Abstract
Background. Recently, the Quantitative Analysis of Normal Tissue Effect in the Clinic (QUANTEC) Group defined dose-volume constraints for the parotid glands to avoid severe xerostomia. The aim of this study was to determine if application of these QUANTEC criteria also protected against moderate-to-severe patient-rated xerostomia. Material and methods. The study population consisted of 307 head and neck cancer patients treated with primary (chemo)radiotherapy, either with 3D-CRT (56%) or with IMRT (44%). All patients participated in a standard follow-up program in which radiation-induced toxicity and quality of life were prospectively assessed. Patients who met the QUANTEC criteria were classified as low risk and otherwise as high risk. Results. In total, 41% of the patients (treated with 3D-CRT and IMRT) were classified as low risk patients. In the group treated with 3D-CRT and IMRT, it was possible to meet the QUANTEC criteria in 47% and 32% of the patients, respectively. Sparing the parotid glands with IMRT was considerably more difficult in patients with lymph node metastases and in patients with nasopharyngeal and oropharyngeal tumours. Low risk patients reported significantly less moderate-to-severe xerostomia than high risk patients. However, the predicted risk of elderly patients and patients with pre-existing minor patient-rated xerostomia at baseline was > 20%, even when the QUANTEC criteria were met. Conclusions. Significantly lower rates of radiation-induced patient-rated xerostomia were found among low risk patients treated according to the QUANTEC criteria, but these criteria do not completely protect against xerostomia. Particularly in elderly patients and patients already suffering from minor xerostomia at baseline, the QUANTEC criteria do not sufficiently protect against persistent, moderate-to-severe patient-rated xerostomia.
Introduction
Radiotherapy is a commonly used treatment modality in the management of head and neck cancer (HNC) patients. When treating patients with radiotherapy, co-irradiation of normal tissues is generally unavoidable.
Based on the results of a number of randomised controlled trials (Citation1,Citation2) showing that salivary dysfunction can be prevented by using intensity modulated radiotherapy (IMRT) instead of conventional radiation techniques, IMRT has become the standard of care for patients with HNC who are treated with radiotherapy. Nevertheless, parts of the salivary glands still receive considerable radiation doses even when IMRT is used, resulting in hyposalivation and subsequent xerostomia (Citation3).
Recently, the QUANTEC (Quantitative Analyses of Normal Tissue Effects in the Clinic) Group suggested practical guidelines to reduce the toxicity risk based on dose constraints to be used in IMRT treatment planning (Citation4). More specifically, the QUANTEC Group concluded that severe xerostomia, defined as long-term stimulated salivary flow < 25% of baseline, can be reduced if at least one parotid gland is spared with a mean dose of less than 20 Gy or if both glands are spared with a mean dose of less than < 25 Gy (Citation5).
Recently, Moiseenko et al. (Citation6) reported the results of a prospective study which was performed to validate these QUANTEC recommendations with regard to salivary flow. When the QUANTEC criteria were met, the rate of grade 4 xerostomia, defined as 25% reduction of pretreatment salivary flow measured at 3 months was > 40% but indeed improved to less than 20% at 12 months. The authors therefore concluded that the QUANTEC recommendations were sufficiently valid to be used in clinical practice.
However, the QUANTEC criteria are only based on the dose to the parotid glands. Although parotid gland dysfunction plays an important role in the development of patient-rated xerostomia (Citation7), it is not the only prognostic factor. We recently showed that age and baseline xerostomia were independent prognostic factors for patient-rated xerostomia, in addition to the mean dose to the parotid glands (Citation7). As previous studies have shown that the correlation between salivary flow and patient-rated xerostomia is relatively weak (Citation2,Citation8), it is important to investigate the value of the QUANTEC criteria for patient-rated xerostomia as well.
Therefore, the purpose of the current study was twofold: 1) to test the hypothesis that the application of the QUANTEC criteria is sufficient to prevent patient-rated moderate-to-severe xerostomia, and 2) to determine the extent to which this effect depends on age and the presence of baseline patient-rated xerostomia.
Material and methods
Patients
The study population of the current analysis was composed of 307 patients, including 171 patients treated with 3D-CRT and 136 patients treated with IMRT. All patients met the following eligibility criteria: (Citation1) HNC originating in the oral cavity, oropharynx, larynx, hypopharynx, nasopharynx, paranasal sinuses or cervical lymph node metastases from unknown primary tumours; (Citation2) treated with curative radiotherapy (RT), either alone or in combination with chemotherapy (CHRT) or cetuximab; (Citation3) no previous surgery, radiotherapy and/or chemotherapy; (Citation4) no previous malignancies; (Citation5) no distant metastases; (Citation6) health-related quality of life (HRQoL) assessments available prior to, 6 weeks after treatment and at 6 months after completion of RT or CHRT, and (Citation7) no moderate-to-severe xerostomia at baseline. Patients with moderate-to-severe complaints at baseline were excluded from the analysis as we were primarily interested in xerostomia induced by the radiation treatment itself. The demographic and tumour characteristics are listed in . The majority of patients were male (74%) and the mean age of the study population was 62 years. The range was 32 to 92 years.
Table I. Patient characteristics.
The study was performed according to the regulations of the local ethical committees.
Treatment
In all patients, a planning CT-scan with contrast- enhancement was performed in treatment position. Radiotherapy was delivered using a 6 MV linear accelerator. The target volumes for the initial fields and boosts were similar, as previously described (Citation7). In summary, the clinical target volume of the initial field (CTV1) was composed of the primary tumour and pathological lymph nodes plus a 1.0 cm margin, and the elective nodal areas on both sides of the neck. The CTV for the boost irradiation (CTV2) consisted of the primary tumour and pathological lymph nodes with a 0.5 cm margin. In all cases, a 0.5 cm margin was applied for the planning target volumes (PTV1 and PTV2).
The parotid glands were contoured according to the guidelines described by Van de Water et al. (Citation9). All parotid glands were contoured by an expert in head and neck radiation oncology.
When treated with 3D-CRT, no attempts were made to spare the salivary glands. Patients with early laryngeal carcinoma were treated with a fraction dose of 2.5 Gy (5 times/week) up to a total dose of 60 Gy in 5 weeks or with a fraction dose of 2.0 Gy (5 or 6 times/week) up to a total dose of 66 Gy. In these patients, only the primary site was irradiated.
Patients treated with concomitant CHRT were treated with conventional fractionation (2.0 Gy per fraction, 5 times per week, up to 70 Gy in 7 weeks). In case of primary radiotherapy of the more advanced cases, which were considered ineligible for CHRT, an accelerated schedule with concomitant boost technique was used, alone or combined with cetuximab. These patients were generally treated with 6 fractions per week, with a second fraction on Friday afternoon and with a minimum interval of 6 hours, up to a total dose of 70 Gy in 6 weeks. Most patients received bilateral elective irradiation of the neck nodes to a total dose of 46 Gy, and a boost to the primary tumour and pathological lymph nodes to a total dose of 70 Gy. In some cases, radiotherapy with only conventional fractionation was used.
When treated with IMRT, the mean dose to both parotid glands was reduced as much as possible without compromising the required dose to the target volumes. Patients were treated with both a sliding window technique and step-and-shoot IMRT. A seven-field equidistant, non-opposing beam configuration was used. All patients were treated with a simultaneous integrated boost (SIB) technique. PTV1 was treated with 35 fractions of 1.55 Gy up to a total dose of 54.25 Gy. The PTV2 was treated with 35 fractions of 2 Gy up to a total dose of 70 Gy. All treatment plans were produced by Pinnacle version 9.0 (Philips, Madeson) using a collapsed cone algorithm taking into account dose inhomogeneities.
The standardised follow up programme
Since 1997, all patients referred for radiotherapy for HNC to the department of Radiation Oncology of the VU University Medical Center, Amsterdam, the Netherlands (VUMC), were included in a standardised follow up program (SFP). Since March 2007, a similar SFP was established at the department of Radiation Oncology of the University Medical Center Groningen, Groningen, the Netherlands (UMCG). Essentially, the SFP includes prospective evaluation of toxicity and HRQoL on a routine basis, prior to, during and at regular intervals after curative RT or CHRT (Citation7). HRQoL was assessed using the head and neck cancer module EORTC QLQ-H&N35 (Citation10). For this study, we used only the xerostomia item.
Endpoints
Patient-rated xerostomia was assessed at baseline, weekly during treatment, 6 weeks after treatment and every 6 months up to 24 months after treatment. A 4-point Likert scale was used (none, a bit, quite a bit, a lot). Patients with quite a bit to a lot of xerostomia were classified as having moderate-to-severe complaints.
Statistics
The patients included in this analysis were divided into two groups (high risk and low risk) based on the criteria described by the QUANTEC Group (Citation5): patients with at least one parotid gland receiving less than 20 Gy and/or both parotids glands receiving less than 25 Gy were classified as low risk patients. All other patients were classified as high risk patients.
Differences in proportions between groups were compared using a chi-square test. Changes over time were calculated for each group and were tested for statistical significance using the McNemar test. P-values below 0.05 were considered statistically significant.
An additional multivariate logistic regression analysis was performed on the group of patients with a complete follow-up of 24 months. This was done because we were also interested in the influence of age and minor xerostomia symptoms at baseline in the development of patient-rated xerostomia over time. In a previous study we showed that patients’ age and minor xerostomia at baseline are both independent risk factors in the development of patient-rated xerostomia at 6 months after treatment (Citation7). This separate analysis therefore enabled us to test if the QUANTEC criteria were sufficient to protect against moderate-to-severe patient-rated xerostomia among patients with and without baseline symptoms and how this depended on age. A predicted risk below 20% for an individual patient was considered successful for the QUANTEC criteria.
In addition to the analysis on the value of the QUANTEC criteria to prevent patient-rated xerostomia, we performed an additional analysis on the proportion of patients in which the QUANTEC criteria could be met when treated with IMRT.
All analyses were performed with SPSS for Windows (version 16.0; SPSS, Chicago, Il).
Results
Proportion of patients meeting the QUANTEC criteria
In total, 41% of the patients (treated with 3D-CRT and IMRT) were classified as low risk patients. In the group treated with 3D-CRT and IMRT, it was possible to meet the QUANTEC criteria in 47% and 32% of the patients, respectively.
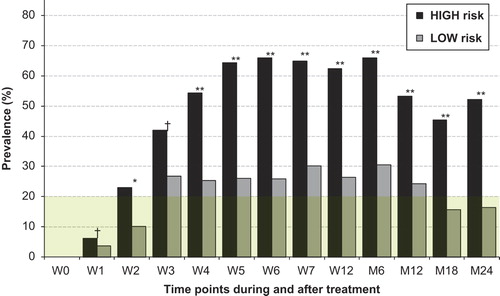
Patient-rated xerostomia (EORTC QLQ-HN35)
shows patient-rated xerostomia over time stratified by risk group. From week 4 during radiation up to 24 months after treatment, patients in the high risk group reported significantly more xerostomia compared to those in the low risk group. Between 6 and 24 months after treatment, significant recovery was observed in the low risk as well as in the high risk patients. Ultimately, in the low risk group, the prevalence of moderate-to-severe patient-rated xerostomia after 12 months of follow up was less than 20%.
Proportion of patients meeting the QUANTEC criteria when using IMRT
In the group of patients treated with IMRT (136 patients), the average mean dose to the ipsilateral and contralateral parotid glands was 34.1 Gy (SD ± 14.8 Gy) and 28.0 (SD ± 11.8) Gy, respectively. Ultimately, the QUANTEC criteria were met in 44 patients (32%), including 35 patients (26%) who received a mean dose below 20 Gy to both parotid glands. Of the 44 low risk patients, 35 patients (74%) received a dose of less than 20 Gy to one of the parotid glands, while all 44 low risk patients received less than 25 Gy to both parotid glands.
Patients in the high risk group had significantly more positive lymph nodes, had significantly more tumours located in the oropharynx and nasopharynx and were treated significantly more frequently with bilateral irradiation. Significantly fewer laryngeal tumours and unknown primary tumours were observed in the high risk group ().
Table II. Differences in baseline characteristics of the IMRT treated patients classified as low risk versus IMRT treated patients classified as high risk.
Patient-rated xerostomia and the role of age and minor xerostomia at baseline
In the multivariate logistic regression analysis of patients with a complete follow-up up to 24 months after completion of treatment (n = 132; ), the significant predictors for patient-rated xerostomia at 6 months, 12 months and 24 months after treatment were the QUANTEC criteria, increasing age and baseline xerostomia.
Table III. Odds ratios (OR) for potential risk factors in the development of patient-rated xerostomia for patients completed a follow up of 24 months after treatment.
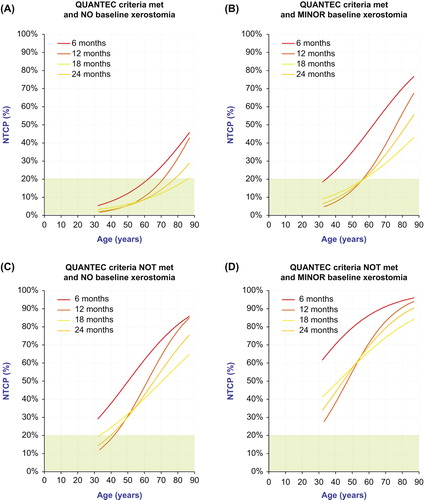
For patients without any xerostomia prior to treatment and in which the QUANTEC criteria were met, the risk of persistent moderate-to-severe xerostomia beyond 6 months of follow up was less than 20%, except for the very old patients, over 70 years of age (). However, in patients with minor xerostomia symptoms before treatment, the risk threshold of 20% or less for moderate-to-severe xerostomia was only attained among patients under 55 years of age (). When the QUANTEC criteria were not met, the risk of moderate-to-severe xerostomia was below 20% in only the very young patients (< 40 years) without baseline complaints ( and ).
Figure 2. Predicted risk for patient-rated moderate-to-severe xerostomia (EORTC QLQ-HN35) at 6, 12, 18 and 24 months after for different categories; QUANTEC criteria (met vs not met) and baseline xerostomia (none vs minor) as function of increasing age. All curves are based on a multivariate logistic regression analysis for 132 patients with a complete follow up of 24 months.
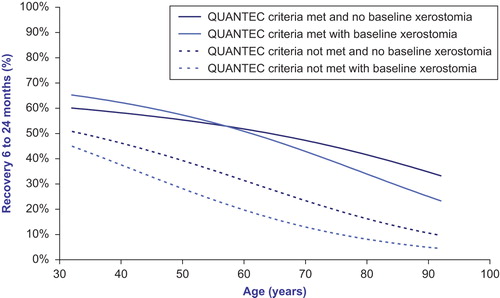
Younger patients without baseline complaints who also met the QUANTEC criteria showed a higher percentage of recovery than elderly patients ().
Figure 3. Percentage of recovery of moderate-to-severe xerostomia as a function of age, stratified by the 4 risk group categories shown in . The results are based on multivariate logistic regression analysis using the data of 132 patients with a complete dataset at all time points. The curves indicate the estimated percentages of patients with moderate to severe xerostomia 6 months after completion of treatment that will have been recovered at 24 months. Younger patients show higher percentages of recovery than elderly patients. Patients in whom the QUANTEC criteria were met show higher percentages of recovery than in whom they were not met.
Discussion
The purpose of this study was 1) to test the hypothesis that the application of the QUANTEC criteria are useful to prevent patient-rated moderate-to- severe xerostomia, and 2) to determine the extent to which this effect depends on age and the presence of baseline patient-rated xerostomia. The current study indeed showed that patients who met the QUANTEC criteria had significantly lower rates of patient-rated moderate-to-severe xerostomia. These results are in line with those previously reported by Lee et al. where patients treated according to the QUANTEC guidelines reported less patient-rated xerostomia 12 months after treatment (Citation11).
Main difference between our study and the study of Moiseenko et al. is that the current study focused on patient-rated xerostomia instead of stimulated parotid flow as a result of irradiation of the parotid glands (Citation6). Based on the findings of that study it was stated that the QUANTEC criteria are valid as a guideline to reduce the incidence of grade 4 xerostomia in terms of stimulated parotid flow.
In a previous paper we reported on the influence of increasing age and minor patient-rated xerostomia at baseline on moderate-to-severe patient-rated xerostomia at 6 months after completion of treatment (Citation7). In the current study, we confirmed that these factors were also predictive for moderate-to-severe patient-rated xerostomia at later time points. In addition, we found that the QUANTEC criteria were significantly associated with this endpoint at later time points, but that these criteria were not sufficient to protect against moderate-to-severe xerostomia in many patients who meet the QUANTEC criteria.
This applies especially to elderly patients and those with pre-existing minor complaints of xerostomia. A possible explanation for these findings is that elderly patients generally have more co-morbidity and thus use more medication, both of which may reduce saliva production (Citation12). Moreover, the capacity to recover from radiation-induced damage to the normal tissues may be reduced in elderly patients, which is supported by the shape of the curves in and . These curves clearly show that a much higher percentage younger patients reported less severe xerostomia than elderly patients. also showed that patients with “QUANTEC criteria met and no baseline xerostomia” had less recovery than “QUANTEC criteria met with baseline xerostomia” patients in the young age group and over 57 years of age recovery crossover. This illustrates that the influence of age (< 57 years) on recovery of xerostomia after treatment is greater than the influence of minor complaints of xerostomia at baseline. These findings are in line with those reported by Ghezzi et al., who showed that the secretory reserve capacity of the major salivary glands decreases with age. Elderly patients are therefore more vulnerable to xerostomia due to their reduced secretory reserve (Citation13). The probable cause is that radiation-induced salivary dysfunction results from the loss of parotid gland stem cells and that the number of stem cells decreases with age (Citation14).
Moreover, despite the use of IMRT it was possible to meet the QUANTEC criteria in only 32% of the patients. In the present study, we identified some subsets of patients in which it was more difficult to spare the parotid glands with IMRT, in particular patients being treated for oropharyngeal and nasopharyngeal carcinoma, those being treated with bilateral irradiation and patients with lymph node metastases. This is mainly due to major overlap of the PTV with larger parts of the parotid glands. Conversely, the parotid glands could be adequately spared in a much higher proportion of patients with laryngeal carcinoma, unilateral irradiation, N0 disease and lymph node metastases from unknown primary tumours.
A possible explanation for these findings is that the quality of IMRT given at our departments was poor and could be further improved. However, we have been using similar dose constraints for the parotid glands in the patients included in this analysis. Moreover, the results in our series are quite similar to those reported elsewhere (Citation1,Citation2). For instance, Nutting et al. (Citation1) recently published the results of a prospective randomised study, in which 47 patients were treated with IMRT. In that study, the average mean doses to the ipsilateral and contralateral parotid glands were of 47.6 Gy and 25.4 Gy, respectively. These doses are more or less similar to those observed in the IMRT treated patients (35.2 Gy and 28.0 Gy to the ipsilateral and contralateral parotid gland, respectively), but it has to be emphasized that in our study patients received a higher total dose to PTV2 than the patients in the cohort of Nutting et al.(Citation1). In our study, patients were treated with 35 fractions and 54.25 Gy to PTV1 and 70 Gy to PTV2, compared to 54 Gy and 65 Gy in 30 fractions when treated with primary IMRT as reported by Nutting et al. For post- operative therapy, the total dose to PTV2 was even lower than 60 Gy, which might explain the differences between our study and that of Nutting et al. In another study, in which patients with nasopharyngeal carcinoma were treated with IMRT (Citation2), the average mean dose to the parotid glands was 32.2 Gy. In our population, these average dose levels were much higher in the subset of nasopharyngeal cancer patients: 56.0 Gy and 44.7 Gy to the ipsilateral and contralateral gland, respectively. However, Kam et al. only included patients with T1 and T2 tumours and with unilateral disease (N1). In our study, 6 of the 7 patients treated for nasopharyngeal tumours had stage N2 or N3 neck disease and all had advanced T-stages, which might explain the higher average mean dose to the parotid glands in nasopharyngeal cancer patients.
Due to the above findings, the question arises as to whether other radiation delivery techniques are more effective at sparing the parotid glands without compromising the dose to the PTV. Van de Water et al. (Citation15) recently showed that the dose to the parotid glands could be reduced even further in approximately 70% of oropharyngeal cancer patients by using spot scanning protons. The possible benefits of using protons instead of photons was described for swallowing disorders after radiotherapy treatment for head and neck cancer (Citation16). In line with swallowing disorders patients could also benefit from protons in the protection of patient-rated xerostomia. The use of protons instead of photons is subject of further research, in particular in the subsets of patients in which the QUANTEC criteria cannot be met.
Based on the findings of the present study, it appears that with IMRT it is more difficult to spare the parotid glands than with 3D-CRT, which is actually not true. The 3D-CRT cohort also included patients who were locally irradiated for early laryngeal cancer, while the patients treated with IMRT had more extensive disease and were treated more often with bilateral neck irradiation. This affected the parotid glands move severely.
In conclusion, the dose constraints recommended by the QUANTEC group have prognostic value with regard to patient-rated moderate-to-severe xerostomia. When these criteria can be met, the risk of this side effect drops below 20%, except in elderly patients and patients with pre-existing, although minor, complaints of xerostomia prior to treatment. Unfortunately, the QUANTEC criteria in this study could only be met in a minority of patients. New radiation delivery techniques to further reduce the dose to the relevant salivary glands are therefore required, which we suggest as a topic for future research.
Funding: No funding
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol 2011;12:127–136.
- Kam MK, Leung SF, Zee B, Chau RM, Suen JJ, Mo F, et al. Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol 2007;25:4873–4879.
- Jellema AP, Slotman BJ, Doornaert P, Leemans CR, Langendijk JA. Impact of radiation-induced xerostomia on quality of life after primary radiotherapy among patients with head and neck cancer. Int J Radiat Oncol Biol Phys 2007; 69:751–760.
- Bentzen SM, Constine LS, Deasy JO, Eisbruch A, Jackson A, Marks LB, et al. Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC): an introduction to the scientific issues. Int J Radiat Oncol Biol Phys 2010; 76:S3–9.
- Deasy JO, Moiseenko V, Marks L, Chao KS, Nam J, Eisbruch A. Radiotherapy dose-volume effects on salivary gland function. Int J Radiat Oncol Biol Phys 2010;76:S58–S63.
- Moiseenko V, Wu J, Hovan A, Saleh Z, Apte A, Deasy JO, et al. Treatment Planning Constraints to Avoid Xerostomia in Head-and-Neck Radiotherapy: An Independent Test of QUANTEC Criteria Using a Prospectively Collected Dataset. Int J Radiat Oncol Biol Phys 2012;82:1108–14.
- Beetz I, Schilstra C, Burlage FR, Koken PW, Doornaert P, Bijl HP, et al. Development of NTCP models for head and neck cancer patients treated with three-dimensional conformal radiotherapy for xerostomia and sticky saliva: The role of dosimetric and clinical factors. Radiother Oncol 2012; 105:86–93.
- Pow EH, Kwong DL, McMillan AS, Wong MC, Sham JS, Leung LH, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys 2006;66:981–991.
- van de Water TA, Bijl HP, Westerlaan HE, Langendijk JA. Delineation guidelines for organs at risk involved in radiation-induced salivary dysfunction and xerostomia. Radiother Oncol 2009;93:545–552.
- Bjordal K, de Graeff A, Fayers PM, Hammerlid E, van Pottelsberghe C, Curran D, et al. A 12 country field study of the EORTC QLQ-C30 (version 3.0) and the head and neck cancer specific module (EORTC QLQ-H & N35) in head and neck patients. EORTC Quality of Life Group. Eur J Cancer 2000;36:1796–1807.
- Lee TF, Fang FM. Quantitative analysis of normal tissue effects in the clinic (QUANTEC) guideline validation using quality of life questionnaire datasets for parotid gland constraints to avoid causing xerostomia during head-and-neck radiotherapy. Radiother Oncol 2013 Mar; 106:352–8.
- Leal SC, Bittar J, Portugal A, Falcao DP, Faber J, Zanotta P. Medication in elderly people: its influence on salivary pattern, signs and symptoms of dry mouth. Gerodontology 2010 Jun; 27:129–33.
- Ghezzi EM, Ship JA. Aging and secretory reserve capacity of major salivary glands. J Dent Res 2003; 82:844–848.
- Pringle S, Van der Zwaag M, Vos L, Stokman M, Van Os R, Coppes R, et al. Characterisation Of Human Salivary Gland Stem Cells To Rescue Radiation-induced Salivary Gland Damage 2011;International Society for Stem Cell Research, ISSCR annual meeting, Toronto 2011(International Society for Stem Cell Research, ISSCR annual meeting, Toronto 2011).
- van de Water TA, Lomax AJ, Bijl HP, de Jong ME, Schilstra C, Hug EB, et al. Potential Benefits of Scanned Intensity-Modulated Proton Therapy Versus Advanced Photon Therapy with Regard to Sparing of the Salivary Glands in Oropharyngeal Cancer. Int J Radiat Oncol Biol Phys 2011; 79:1216–24.
- van der Laan HP, van de Water TA, van Herpt HE, Christianen ME, Bijl HP, Korevaar EW, et al. The potential of intensity-modulated proton radiotherapy to reduce swallowing dysfunction in the treatment of head and neck cancer: A planning comparative study. Acta Oncol 2013;52: 561–9.