Abstract
Background. The aim of this study was to investigate the impact of structured exercise with jaw mobilizing devices on trismus and its effect on trismus symptomatology and health-related quality of life (HRQL) in head and neck (H&N) cancer patients. Material and methods. Fifty patients with H&N cancer and trismus, i.e. maximum interincisal opening (MIO) ≤ 35 mm participated in a structured intervention program with jaw exercise. The patients in the intervention group underwent a 10-week exercise program with regular follow-up. A control group comprising of 50 patients with trismus and H&N cancer were matched to the intervention group according to gender, tumor location, tumor stage, comorbidity and age. HRQL and trismus-related symptoms were assessed. Results. The mean MIO improvement was 6.4 mm (4.8–8.0) and 0.7 (−0.3–1.7) mm in the intervention group and control group respectively, three months post-intervention commencement (p < 0.001). The intervention group demonstrated a statistically significant improvement in Role functioning, Social functioning and Global quality of life (EORTC QLQ C30) and in all Gothenburg Trismus Questionnaire (GTQ) domains, i.e. jaw-related problems (p < 0.001), eating limitation (p < 0.05) and muscular tension (p < 0.001). Conclusion. We found that a structured jaw exercise program was effective and improved the mouth opening capacity significantly. The objective effect on trismus (MIO) was also reflected in the patient-reported outcome questionnaires where the patients who underwent the structured exercise program after cancer treatment reported improvements in HRQL and less trismus-related symptoms compared to the control group.
Reduced ability to open the mouth (trismus) is a common symptom in head and neck (H&N) cancer patients. It can be caused by the tumor itself or arises as a complication after H&N cancer surgery and/or radiation therapy. Trismus affects many aspects of daily life such as eating; chewing, swallowing, dental hygiene and impairs necessary dental or surgical management. As a consequence, trismus can lead to malnutrition and weight loss [Citation1]. Patients with trismus and H&N cancer also report pain; depressive symptoms and an overall impaired health-related quality of life (HRQL) [Citation1–4].
The definition of trismus as proposed by Dijsktra, i.e. maximal interincisal opening (MIO) ≤ 35 mm, is widely used in the research on trismus in H&N cancer patients and has facilitated the comparison and evaluation of results from different studies and interventions [Citation5].
Two recent studies, using the definition of trismus of MIO ≤ 35 mm, have revealed that trismus is a common side effect after oncological treatment, with an incidence of trismus of 38–42% in H&N cancer patients [Citation4,Citation6]. Trismus can be caused by radiation-induced fibrosis, post-surgical scarring, tumor growth or muscle spasm affecting the muscles of mastication and surrounding tissues [Citation7]. High radiation dosages that affect the pterygoid and masseter muscles seem to particularly influence the development of trismus [Citation8–10].
Patients with tumors of the oral cavity and oropharynx are at high risk of developing trismus [Citation1]. Trismus evolves most rapidly during the first nine months after the radiation therapy and can then continue to progress over several years [Citation11].
Today there is no consensus on how to treat trismus related to H&N cancer. Three retrospective studies have found evidence that jaw mobilizing devices such as the Therabite® or the Dynasplint system® are useful and effective in the treatment of trismus [Citation12–14]. However, these studies do not have a prospective design, do not include any patient- reported outcome (PRO) and mostly have small patient numbers.
A recent review by Cousin et al. assessed the literature for studies on eating and drinking difficulties with the focus on the impact of HRQL amongst H&N cancer patients. The study concluded that past and present research has not yet investigated both the patient reported outcome and the more traditional endpoints such as MIO, measured in millimetres [Citation15]. Hence, there are few available data regarding outcome of rehabilitation and treatment of trismus in relation to the patients experience and reported HRQL.
Subsequently, the aim of this prospective intervention study was to investigate the impact of a structured exercise program with jaw mobilizing devices on trismus in H&N cancer patients and its effect on trismus symptomatology and HRQL.
Methods
Subjects
All patients with H&N malignancies from five medical centers serving the region of Western Sweden were identified at the multidisciplinary tumor conference held weekly. Patients newly diagnosed with H&N cancer between 2007 and 2012 were asked to participate in the study.
Inclusion criteria were treatment with radiation therapy ± chemotherapy. Patients with tumor colli were also included and underwent lymph node removal. Patients with a recurrent H&N tumor, poor general health, difficulties in filling out questionnaires and edentulous patients were excluded from the study.
Patients living in Gothenburg were regularly followed up and underwent detailed clinical evaluation by one single oral surgeon. Those who developed trismus after H&N cancer treatment were invited to attend an intervention program for treatment of trismus. In the case of co-existing acute mucositis or painful mouth symptoms, the patients started the intervention as soon as their oral status allowed. For logistical reasons, only patients living in Gothenburg were included in the intervention group. The control group was comprised of patients living outside the Gothenburg catchment area and was matched according to gender, tumor location, tumor stage, comorbidity, radiation dosage and age.
The control group followed the standard regional hospitals schedule for follow-up visits according to their local guidelines, which included regular MIO measurements by the hospital dentist. No structured intervention program addressing trismus existed in the region during the time period but any amount of exercise, any device used or attempt of improving the mouth opening performed in the control group was registered by the study coordinator.
Ethics
The study was approved by the Regional Ethical Review Board at Gothenburg University and performed in accordance with the Declaration of Helsinki. All participants gave their informed consent to participate in the study.
Endpoints and assessment
The primary endpoint in this study was MIO and secondary endpoints were trismus-related symptoms and HRQL before and after treatment. A multidimensional study protocol was used to evaluate functional outcomes before and after the trismus exercise program. The protocol included MIO, weight, height, socio-demographic data, treatment regimens, tumor classification and comorbidity. The patients’ comorbidity was assessed using the Adult Comorbidity Evaluation 27(ACE-27) method [Citation16]. TNM-classification and tumor stage were retrieved according to the system of classification determined by International Union against cancer (UICC) [Citation17].
Maximum interincisal opening (MIO)
The criterion for trismus of MIO ≤ 35 mm suggested by Dijsktra et al. was used [Citation5].
MIO were measured using a ruler with the patient in an upright position. MIO was measured as the maximal distance between the edges of the incisors of the mandible and the maxilla, expressed in millimetres.
Trismus intervention
The exercise program consisted of a 10-week structured exercise program with exercise five times per day. The program consisted of three steps: 1) warm up movements consisting of jaw opening 10 times and small sideway movements of the jaws 10 times without using the jaw device; 2) passive stretching, with the jaw mobilizing device, 30 seconds (if possible), repeated five times; 3) five repetitions of active exercise (bite towards resistance). Patients were instructed to relax in between the sessions. Furthermore, the patients were instructed to gradually increase the amount and intensity of the exercises to avoid pain or injury. During the program the patients were evaluated by an oral surgeon with measurement of MIO after four and 10 weeks and in addition, three months after intervention commencement.
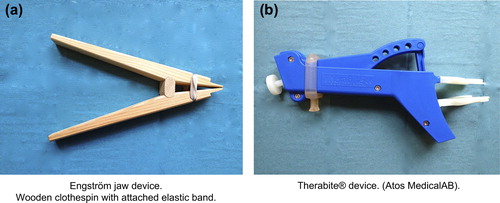
The patients in the intervention group were randomized into two exercise groups; one using the Therabite® and one using the Engström jaw mobilizing device (). The jaw exercise devices are placed in between the teeth of the maxilla and the mandible and when the patient squeeze the handles of the device it assist the opening of the jaw. The patients received written and oral instructions and the device was demonstrated to the patient by an oral surgeon.
Patient reported outcome (PRO)
Gothenburg Trismus Questionnaire (GTQ). Gothenburg Trismus Questionnaire (GTQ) is a newly developed validated symptom-specific trismus questionnaire. GTQ is well accepted by patients, has satisfactory compliance with low rates of missing items and has shown good psychometric properties (validity and reliability). The GTQ contains 21 items; with 13 items divided into the three domains: jaw-related problems (six items), eating limitation (four items) and muscular tension (three items). The remaining eight items are retained as single items. The domains and single items range from 0–100, where 100 indicate maximal amount of symptoms and 0 is equal to no symptoms [Citation18].
EORTC QLQ C30 and EORTC QLQ H&N35. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ C30) is a cancer-specific questionnaire that evaluates HRQL in cancer patients [Citation19].
Calculated scale scores range from 0–100. On the function scales and Global Quality of Life (GQL) scale, a score of 100 represents maximum functioning, whereas on the symptom scales and single items, a score of 100 indicates the worst possible symptoms.
For interpretation of EORTC QLQ C30 scores and clinical significance, the guidelines developed by Cocks et al. was used were clinical significance is graded as: no difference, small difference, medium difference and large difference [Citation20].
To address additional symptoms associated specifically with H&N cancer, a complementary 35-item module was used, the EORTC QLQ-H&N35. Calculated scale scores range from 0–100. For symptom scales and single items, a score of 100 indicates the worst possible symptoms and 0 indicates no symptoms [Citation21].
We used a shortened version for presentation av data and for statistical analysis of significance including three functional scales from EORTC QLQ C30 (Role functioning, Social functioning and GQL) and three single items from H&N 35 (pain, social eating, problems with opening mouth).
Hospital Anxiety and Depression Scale (HADS). The patients also completed the Hospital Anxiety and Depression Scale (HADS), which is widely used to detect mood disorders in patients with somatic comorbidity [Citation22]. The HADS consists of 14 items, seven items for depression and seven items for anxiety with a score range from 0–21.
Statistical methods
For comparison between groups, Fisher's exact test was used for dichotomous variables. The Mantel-Haenszel χ2 exact test was used for ordered categorical variables and χ2 exact test was used for non-ordered categorical variables. Mann-Whitney U-test was used for continuous variables. Continuous variables are reported using mean and confidence intervals. All tests were two-tailed and conducted at 5% significance level.
Results
Patient characteristics
Fifty-one patients with trismus were enrolled in the study and asked to participate in the intervention program. One patient died before finishing the intervention program and was therefore excluded. Fifty patients completed the intervention program. Another 50 patients with H&N cancer and trismus were enrolled during the same period and matched to the intervention group. The patients in the intervention group and the matched controls were enrolled 3–6 months after receiving radiation therapy. The characteristics of the groups are presented in .
Table I. Characteristics of the intervention and control group.
In the control group, 14 of the patients received treatment for their trismus, by the regional hospital dentist. Eight of the patients used the Engström jaw device, five patients used manual stretching and one patient unspecified method. None of the patients in the control group used the Therabite device. The treatment was not conducted according to a structured exercise program.
Treatment regimes
All patients, both intervention as well as the control group, received radiation therapy. Intensity modulating radiation therapy (IMRT)-technique was used in 77 (77%) patients.
During 2007–2009 external radiation therapy was generally administered through accelerated hyper fractionated therapy as 1.7 Gy/fraction 2 times/day 5 days per week to a total dosage of 64.6 Gy. During 2010–2012 the external radiation therapy was generally administered through accelerated fractioning 2 Gy/day 1–2 times/day 5 days per week with a total of 6 treatments/week resulting in a 68 Gy dosage to the tumor.
Chemotherapy was generally given as inductive therapy, two courses of treatment with cisplatin-fluorouracil before start of the radiation therapy or as concomitant cisplatin administered weekly throughout the radiation therapy treatment. Additionally 44 (44%) patients received interstitial radiation therapy or brachytherapy. Eight (8%) of the patients underwent radical neck dissection in addition to radiation therapy.
MIO
The intervention group had lower mean MIO before the intervention and higher mean MIO after intervention compared to the control group, both statistically significant as per . At the three-month follow-up, the mean MIO improvement was 6.4 mm in the intervention group and 0.7 mm in the control group. Thirty-seven patients (74%) in the intervention group no longer fulfilled the trismus diagnostic criteria compared to 16 patients (32%) in the control group.
Table II. Maximal interincisal opening (MIO) before and 3 months after intervention (10-week structured exercise program).
Patient-reported outcome (PRO)
GTQ. Before intervention there were no statistically significant differences in GTQ-scores between the intervention and control group. At the three-month follow-up there was a statistically significant difference in GTQ-scores between the groups in all three domains (jaw-related problems, eating limitations and muscular tension) and in four of eight single items indicating a decrease in trismus-related symptoms in the intervention group ().
Table III. GTQ-score, mean value, 95% confidence interval (CI) for H&N cancer patients before study group exercise and 3-month follow-up.
EORTC QLQ C30 & H&N 35. Before intervention there were no statistically significant differences in mean scores of EORTC QLQ C30 and H&N 35 in the functional scales (Role functioning, Social functioning and GQL) and single items (pain, social eating and problem with opening mouth). After the intervention at the three-month follow-up there was both a statistically and clinically significant difference in the three functional scales. Clinical significance was graded as medium according to the guidelines by Cock et al. For the single items there was a statistically significant difference in two of three single items (social eating and problem with opening of mouth) ().
Table IV. EORTC QLQ-C30 and H&N 35 (shortened version) for H&N cancer patients before and after study intervention.
HADS. For the anxiety disorder score, before intervention, 12 patients (24%) in the intervention group and 14 patients (28%) in the control group, reported a possible or probable anxiety disorder according to the HADS questionnaire. For depression, 17 (34%) in the intervention group and 17 (34%) in the control group reported possible or probable depression.
At the three-month follow-up, for the anxiety disorder score, nine (18%) of the intervention group and 15 (30%) of the control group reported possible or probable anxiety disorder.
For depression, 11 (22%) of the intervention group and 16 (32%) of the control group reported possible or probable depression. The numbers of patients reporting possible or probable anxiety or depression declined to a greater extent in the intervention group at follow-up.
Discussion
This prospective intervention study investigated the impact of structured exercise on trismus. We found that structured jaw exercise program with the Therabite® or Engström jaw mobilizing device were effective and significantly improved patients' mouth opening capacity. The objective effect on trismus (MIO) was also reflected in the PRO questionnaires where the patients who underwent a structured exercise program after cancer treatment also reported improvements in HRQL and less trismus-related symptoms to a higher extent compared to the control group.
To date there have been few prospective studies investigating the impact of exercise therapy on trismus related to H&N cancer. Buchbinder demonstrated in 1993 that it is possible to improve mouth opening in irradiated H&N cancer patients with jaw mobilizing devices and Cohen et al. suggested that jaw mobilizing exercise also could be useful in the post-operative management of H&N cancer patient undergoing surgical procedures affecting the mouth opening capacity [Citation23,Citation24].
In recent retrospective materials the impact of exercise with jaw devices such as the Dynasplint system® and the Therabite® has been investigated with results of MIO improvement varying from 5.4 to 7.0 mm, which is congruent with results from this study [Citation12–14].
However, to our knowledge there are no previous data regarding the effect of exercise on trismus in a consecutive prospective material combining MIO and PRO as endpoints.
It has been suggested that an early exercise start is favorable in the treatment of radiation-related trismus [Citation14]. Kamstra et al. reported that the odds of improvement in mouth opening were reduced if time from oncological treatment was long. This could be explained by the pathophysiology of radiation-induced damage in normal tissue, with an initial inflammatory phase and a subsequent, sometimes irreversible, atrophic and fibrotic phase [Citation25]. In the present study, time from oncological treatment to start of exercise was short, given the design that the patients were enrolled as soon as they had developed trismus, i.e. MIO ≤ 35 mm. There was no statistically significant difference in time from oncological treatment to start of study between the intervention group and the matched controls.
We found that the patients who underwent structured exercise intervention reported improvements in EORTC QLQ C30 as well as in the GTQ-item that reflects the effect of trismus on social and family activities. The results from the questionnaires suggested that exercise intervention with improved mouth opening capacity might have a positive social implication for the patients, e.g. being comfortable in eating together with other people, being able to eat normal food and being able to finish a meal within a reasonable time. Furthermore, after the exercise program, the intervention group reported improvements in the ability to work reflected in the functional scale Role functioning (EORTC QLQ C30) and in the GTQ. (Facial pain and limitation in mouth opening affecting the ability to work).
Facial pain and restricted mouth opening can affect speech and as a consequence affect the ability to work, especially in occupations where verbal communication is paramount, e.g. conducting meetings, liaising with others either personally or via telephone.
Seventy-six percent of the patients in the intervention group improved their mouth opening to a MIO > 35 mm, therefore no longer fulfilling the trismus criterion. Even though the mean MIO change after the intervention (6.7 mm) might seem small, the PRO results indicates that exercise intervention has an evident impact on the patients’ experience of mouth opening capacity with regards to fewer symptoms related to trismus and improved HRQL.
Clinical implications
According to the study results, a structured exercise program for trismus after H&N cancer treatment was effective according to objective (MIO) and subjective (PRO) measures and should be offered to patients at risk of developing trismus.
Study limitations
The follow-up time in this study was limited. Further long-term studies on the exercise effect on trismus, is needed in order to investigate outcome maintenance and possible deterioration of improvements over time. In a non-randomized controlled trial there is inevitably a risk of selection bias. The risk of selection bias has been minimized through the matching procedure in this study were factors by us known as possible bias factors were taken into account.
Conclusion
This prospective intervention study investigated the impact of structured exercise on trismus. We found that jaw mobilization exercise with Therabite® or Engström jaw device is effective and improves the mouth opening capacity significantly.
The patients who underwent structured exercise after cancer treatment reported less trismus-related symptoms and improvements in HRQL compared to a matched control group. In the future, research on preventive management of patients at high risk of developing trismus is warranted.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
This study was supported by the Swedish Cancer Society, the Research and Development Council (FoU), Va stra Go taland County, Sweden, the Assar Gabrielsson Foundation Göteborg and the Medical Faculty of Gothenburg University Sweden.
References
- Weber C, Dommerich S, Pau HW, Kramp B. Limited mouth opening after primary therapy of head and neck cancer. Oral Maxillofac Surg 2010;14:169–73.
- Lee R, Slevin N, Musgrove B, Swindell R, Molassiotis A. Prediction of post-treatment trismus in head and neck cancer patients. Br J Oral Maxillofac Surg 2012;50: 328–32.
- Louise Kent M, Brennan MT, Noll JL, Fox PC, Burri SH, Hunter JC, et al. Radiation-induced trismus in head and neck cancer patients. Support Care Cancer 2008;16: 305–9.
- Pauli N, Johnson J, Finizia C, Andrell P. The incidence of trismus and long-term impact on health-related quality of life in patients with head and neck cancer. Acta Oncol 2013;52:1137–45.
- Dijkstra PU, Huisman PM, Roodenburg JL. Criteria for trismus in head and neck oncology. Int J Oral Maxillofac Surg 2006;35:337–42.
- Johnson J, van As-Brooks CJ, Fagerberg-Mohlin B, Finizia C. Trismus in head and neck cancer patients in Sweden: Incidence and risk factors. Med Sci Monit 2010; 16:CR278–82.
- Ichimura K, Tanaka T. Trismus in patients with malignant tumours in the head and neck. J Laryngol Otol 1993;107: 1017–20.
- Teguh DN, Levendag PC, Voet P, van der Est H, Noever I, de Kruijf W, et al. Trismus in patients with oropharyngeal cancer: Relationship with dose in structures of mastication apparatus. Head Neck 2008;30:622–30.
- Goldstein M, Maxymiw WG, Cummings BJ, Wood RE. The effects of antitumor irradiation on mandibular opening and mobility: A prospective study of 58 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88: 365–73.
- van der Molen L, Heemsbergen WD, de Jong R, van Rossum MA, Smeele LE, Rasch CR, et al. Dysphagia and trismus after concomitant chemo-Intensity-Modulated Radiation Therapy (chemo-IMRT) in advanced head and neck cancer; dose-effect relationships for swallowing and mastication structures. Radiother Oncol 2013;106:364–9.
- Wang C-J, Huang E-Y, Hsu H-C, Chen H-C, Fang F-M, Hsiung C-Y. The degree and time-course assessment of radiation-induced trismus occurring after radiotherapy for nasopharyngeal cancer. Laryngoscope 2005;115:1458–60.
- Stubblefield MD, Manfield L, Riedel ER. A preliminary report on the efficacy of a dynamic jaw opening device (dynasplint trismus system) as part of the multimodal treatment of trismus in patients with head and neck cancer. Arch Phys Med Rehabil 2010;91:1278–82.
- Baranano CF, Rosenthal EL, Morgan BA, McColloch NL, Magnuson JS. Dynasplint for the management of trismus after treatment of upper aerodigestive tract cancer: A retrospective study. Ear Nose Throat J 2011;90:584–90.
- Kamstra JI, Roodenburg JL, Beurskens CH, Reintsema H, Dijkstra PU. TheraBite exercises to treat trismus secondary to head and neck cancer. Support Care Cancer 2013; 21:951–7.
- Cousins N, Macaulay F, Lang H, Macgillivray S, Wells M. A systematic review of interventions for eating and drinking problems following treatment for head and neck cancer suggests a need to look beyond swallowing and trismus. Oral Oncol 2013;49:387–400.
- Paleri V, Wight RG, Silver CE, Haigentz M Jr., Takes RP, Bradley PJ, et al. Comorbidity in head and neck cancer: A critical appraisal and recommendations for practice. Oral Oncol 2010;46:712–9.
- International Union Against Cancer (UICC) TNM Classification of Malignant Tumors. 7th ed. Oxford UK: Wiley-Blackwell, 2009.
- Johnson J, Carlsson S, Johansson M, Pauli N, Ryden A, Fagerberg-Mohlin B, et al. Development and validation of the Gothenburg Trismus Questionnaire (GTQ). Oral Oncol 2012;48:730–6.
- Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality- of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365–76.
- Cocks K, King MT, Velikova G, de Castro G Jr., Martyn St-James M, Fayers PM, et al. Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur J Cancer 2012; 48:1713–21.
- Bjordal K, Ahlner-Elmqvist M, Tollesson E, Jensen AB, Razavi D, Maher EJ, et al. Development of a European Organization for Research and Treatment of Cancer (Eortc) questionnaire module to be used in quality of life assessments in head and neck cancer patients. Acta Oncol 1994;33:879–85.
- Mitchell AJ, Meader N, Symonds P. Diagnostic validity of the Hospital Anxiety and Depression Scale (HADS) in cancer and palliative settings: A meta-analysis. J Affect Disord 2010;126:335–48.
- Buchbinder D, Currivan RB, Kaplan AJ, Urken ML. Mobilization regimens for the prevention of jaw hypomobility in the radiated patient: A comparison of three techniques. J Oral Maxillofac Surg 1993;51:863–7.
- Cohen EG, Deschler DG, Walsh K, Hayden RE. Early use of a mechanical stretching device to improve mandibular mobility after composite resection: A pilot study. Arch Phys Med Rehabil 2005;86:1416–9.
- Stubblefield MD. Radiation fibrosis syndrome: Neuromuscular and musculoskeletal complications in cancer survivors. Phys Med Rehab 2011;3:1041–54.