Abstract
Introduction. Patients with left-sided breast cancer with lymph node involvement have routinely been treated with enhanced inspiration gating (EIG) for a decade at our institution. In a transition from EIG to deep inspiration breath hold (DIBH) we compared the two techniques with focus on target coverage, dose to organs at risk and reproducibility of the inspiration level (IL). Material and methods. Twenty-four patients were computed tomography (CT) scanned with EIG and DIBH. For DIBH we used visual feedback and for EIG audio coaching, both during scan and treatment. Treatment plans for 50 Gy over 25 fractions were calculated. Seventeen of the patients were included in the analysis of reproducibility. They were audio coached for one minute before beam-on in DIBH at nine treatment sessions. These respiration curves were analysed with average maximum IL and standard deviation (SD) for the EIG part of the respiratory signal, and mean IL and SD for the DIBH. Comparison of dosimetric and respiration parameters were performed with the Wilcoxon signed rank-sum test. Results. In DIBH, the ipsilateral lung volume increased further compared to EIG (p < 0.0004, mean increase 11%). This lead to a 9% mean reduction (p = 0.002) of the ipsilateral lung volume receiving 20 Gy (V20 Gy). We found no other significant dosimetric differences between the two methods. The reproducibility of the IL was better with the DIBH method, observed as a significantly smaller SD in most patients (p < 0.04 for 16 of 17 patients). Conclusion. The DIBH method resulted in a significantly larger lung volume and lower ipsilateral lung V20 Gy compared to EIG. The IL for visually guided DIBH was more reproducible than audio-coached EIG. Based on these findings, the DIBH technique is our new breathing adaptation standard for radiotherapy of patients with left-sided breast cancer with lymph node involvement.
Adjuvant radiotherapy of breast cancer implies a risk of late cardiac and pulmonary toxicity [Citation1,Citation2], which may be reduced with application of respiratory management [Citation3–6], where lung inflation reduces the amount of lung tissue within the treatment fields and increases the distance between heart and target. Early studies from our institution [Citation3,Citation4] showed that both free breathing inspiration gating (IG) and deep inspiration breath hold (DIBH) provided substantial reduction in dose to the heart and the lungs, DIBH being superior to IG. However, with mean anterio-posterior chest wall excursion in voluntary DIBH over 4 mm [Citation3], the necessary treatment margins would increase. Therefore we chose to implement enhanced inspiration gating (EIG) where an individually applied audio coaching increased the inspiration level of breathing. Analysis of the first patients showed that EIG significantly reduced the dose to the left anterior descending coronary artery (LAD) compared to the uncoached IG technique employed in the first studies [Citation7]. Since January 2004, EIG was clinical routine for radiotherapy of loco-regional left-sided breast cancer and over 1000 breast cancer patients have been treated accordingly until May 2013. However, while audio coaching increased the patients’ inspiration level, for some patients it also made it difficult to maintain the same inspiration level on a daily basis, resulting in inspiration levels outside the gating window, which prolonged their daily treatment time. The potential of visually guided DIBH over free breathing has been reported, both in terms of sparing of organs at risk (OAR) and of target coverage [Citation8–11]. Visual feedback of the patient's own respiratory signal improves the stability of the inspiration level [Citation12] and has become compatible with most clinical gating systems. We therefore wanted to investigate the potential benefit for our patient population with visually guided DIBH compared to audio-guided EIG, by focusing on: 1) the reproducibility of the inspiration level; and 2) quality of the treatment plan with respect to target coverage and dose to risk organs.
Material and methods
Twenty-eight consecutive patients with left-sided breast cancer (median age 51 years; range 29–88; all females) referred to adjuvant loco-regional radiotherapy after either mastectomy (14) or lumpectomy (14) were included in the study. The patient flow is illustrated in .
Figure 1. Patient flow in the study. One patient was only scanned in EIG because she was not able to perform a 15 s long stable DIBH. The three patients who were scanned in free breathing (FB) only did not comply with either EIG or DIBH.
Respiration monitoring and compliance
For respiratory monitoring, we used the Real-time Position Management (RPMTM) system (Varian Medical Systems Inc) consisting of an infra-red camera which tracked the respiratory signal from an externally placed plastic marker box with two optical markers. The motion of the box was a surrogate of the motion of the chest wall. Visual feedback from the RPM system was provided to the patient via the use of video goggles (Wrap 920, Vuzix Corporation, www.vuzix.com) or a small display (see Supplementary Appendix 1 available online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2013.813073). The width of the gating window was set to 2–3 mm for DIBH and 3–5 mm for EIG.
The patients were coached prior to the CT scan in a quiet room with a RPM system dedicated to the respiratory gating training. The coaching was performed either by a physicist or a specially trained nurse. After a brief introduction to respiratory gating, the audio instructions for EIG were applied and adapted individually to ensure a comfortable breathing pace at enhanced inspiration amplitude. The patient was then introduced to DIBH using visual feedback (see Supplementary Appendix 2 available online at http://informahealthcare.com/doi/ abs/10.3109/0284186X.2013.813073). The DIBH level was set individually to ensure high lung inflation that could be maintained for at least 15 seconds. This ensured that the planning CT could be acquired within a single DIBH. For both techniques no pre-set level was defined, but patients were encouraged to breathe as deeply as comfortable. For EIG, a stable inspiration level was usually found after 10–15 minutes of training with audio feedback. For DIBH, the patients usually found a comfortable deep inspiration level after two or three breath holds using the visual coaching equipment corresponding to five minutes of training. The compliance of the patients was evaluated in terms of the ability to comply with the respiratory instructions.
Treatment planning study
Patients were scanned on a CT scanner (Siemens Sensation Open), immobilised in a breast board (ConChest, Candor Aps), with both arms above their head. The marker box was positioned on the thorax of the patient, on bony structures close to the sternum and the chosen position was marked on the patient with two tattoos to ensure reproducibility for all following treatment sessions. For DIBH the scanner was operated in spiral mode and the patient was provided with visual feedback. For the following EIG scan, the scanner was operated in sequential mode and triggered by a threshold sent from the RPM system, while the patient was provided with audio coaching only.
Twenty-four patients received loco-regional treatment including the ipsilateral axillary lymph node levels II and III, peri-clavicular lymph nodes, and the internal mammary nodes (IMN) intended from intercostal spaces I through IV, while three patients received treatment of the breast only. One additional patient received bilateral treatment (loco-regional treatment on the left side and breast treatment on the right side). Delineation was performed according to national guidelines [Citation13]. On all scans we delineated the clinical target volume (CTV) for the breast tissue, the lymph nodes, LAD, the heart and the left lung. Treatment planning was performed in Eclipse, Varian Medical Systems Inc. Treatment plans for 50 Gy in 25 fractions were generated using 3D conformal technique with wide tangents, 6 MV or a combination of 6 and 18 MV and calculated with analytical anisotropic algorithm (AAA, version 10.0.28). The loco-regional treatment plans consisted of 5–8 and 4–9 fields for the DIBH and EIG plans, respectively. For the patients receiving treatment of the breast alone, 4–5 fields were adequate. For one patient, the 3D conformal technique was not adequate to provide an acceptable plan due to anatomy complexity and IMRT plans were generated on both scans.
Constraints for target coverage and OARs sparing followed the national guidelines of the Danish Breast Cancer Cooperative Group (www.dbcg.dk) and all plans were clinically acceptable. For the purposes of this study, dose coverage was analysed in terms of mean dose to the breast CTV (Dmean, CTV), as well as the relative volume receiving more than 95% of the prescribed dose (V95%, CTV). When the IMN were included in the target volume (19 of 24 patients) the relative volume receiving 90% of the prescribed dose was extracted (V90%, IMN). The peri-clavicular and axiliar lymph nodes were omitted in this evaluation as they were assumed to be less affected by the respiratory motion than the breast CTV and IMN. Hot spots in the plans were reported as the volume receiving more than 107% of the prescribed dose (V107%, body) corresponding to a dose of 53.5 Gy. The absolute volume of the left lung (Vleft lung), as well as the relative volume of the lung receiving 20 Gy or more (V20 Gy, left lung), were reported. The heart was retrospectively contoured on all patients as the dose received by the heart and the LAD are not necessarily correlated [Citation14]. The exposure of the cardiovascular structures was reported as the maximum dose to the LAD (Dmax, LAD), the mean dose to the heart (Dmean, heart) and as the volume receiving more than 25 Gy (V25 Gy, heart).
Reproducibility of the respiratory signals
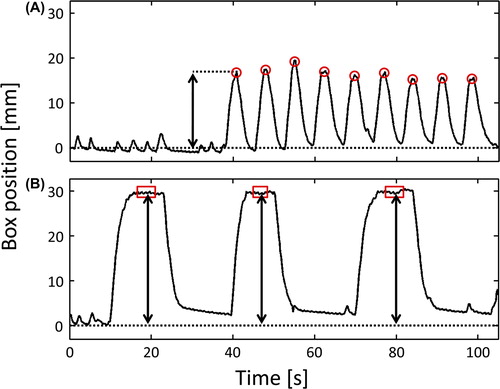
Twenty-one patients were treated in DIBH using daily orthogonal kV images synchronised with respiratory management (DIBH or EIG). Of these, 19 patients were audio coached without visual feedback for one minute prior to nine treatment sessions (most commonly session 2, 3, 4, 12, 13, 14, 22, 23 and 24) where the breathing traces, detected as external surface motion of the RPM marker box, were registered. The patients were then treated using a DIBH strategy, and these DIBH breathing signals were included in the analysis. All EIG and DIBH signals were imported into in-house software for the analysis. illustrates how the inspiration levels were determined in either case. For the EIG signals, the maximum value for each enhanced inspiration was found and for each EIG session, the mean and standard deviation (SD) were determined. For the DIBH signals, the mean value of the central part (corresponding to the middle 60%) of each breath hold was found and a SD of these means was determined for each DIBH session. Hereby both intra- and interfraction variations were included in the analysis. For each patient the SDs were compared using the Wilcoxon signed rank-sum test.
Figure 2. Respiration curves collected during the one minute of audio-coached EIG (A) and the subsequent treatment in DIBH with visual feedback (B). The red circles in (A) shows the extracted maxima for the EIG curve and the red squares in (B) shows the interval from which the mean inspiration level for a breath hold is calculated. The arrows indicate the inspiration level extracted for the analysis. The inspiration level was found for all enhanced inspirations and all breath holds). The dotted line is the baseline of the respiration. These curves were obtained for the same patient at the same treatment session (22nd fraction).
Results
Respiration monitoring and compliance
The duration of EIG coaching was approximately 30 minutes and maximum 10 minutes for DIBH. Three patients were not able to cooperate with either EIG or DIBH to a reproducible extent and these patients were therefore treated in uncoached free breathing. The age of the three patients was 88, 81 and 67 years, respectively. One patient (35 years old) was not able to hold her breath long enough to complete a DIBH scan, but she was able to follow the audio instructions and was successfully scanned and treated in EIG. The mean age for the patients scanned with both EIG and DIBH was 48 years (range 29–68). All in all, of 28 patients evaluated, 24 were judged DIBH-compliant and 25 were judged EIG-compliant.
Treatment planning
Eleven of the 24 patients included in the analysis were referred to adjuvant radiotherapy for breast cancer after mastectomy and 13 after lumpectomy. The plans were evaluated on the basis of CTV coverage as well as dose the lung and the LAD, and the overall clinically superior plan was chosen at the discretion of the treating oncologist. The DIBH plan was judged to be equivalent or superior to the EIG plan for 21 patients while the EIG plan was deemed superior to the DIBH plan for the remaining three patients.
The volume of the left lung was significantly higher in DIBH (mean 2286 cm3) compared to EIG (mean 1982 cm3) with a mean increase of 11% (p < 0.0004, range –10–41%). This indicated that patients achieved a deep level of inspiration with DIBH, leading to a clinically meaningful mean decrease in the V20 Gy, left lung of 9% (p < 0.002). Values are presented in . No significant difference in the breast CTV coverage, IMN coverage or dose to LAD and the whole heart was found between the two methods (p > 0.1).
Table I. Results of the treatment planning analysis. The bold type indicates where a statistical significant difference was found (p < 0.05).
Reproducibility of the respiratory signals
Respiratory signals were collected for 19 patients treated using DIBH. For the majority of the patients, 8–9 sessions with 7–15 breathing cycles per session were recorded. Patient 18 had 11 recorded sessions, Patient 17 had only five recorded sessions due to technical issues and Patient 24 had her treatment cancelled after three recorded sessions due to newly diagnosed metastatic disease. Patient 17 and 24 were thus excluded from the reproducibility analysis. All respiration curves obtained with audio coaching were analysed. All 17 patients were treated using the 3D conformal technique.
The results are shown in . The mean inspiration level for DIBH was compared to the means of the maxima of the EIG curves: DIBH led to a clearly deeper inspiration in 13 of the 17 patients. Including all 17 patients, the change in inspiration level from EIG to DIBH was on average an increase of 32% (range –9–91%) for the mean value, corresponding to an additional 3.9 mm (measured as an excursion of the rigid marker box). The mean inspiration level was 20.5 mm and 16.6 mm for DIBH and EIG, respectively. The increase in inspiration level from IG to DIBH was significant (p < 0.002). For two of four patients with an EIG level higher than DIBH level, the difference was < 1.5%. For the remaining two the difference was 4% and 9%, respectively.
Table II. Results of the reproducibility analysis. The differences between EIG and DIBH were found to be statistically significant with the Wilcoxon sign rank test (p < 0.05). The reported mean is the average of the mean inspiration levels for all respiration curves.
For 16 of the 17 patients DIBH was more reproducible than EIG (p < 0.05). The mean SD (mean of the SD of the inspiration level averaged over all sessions) was smaller for DIBH compared to EIG (). One patient demonstrated both highly reproducible DIBH and EIG patterns (SD of 0.4 mm for DIBH and 0.5 mm for EIG). Hence for all 17 patients, the reproducibility of inspiration level with DIBH was shown to be least as good as or better than with EIG.
Discussion
Respiratory gating is offered to all patients with left-sided breast cancer and lymph node involvement and was first introduced in 2003 in our clinic. In 2003, it was considered that patient compliance was higher with EIG than DIBH. In the present study, both inspiration modalities are well tolerated by the patient group as a whole, although individual patients may have more difficulty with either one of these approaches. The oldest patient of the cohort, e.g. could perform DIBH better than EIG, but this was not sustained throughout the treatment course. This indicates that for some patients, any form of inspiration gating may be too challenging and an ungated free breathing treatment would be preferred.
Overall, patients achieved a higher level of lung inflation with DIBH, leading to a clinically meaningful lower V20 Gy, left lung. However, no additional benefit was seen for the coronary structures. One possible limitation of the study is that all patients were first trained with EIG and then introduced with DIBH: this could arguably have encouraged the patients to hold a deeper DIBH level than if they had exclusively been introduced to DIBH. However, this potential bias would only be present at the training session: during treatment, the DIBH level was always matched to that of the reference session and the recording of EIG curves before selected treatment fractions was unlikely to have an effect on the DIBH levels. In contrast to our study, Kini et al. [Citation12] have reported a deeper inspiration level when using audio instructions compared to visual feedback, though they did not use a breath hold approach. In our study, visually guided DIBH ensured a more reproducible level of inspiration than audio-coached EIG; this supports that DIBH is well tolerated by most patients throughout the whole treatment course. Kini et al. [Citation12] also report a more reproducible amplitude with visual feedback. It should be noted that user friendliness and availability of visual guidance equipment has greatly improved during the last decade. For instance, the equipment used in this study consisted of small video goggles destined for recreational purposes. Also, with mature gating software, the additional time spent on the accelerator and in the CT scanner for either gating technique is modest.
Alternative techniques for monitoring of DIBH levels include spirometry-based systems [Citation15,Citation16] or more recently, surface imaging techniques [Citation17,Citation18]. It has also been suggested that a voluntary DIBH without visual feedback or any form of respiration monitoring might be feasible, as long as a proper daily IGRT strategy is in place to deal with interfraction variation [Citation19]. In our experience, however, patients found the visual feedback helpful and the treatment personnel at our institution reported a smoother workflow when the patient was regulating her own inspiration levels compared to audio-coached EIG, as most fields could be delivered within one single DIBH. It should be emphasised that image guidance is still essential before treatment to ensure the proper positioning of the patient, regardless of respiratory management [Citation20].
A considerable advantage of a DIBH approach over EIG is that more monitor units can be delivered without beam interruption: a typical DIBH of 20 s can be used to deliver 200 MUs, while with EIG the beam is interrupted every 10–30 MUs, depending on the patient's respiratory pattern and the width of gating window. Because beam-on interruptions can be limited, DIBH makes respiratory management more compatible with the use of enhanced dynamic wedges or the delivery of inversely optimised modulated plans [Citation21].
In conclusion, visually guided DIBH led to a deeper and more reproducible inspiration level than audio-coached EIG. DIBH resulted in a significantly larger lung volume and lower V20 Gy for the ipsilateral lung but no difference in dose coverage of the target or sparring of coronary structures. These findings support the choice of visually guided DIBH as an optimal strategy for breathing-adapted radiotherapy for patients with left-sided breast cancer.
Supplementary Appendix 1–2
Download PDF (1.1 MB)Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Darby SC, Ewertz M, McGale P, Bennet AM, Blom- Goldman U, Brønnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 2013;368:987–98.
- Grantzau T, Mellemkjær L, Overgaard J. Second primary cancers after adjuvant radiotherapy in early breast cancer patients: A national population based study under the Danish Breast Cancer Cooperative Group (DBCG). Radiother Oncol 2013;106:42–9.
- Korreman SS, Pedersen AN, Nøttrup TJ, Specht L, Nyström H. Breathing adapted radiotherapy for breast cancer: Comparison of free breathing gating with the breath-hold technique. Radiother Oncol 2005;76:311–8.
- Pedersen AN, Korreman S, Nyström H, Specht L. Breathing adapted radiotherapy of breast cancer: Reduction of cardiac and pulmonary doses using voluntary inspiration breath-hold. Radiother Oncol 2004;72:53–60.
- Remouchamps VM, Vicini FA, Sharpe MB, Kestin LL, Martinez AA, Wong JW. Significant reductions in heart and lung doses using deep inspiration breath hold with active breathing control and intensity-modulated radiation therapy for patients treated with locoregional breast irradiation. Int J Radiat Oncol Biol Phys 2003;55:392–406.
- Korreman SS, Pedersen AN, Aarup LR, Nøttrup TJ, Specht L, Nyström H. Reduction of cardiac and pulmonary complication probabilities after breathing adapted radiotherapy for breast cancer. Int J Radiat Oncol Biol Phys 2006; 65:1375–80.
- Korreman SS, Pedersen AN, Josipović M, Aarup LR, Juhler-Nøttrup T, Specht L, et al. Cardiac and pulmonary complication probabilities for breast cancer patients after routine end-inspiration gated radiotherapy. Radiother Oncol 2006;80:257–62.
- Nissen HD, Appelt AL. Improved heart, lung and target dose with deep inspiration breath hold in a large clinical series of breast cancer patients. Radiother Oncol 2013;106:28–32.
- Johansen S, Vikström J, Hjelstuen MHB, Mjaaland I, Dybvik KI, Olsen DR. Dose evaluation and risk estimation for secondary cancer in contralateral breast and a study of correlation between thorax shape and dose to organs at risk following tangentially breast irradiation during deep inspiration breath-hold and free breathing. Acta Oncol 2011;50:563–8.
- Hjelstuen MHB, Mjaaland I, Vikström J, Dybvik KI. Radiation during deep inspiration allows loco-regional treatment of left breast and axillary-, supraclavicular- and internal mammary lymph nodes without compromising target coverage or dose restrictions to organs at risk. Acta Oncol 2012;51:333–44.
- Vikström J, Hjelstuen MHB, Mjaaland I, Dybvik KI. Cardiac and pulmonary dose reduction for tangentially irradiated breast cancer, utilizing deep inspiration breath-hold with audio-visual guidance, without compromising target coverage. Acta Oncol 2011;50:42–50.
- Kini VR, Vedam SS, Keall PJ, Patil S, Chen C, Mohan R. Patient training in respiratory-gated radiotherapy. Med Dosim 2003;28:7–11.
- Nielsen MH, Berg M, Pedersen AN, Andersen K, Glavicic V, Jakobsen EH, et al. Delineation of target volumes and organs at risk in adjuvant radiotherapy of early breast cancer: National guidelines and contouring atlas by the Danish Breast Cancer Cooperative Group. Acta Oncol 2013;52: 703–10.
- Aznar MC, Korreman SS, Pedersen AN, Persson GF, Josipovic M, Specht L. Evaluation of dose to cardiac structures during breast irradiation. Br J Radiol 2011;84:743–6.
- Sixel KE, Aznar MC, Ung YC. Deep inspiration breath hold to reduce irradiated heart volume in breast cancer patients. Int J Radiat Oncol Biol Phys 2001;49:199–204.
- Swanson T, Grills IS, Ye H, Entwistle A, Teahan M, Letts N, et al. Six-year experience routinely using moderate deep inspiration breath-hold for the reduction of cardiac dose in left-sided breast irradiation for patients with early-stage or locally advanced breast cancer. Am J Clin Oncol 2013; 36:24–30.
- Gierga DP, Turcotte JC, Sharp GC, Sedlacek DE, Cotter CR, Taghian AG. A voluntary breath-hold treatment technique for the left breast with unfavorable cardiac anatomy using surface imaging. Int J Radiat Oncol Biol Phys 2012;84: 663–8.
- Cerviño LI, Gupta S, Rose MA, Yashar C, Jiang SB. Using surface imaging and visual coaching to improve the reproducibility and stability of deep-inspiration breath hold for left-breast-cancer radiotherapy. Phys Med Biol 2009;54: 6853–65.
- Betgen A, Alderliesten T, Sonke J-J, Van Vliet-Vroegindeweij C, Bartelink H, Remeijer P. Assessment of set-up variability during deep inspiration breath hold radiotherapy for breast cancer patients by 3D-surface imaging. Radiother Oncol 2013;106:225–30.
- Korreman SS, Juhler-Nøttrup T, Persson GF, Navrsted Pedersen A, Enmark M, Nystrom H, et al. The role of image guidance in respiratory gated radiotherapy. Acta Oncol 2008;47:1390–6.
- Nicolini G, Vanetti E, Clivio A, Fogliata A, Cozzi L. Pre-clinical evaluation of respiratory-gated delivery of volumetric modulated arc therapy with RapidArc. Phys Med Biol 2010;55:347–57.
