Abstract
Background. The use of central venous lines carries a significant risk for serious complications and high economic costs. Lately, the peripherally inserted central venous catheter (PICC) has gained in popularity due to presumed advantages over other central venous lines. The aim of this systematic literature review was to identify scientific evidence justifying the use of PICC. Material and methods. The literature review was performed according to the principles of Cochrane Collaboration. The electronic literature search included common databases up to March 2011. Only those studies rated as high or moderate quality were used for grading of evidence and conclusions. Results. The search resulted in 827 abstracts, 48 articles were read in full text, and 11 met the inclusion criteria. None of the articles was classified as high quality and two had moderate quality. The results of these two studies indicate that PICC increases the risk for deep venous thrombosis (DVT), but decreases the risk for catheter occlusion. The quality of scientific evidence behind these conclusions, however, was limited. Due to the lack of studies with sufficiently high quality, questions such as early complications, patient satisfaction and costs could not be answered. Discussion. We conclude that although PICCs are frequently used in oncology, scientific evidence supporting any advantage or disadvantage of PICC when comparing PICC with traditional central venous lines is limited, apart from a tendency towards increased risk for DVT and a decreased risk for catheter occlusion with PICC.
Central venous lines are essential in the care of patients with severe diseases treated in surgical, intensive care and oncological/haematological units. Traditionally clinicians have used non-tunneled or tunneled (t-CVC) central venous catheters (CVC) or subcutaneous venous ports (PORT) inserted into the superior vena cava via the subclavian or the internal jugular veins depending on the indication and on how long the patient will require the central venous line. The placement of these lines carries a significant risk for serious complications, e.g. pneumothorax, arterial puncture, haemothorax, stroke, arrhythmias and nerve damage [Citation1]. The procedure must therefore be performed by a specially trained physician, usually on an intensive care unit or in the operating theatre. While in use, the catheters may cause other complications such as infection, deep venous thrombosis (DVT), thrombophlebitis and dislodgement. Furthermore line occlusion may occur sooner or later. Serious complications per se, or delayed treatment, can lead to increased morbidity and suffering, and sometimes, even a fatal outcome [Citation1]. Furthermore, a central venous line may affect the patient´s well-being in other respects, as it may be inconvenient and painful, leading to restrictions in daily activities and a change in body image [Citation2]. It is also evident that major as well as minor complications lead to increased costs, due to extra nursing and prolonged hospital care.
Some years ago the peripherally inserted central venous catheter (PICC) was introduced into clinical practice as an alternative to the traditional central venous line and has since gained increasing popularity [Citation3]. The PICC is a thin and long flexible catheter made of biocompatible material, either silicone or polyurethane, inserted percutaneously into the basilic or cephalic vein in the forearm or the antecubital fossa, often with the help of ultrasound or fluoroscopy guidance. The catheter is then advanced into the central circulation with tip of the catheter most often placed in the superior vena cava or at the caval-atrial junction. It is reasonable to assume that the use of PICC is associated with fewer serious complications related to the insertion of the catheter compared to other central venous lines, since direct puncture of one of the great veins at the upper thoracic aperture is avoided. It has also been claimed that PICC has fewer complications of other kinds such as infections [Citation4]. Furthermore, since the PICC can be inserted by specially trained nurses outside the operating theatre, it has been suggested that the use of this method reduces cost and decreases any delay because of busy operating or intensive care units [Citation5].
The central venous line is an important and sometimes life-saving clinical tool that unfortunately carries with it complications with significant consumption of healthcare resources. The main aim of the present systematic literature review was to evaluate the literature regarding the scientific evidence that justifies the increased use of PICC compared to other central venous lines.
Methods
The systematic literature review
The Cochrane Collaboration definition of a systematic review has been used, namely “A systematic review attempts to identify, appraise and synthesize all the empirical evidence that meets pre-specified eligibility criteria to answer a given research question. Researchers conducting systematic reviews use explicit methods aimed at minimizing bias, in order to produce more reliable findings that can be used to inform decision making.” (www.thecochranelibrary.com).
The primary questions in the present systematic literature review were:
What are the advantages and disadvantages of PICC compared to other central venous lines in terms of successful insertion rate, function, early and late complications and patient satisfaction/quality of life in patients needing a central venous line?
What does the treatment cost?
Is the treatment cost-effective?
Literature search and selection of articles
The electronic literature search included the databases PubMed, Cinahl, the Cochrane Library up to March 2011. The text words (TW) and Mesh term used were: PICC(s)(TW), peripherally inserted central catheter(s) (TW), peripherally inserted central venous catheter(s)(TW), as well as cost and cost analysis/economics (Mesh), cost effectiveness (TW), cost utility and cost benefit (TW). Language was restricted to English, Swedish and Norwegian.
Inclusion and exclusion criteria
The selection of studies was based on the following criteria:
Population: patients in all clinical areas, both children (not neonates) and adults, needing a central venous line.
Intervention: PICC, regardless of material (silicon or polyurethane), thickness, number of lumens, insertion technique (percutaneous with or without fluoroscopy or ultrasound guidance), tip appearance (valved or not valved). The catheter should be inserted in the upper extremity with the tip position in the central circulation.
Control: CVC, t-CVC or PORT.
Endpoints: successful insertion rate, function (occlusion, catheter fracture, catheter displacement), early complications (action-requiring bleeding, nerve injury, pneumothorax, haemothorax, cardiac tamponade, arrhythmias), late complications (infection, DVT, thrombophlebitis, venous stenosis), patient satisfaction and quality of life.
Study type: prospective studies only (randomised or non-randomised) with control group, and including clinical outcome measures. To examine patient satisfaction and quality of life, studies having a qualitative methodology (grounded theory and phenomenology) were eligible for inclusion.
Rating quality of individual studies
The quality of each study included was rated as high, moderate or low according to the Swedish Council on Health Technology Assessment (SBU) standard checklist determining the extent to which the studies met the basic quality criteria, e.g. study design, study population, outcome measures and the analytical methods used [Citation6]. The pre-specified criteria related to the question of the present systematic review are given in . Only studies with a high or moderate quality were considered good enough to be used for grading of scientific evidence and conclusions.
Table I. Criteria of high-, moderate- and low quality studies according to the aim of the systematic review.
Grading the scientific evidence across studies
The quality of scientific evidence of the outcomes of PICC was rated as four levels according to GRADE [Citation7,Citation8]:
High (⊕⊕⊕⊕) Based on high or moderate quality studies containing no factors that weaken overall judgment.
Moderate (⊕⊕⊕○) Based on high or moderate quality studies containing isolated factors that weaken overall judgment.
Limited (⊕⊕○○) Based on high or moderate quality studies containing factors that weaken overall judgment.
Insufficient (⊕○○○) The evidence base is insufficient when scientific evidence is lacking, the quality of available studies is low or studies of similar quality are contradictory.
The aim of applying GRADE is to find out: firstly, how much confidence one can have in a particular estimate of effect; secondly, if the result is sustainable, or if it is likely that new research findings will change the evidence within the foreseeable future. The rating usually starts at a high scoring, but during the process of analysis confidence in the evidence may decrease stepwise for several reasons including limitations in study design and/or quality, inconsistency or indirectness of results, imprecise estimates and probability of publication bias. Any disagreements on inclusion/exclusion criteria, rating quality of individual studies or quality of evidence of test methods were solved within the group of reviewers by consensus.
Results
The literature search
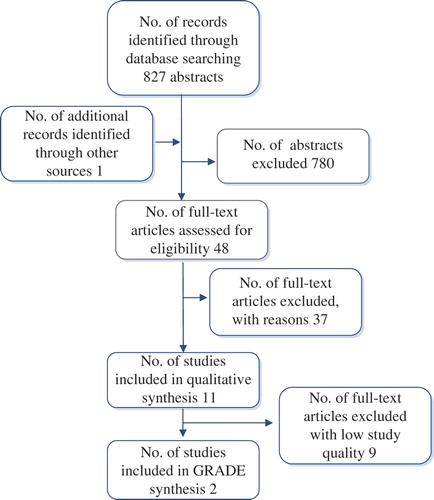
A flow chart showing the results of the literature search and the outcome of the selection procedures is given in . The electronic searches resulted in 827 abstracts. Three reviewers (EJ, FH and DL) read these abstracts independently. An article was read in full text if at least one of the three reviewers considered an abstract to be potentially relevant. Hand search and grey literature added one relevant article. Altogether, 48 articles were read in full text and assessed independently by the same three reviewers. Of these articles, 37 did not fulfill the inclusion criteria and were excluded. The remaining 11 articles met the predefined inclusion and exclusion criteria [Citation9–19] and were included and assessed using the SBU standardised checklists [Citation6] and tools. None of the included articles were classified as high study quality. Two were judged having medium quality and thus qualified to serve as a basis for the grading of the scientific evidence and conclusions [Citation9,Citation10]. Their characteristics are presented in , and the outcomes and quality of evidence according to GRADE are reported in . The remaining nine articles [Citation11–19] were found to be of low study quality, and therefore not used for further analyses.
Table II. Summary of the two studies of moderate quality.
Table III. Summary of results (GRADE); PICC in relation to other central venous lines.
Outcomes: Deep venous thrombosis and occlusion
The two studies of medium study quality are both cohort studies comparing patients with a PICC to other types of central venous lines with regard to the outcomes DVT [Citation9,Citation10] and occlusion [Citation10], respectively. In both studies, standard definitions of complications are used and the number of complications is presented as per 1000 catheter-days or with survival analysis [Citation9,Citation10] and Cox-regression.
Bonizzoli and co-workers [Citation9] investigated the prevalence of DVT when using PICC compared to traditional CVCs. In total, 239 adult patients who were discharged from an intensive care unit for further care at a medical or surgical ward were prospectively studied. The study period was eight months. Patients who were transferred during the first four months received a CVC. In the following four months the patients had a PICC inserted. The sample consisted of 114 patients with a PICC (double lumen, 5 French) and 125 patients with a CVC (triple lumen, 7 French). To prevent thrombosis, all patients were prescribed a daily dose of 5000 IU dalteparin. The personnel involved were periodically educated in the management of central venous lines. The occurrence of DVT was evaluated using ultrasound on days 7, 15 and 30 after catheter insertion. The mean catheter survival time was longer in patients with a PICC (mean 35 days) than in patients with a CVC (mean 23 days). Patients with a PICC had a statistically significantly higher incidence of confirmed DVT than patients with a CVC (7.7 vs. 4.4 per 1 000 catheter-days). No differences with regard to demographic or clinical variables were identified in patients diagnosed with DVT compared to those not developing thrombosis. In addition, a higher risk for DVT was observed in women, and if the catheter was inserted through the basilic vein of the left arm.
Revel-Vilk and co-workers [Citation10] compared in a prospective cohort study the occurrences of DVT and occlusion in patients with a PICC, t-CVC or PORT. The population consisted of 262 children and adolescents with cancer undergoing chemotherapy at three different departments. The median age of the participants was 7.4 years (range 28 days to 28 years). One patient could have one or more catheters during the study period. There were a total of 423 catheters inserted of which 188 were PICC, 104 t-CVC and 126 PORT. Patients were observed for catheter occlusion and risk factors with respect to symptomatic DVT verified with conventional methods. The mean catheter survival time of the total sample was 4.8 months, PICCs, t-CVCs and PORTs were used in 3.1, 4.1 and 9.8 months, respectively. Management of the catheters was performed according to a local protocol. The results showed that patients with a PICC were at lower risk for catheter occlusion compared to patients with a t-CVC or PORT (Hazard ratio PICC; 1 vs. t-CVC; 2.3 and PORT; 1.8). DVT occurred 14 times in 13 children. Ten of these thromboses were catheter-related. In eight of the 10 cases, the child had a PICC. A statistically significant higher risk for symptomatic DVT was observed in children with a PICC compared to the other types of catheters (Hazard ratio PICC: 7.03 vs. others: 1).
A classification of the quality of scientific evidence according to GRADE, however, indicates that the difference in outcome between PICCs and t-CVCs found in the two studies is based solely on limited scientific evidence ().
Other patient-related outcomes reviewed
We were unable to identify any relevant articles with sufficient quality focusing on the following endpoint used in the systematic literature review: successful insertion rate, catheter fracture, catheter displacement, action-requiring bleeding, nerve injury, pneumothorax, haemothorax, cardiac tamponade, arrhythmias, infection, thrombophlebitis, venous stenosis, patient satisfaction and quality of life.
Economic aspects
Since the evidence concerning patient-related outcomes was insufficient, the cost-effectiveness of using PICCs could not be appraised.
Discussion
The main aim of this article was to systematically and critically review the scientific literature comparing the use of PICC with other central venous lines in terms of successful insertion rate, function, early and late complications, patient satisfaction, and economic aspects.
The main and rather disappointing finding was that we could identify no more than two studies with an acceptable study quality (medium) that compared PICC with other central venous lines, and none with high quality. Furthermore, we were unable to identify studies of sufficiently high quality to answer the primary questions of the review related to successful insertion rate, function and early complications of the technique, compared to other central venous lines. The same was true for patient satisfaction and cost-effectiveness. However, there were two studies of acceptable quality (medium) that allowed closer analyses of the occurrence of late complications such as DVT and catheter occlusion. One study investigated the occurrence of DVT, diagnosed with ultrasound, in trauma patients who were transferred from an ICU to a surgical ward [Citation9]. The other study focused on symptomatic DVT and catheter occlusion in a pediatric oncology population [Citation10]. Both studies showed an increased incidence of DVT in patients using a PICC compared to other central venous lines. This finding is supported by a recent meta-analysis on DVT risk factors in adult oncology patients [Citation20]. However, this meta-analysis used rather wide inclusion criteria, i.e. cohort studies without control groups were included. It thus did not meet the inclusion criteria of the present systematic review and was not accepted for closer analysis. It is well known that patients with a malignancy are predisposed to develop thrombosis. The increased predisposition of PICCs to induce DVT should therefore be considered when a central venous line is chosen in this group of patients. The study of Revel-Vilk also showed a lower incidence of catheter occlusion in the PICC group compared to patients with a t-CVC or PORT. The results of the study could not explain this finding. Important factors such as kinds of solutions administrated via the catheter (concentrated glucose, parenteral nutrition, blood products etc.) and degree of adherence to catheter care routines were not presented in the study. It is important to point out that when attempting to summarise the quality of scientific evidence according to GRADE, the differences in outcome between PICC and other central venous lines, found in the two studies was based on limited scientific evidence only.
It has been stated that PICCs have a lower infection rate compared to other central venous lines [Citation4]. However, none of the studies evaluating infection complications, identified by the search, had comparable patient groups, and therefore no conclusions could be made on this matter.
Evidently, scientific evidence supporting the choice of PICC as a clinical routine method rather than traditional central venous lines is limited. The increasing popularity of PICC as an alternative to traditional CVCs has several possible explanations: fewer serious complications expected, both in relation to the insertion procedure and later, less delays, and lower cost due the possibility of insertion by nurses outside the operating and intensive care unit. According to the present study none of these arguments are based on scientific evidence.
There are some ethical aspects regarding the findings of our study. The placement and use of central venous lines carries significant risks of serious early and late complications. Different devices apparently have different risk/benefit ratios. Nonetheless new methods such as PICC, have been introduced into clinical practice without any support of high quality evidence-based research. It would seem that marketing of PICCs has been based mainly on commercial and specific professional interests. According to the ethical principles of doing good (beneficence) and doing no harm (non-maleficence) the method with the lowest risk/benefit ratio should be chosen. If such knowledge is lacking there is a risk for unnecessary harmful and unethical choices. The ethical principle of justice may be violated when economic restrictions or lack of competence in a specific department are allowed to affect the choices of central venous access, in which case the use of more harmful methods might cause unethically increased risks for serious complications and patient suffering. Furthermore, the lack of knowledge about general patient satisfaction regarding the use of different central venous lines, makes it difficult to inform the patients properly, thereby limiting the possibility of the patient to influence the choice of procedure, and to exercise their right to autonomy.
Conclusions
Unfortunately, our systematic literature review identified too few studies of sufficiently high quality to answer questions related to successful insertion rate, function, early complications, patient satisfaction and the cost-effectiveness of PICC compared to other central venous lines. The literature review identified two studies with sufficient quality with regard to late complications, the results of which indicated that PICC increases the risk for DVT, but decreases the risk for catheter occlusion. However, the quality of scientific evidence according to GRADE indicates that the difference in outcome between PICC and other central venous lines reported in these two studies is solely based on limited scientific evidence. Apparently, there is an urgent need for prospective randomised controlled studies evaluating and comparing different types of central venous lines in different patient populations. Meanwhile all units using intravascular catheters should use structured routines based on written guidelines well adapted to the clinical setting so as to guarantee maximum patient safety and satisfaction. Routines must include an effective follow-up system so as to capture early and late complications.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
The study was supported by the Swedish Council on Health Technology Assessment, SBU.
References
- Polderman KH, Girbes AJ. Central venous catheter use. Part 1: Mechanical complications. Intensive Care Med 2002;28:1–17.
- Johansson E, Engervall P, Bjorvell H, Hast R, Bjorkholm M. Patients’ perceptions of having a central venous catheter or a totally implantable subcutaneous port system-results from a randomised study in acute leukaemia. Support Care Cancer 2009;17:137–43.
- Hammarskjöld F, Nielsen N, Rödjer S, Pärsson H, Falkmer U, Malmvall BE.[Peripherally inserted central venous catheter still not evaluated for clinical use. More scientific support is needed according to a literature study]. Läkartidningen. 2008;105:1576–80.
- Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: A systematic review of 200 published prospective studies. Mayo Clin Proc 2006;81:1159–71.
- Oakley C, Wright E, Ream E. The experiences of patients and nurses with a nurse-led peripherally inserted central venous catheter line service. Eur J Oncol Nurs 2000;4:207–18.
- SBU. Utvärdering av metoder i hälso- och sjukvården – En handbok. www.sbu.se/sv/Evidensbaserad-vard/Utvardering-av-metoder-i-halso-och-sjukvarden – En-handbok/2012.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6.
- Schunemann HJ, Oxman AD, Brozek J, Glasziou P, Bossuyt P, Chang S, et al. GRADE: Assessing the quality of evidence for diagnostic recommendations. ACP J Club 2008;149:2.
- Bonizzoli M, Batacchi S, Cianchi G, Zagli G, Lapi F, Tucci V, et al. Peripherally inserted central venous catheters and central venous catheters related thrombosis in post-critical patients. Intensive Care Med 2011;37:284–9.
- Revel-Vilk S, Yacobovich J, Tamary H, Goldstein G, Nemet S, Weintraub M, et al. Risk factors for central venous catheter thrombotic complications in children and adolescents with cancer. Cancer 2010;116:4197–205.
- Mollee P, Jones M, Stackelroth J, van Kuilenburg R, Joubert W, Faoagali J, et al. Catheter-associated bloodstream infection incidence and risk factors in adults with cancer: A prospective cohort study. J Hosp Infect 2011;78:26–30.
- Alonso-Echanove J, Edwards JR, Richards MJ, Brennan P, Venezia RA, Keen J, et al. Effect of nurse staffing and antimicrobial-impregnated central venous catheters on the risk for bloodstream infections in intensive care units. Infect Control Hosp Epidemiol 2003;24:916–25.
- Cowl CT, Weinstock JV, Al-Jurf A, Ephgrave K, Murray JA, Dillon K. Complications and cost associated with parenteral nutrition delivered to hospitalized patients through either subclavian or peripherally-inserted central catheters. Clin Nutr 2000;19:237–43.
- Kim HJ, Yun J, Kim KH, Kim SH, Lee SC, Bae SB, et al. Safety and effectiveness of central venous catheterization in patients with cancer: Prospective observational study. J Korean Med Sci 2010;25:1748–53.
- Al Raiy B, Fakih MG, Bryan-Nomides N, Hopfner D, Riegel E, Nenninger T, et al. Peripherally inserted central venous catheters in the acute care setting: A safe alternative to high-risk short-term central venous catheters. Am J Infect Control 2010;38:149–53.
- Duerksen DR, Papineau N, Siemens J, Yaffe C. Peripherally inserted central catheters for parenteral nutrition: A comparison with centrally inserted catheters. JPEN J Parenter Enteral Nutr 1999;23:85–9.
- Giuffrida DJ, Bryan-Brown CW, Lumb PD, Kwun KB, Rhoades HM. Central vs peripheral venous catheters in critically ill patients. Chest 1986;90:806–9.
- Raad I, Davis S, Becker M, Hohn D, Houston D, Umphrey J, et al. Low infection rate and long durability of nontunneled silastic catheters. A safe and cost-effective alternative for long-term venous access. Arch Intern Med 1993;153:1791–6.
- Worth LJ, Seymour JF, Slavin MA. Infective and thrombotic complications of central venous catheters in patients with hematological malignancy: Prospective evaluation of nontunneled devices. Support Care Cancer 2009;17:811–8.
- Saber W, Moua T, Williams EC, Verso M, Agnelli G, Couban S, et al. Risk factors of catheter-related thrombosis (CRT) in cancer patients: A patient-level data (IPD) meta-analysis of clinical trials and prospective studies. J Thromb Haemost 2011;9:312–9.