharynx, ipsilateral pyriform sinus and lateral pharyngeal wall; a 0.5 cm level II lymph node was palpable in the right side of the neck. HPV-16 status was positive () after evaluation of the formalin-fixed, paraffin-embedded tumor specimens by the in situ hybridization-catalyzed signal-amplification method for biotinylated probes (GenPoint, Dako [Citation7]). A chest radiograph was normal. The multidisciplinary tumor board at our institution staged the HPV-16 positive OPSCC as IVB (T4bN1M0) and recommended ICCR with a curative intent. Combined therapy was administered in the manner akin to that mentioned in a previous report except that the employed total dose for gross disease was 60 Gy given in 30 fractions, and for subclinical disease, 50 Gy in 25 fractions [Citation8]. Treatment was well tolerated and a complete response was achieved. The patient was alive and free of cancer at the time of the last follow-up in March 2012.
Discussion
The reported incidence of stage IVB head and neck cancer is 4–27% [Citation9,Citation10]. In our institution, we observed such locally advanced, HPV-positive OPSCC in an individual who remains disease free for more than 10 years after ICCR. A review of the literature about HPV-positive OPSCC and its management by chemoradiation did not reveal a case of similar disease stage. More importantly, due to clinician preference, our administered dose (way below the standard prescription of 70 Gy) to the primary tumor was 60 Gy. This dose selection was based on the impression that chemoradiotherapy alters the potential for late effects of treatment, and the use of chemotherapy adds a biologic equivalent dose of 12 Gy [Citation11].
The reasons for the generally observed good outcome in patients with HPV-16 positive OPSCCs are not clearly known, but the various postulations include patient-related factors such as: young age, infrequent presence of co-morbidity, and limited exposure to tobacco and alcohol, the absence of field cancerization, enhanced local immunity to the viral antigen, and the theories that HPV-positive tumors are apparently less hypoxic and can be more easily induced to undergo apoptosis after chemoradiation [Citation12–15].
Appropriate selection of patients is essential to ensure that they are neither under- nor over-treated. Besides the higher cost, the use of aggressive chemoradiotherapy is associated with a greater risk of significant toxicity and smaller benefit compared to radiotherapy alone [Citation16]. HPV-16 positive OPSCCs in patients without a history of tobacco or alcohol abuse may be biologically different and more amenable to cure [Citation17]. This consideration can, perhaps, be ascribed to the hypothesis that tumors in this category do not develop as many mutations to undergo malignant transformation as a result of the viral-induced molecular changes. Very little in the way of a treatment recommendation can be drawn from this single case report. Nonetheless, under the perspective of the observed good outcome, decreasing the treatment intensity for these neoplasms which are believed to be less hypoxic, might result in lesser toxicity through reduction of treatment-associated morbidity, a more complete and durable response, and an ultimately favorable impact on long-term survival. Clinical investigations designed to identify the precise role of chemotherapy with de-intensified radiotherapy for HPV-16 positive OPSCCs are currently in progress.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Adelstein DJ, Li Y, Adams GL, Wagner H Jr, Kish JA, Ensley JF, et al. An Intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol 2003;21:92–8.
- Fu KK, Phillips TL, Silverberg IJ, Jacobs CM, Goffinet DR, Chun C, et al. Combined radiotherapy and chemotherapy with bleomycin and methotrexate for advanced inoperable head and neck cancer. Update of a Northern California Oncology Group randomized trial. J Clin Oncol 1987;5:1410–8.
- Poole ME, Sailer SL, Rosenman JG, Tepper JE, Weissler MC, Shockley WW, et al. Chemoradiation for locally advanced squamous cell carcinoma of the head and neck for organ preservation and palliation. Arch Otolaryngol Head Neck Surg 2001;127:1446–50.
- Ang KK, Harris J, Wheeler R, Weber RM, Rosenthal DI, Nguyen-Tan P, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 2010;363: 24–35.
- Fakhry C, Westra CH, Cmelak A, Ridge JA, Pinto H, Forastiere A, et al. Improved survival of patients with HPV-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 2008;100:261–9.
- Worden FP, Kumar B, Lee JS, Wolf GT, Cordell KG, Taylor JMG, et al. Chemoselection as a strategy for organ preservation in advanced oropharyngeal cancer: Response and survival positively associated with HPV16 copy number. J Clin Oncol 2008;26:3138–46.
- Huang CC, Qiu JT, Kashima ML, Kurman RJ, Wu TC. Generation of type-specific probes for the detection of single copy human papillomavirus by a novel in situ hybridization method. Mod Pathol 1998;11:971–7.
- Ampil FL, Mills GM, Stucker FJ, Burton GV, Nathan CAO. Radical combined treatment of locally extensive head and neck cancer in the elderly. Am J Otolaryngol 2001;22: 65–9.
- Iro H, Waldfahrer F. Evaluation of the newly updated TNM classification of head and neck carcinoma with data from 3247 patients. Cancer 1998;83:2201–7.
- Mendenhall WM, Parsons JT, Million RR, Cassisi NJ, Devine JW, Greene BD. A favorable subset of AJCC stage IV squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 1984;10;1841–3.
- Kasibhatla M, Kirkpatrick JP, Brizel DM. How much radiation is chemotherapy worth in advanced head and neck cancer?Int J Radiat Oncol Biol Phys 2007;68:1491–5.
- Kong CS, Narasimhan B, Cao H, Kwok S, Erickson JP, Koong A, et al. The relationship between papillomavirus status and other molecular prognostic markers in head and neck squamous cell carcinomas. Int J Radiat Oncol Biol Phys 2009;74:553–61.
- Lassen P. The role of human papillomavirus in head and neck cancer and the impact on radiotherapy outcome. Radiother Oncol 2010;95:371–80.
- O’Rorke MA, Ellison MV, Murray LJ, Moran M, James J, Anderson LA. Human papillomavirus related head and neck cancer survival: A systematic review and meta-analysis. Oral Oncol 2012;48:1191–201.
- Spanos WC, Nowicki P, Lee DW, Hoover A, Hostager B, Gupta A, et al. Immune response during therapy with cisplatin or radiation for human papillomavirus related head and neck cancer. Arch Otolaryngol Head Neck Surg 2009;135: 1137–46.
- Pignon JP, Burhis J, Domenge C, Designe L. On behalf of the MACH-NC Collaborative Group: Chemotherapy added to locoregional treatment for head and neck squamous carcinoma: Three meta-analyses of updated individual data. Lancet 2000;355:949–55.
- Agarwal JP, Mallick I, Bhutani R, Ghosh-Laskar S, Gupta T, Budrukkar A, et al. Prognostic factors in oropharyngeal cancer: Analysis of 627 cases receiving definitive radiotherapy. Acta Oncol 2009;48:1026–33.