Abstract
Purpose. The purpose of this study was to examine whether or not vaginal elasticity or lack of lubrication is associated with deep or superficial dyspareunia. We investigated gynecological cancer survivors treated with radiation therapy.
Methods. In a population-based study with 616 women answering a questionnaire (participation rate 78%) and who were treated with radiotherapy for gynecological cancer, we analyzed information from 243 women (39%) who reported that they had had intercourse during the previous six months. Analyses included log-binomial regression (relative risks) and multiple imputations by chained equations in combination with Bayesian Model Averaging, yielding a posterior probability value. Age range of this cancer recurrent-free group of women was 29–80.
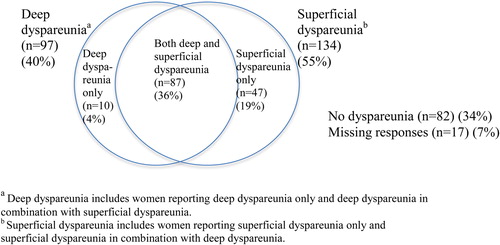
Results. Dyspareunia affected 164 of 243 of the women (67%). One hundred thirty-four women (55%) reported superficial pain, 97 women (40%) reported deep pain, and 87 women (36%) reported both types of dyspareunia. The relative risk (RR) of deep dyspareunia was 1.87 (CI 1.41–2.49) with impaired vaginal elasticity compared to normal vaginal elasticity. Age and lower abdominal swelling were separate risk factors for deep dyspareunia. However, effects remain after adjusting for these factors.
Conclusion. The relative risk of deep dyspareunia was almost twice as high with impaired vaginal elasticity compared to normal vaginal elasticity. If we wish to treat or even prevent deep dyspareunia in women with gynecological cancer, we may use our knowledge of the pathophysiology of deep dyspareunia and increasingly provide dilators together with instructions on how to use them for stretching exercises in order to retain vaginal elasticity. Results highlight the need for studies with more precise questions distinguishing superficial from deep dyspareunia so that in the future we may be able to primarily try to avoid reduced vaginal elasticity and secondarily reduce the symptoms.
It is challenging to prevent or treat that which is not understood. Women treated with radiation therapy for a gynecological cancer report a variety of physical, psychological, and social problems documented to affect quality of life, such as fecal incontinence [Citation1], lower limb lymphedema [Citation2], pain and fatigue [Citation3], emotional distress [Citation4], and problems related to sexual health [Citation5–8]. Studies have focused on women's experiences with impaired sexual health after having undergone treatment for gynecological cancer [Citation9–12]. Evidence in the literature demonstrates dyspareunia (pain with intercourse) among these women to be a common, debilitating problem as one in five women report painful symptoms with intercourse [Citation7]. These women suffer first from their long-term dysfunction [Citation13] and second, as their problems are rarely addressed by healthcare staff [Citation14]. In order to move this field forward, we need to better understand the underlying pathophysiology of dyspareunia so that we in the future may treat or even prevent it. The purpose of this study was to examine whether or not vaginal elasticity or lack of lubrication is associated with deep or superficial dyspareunia. We have used a validated questionnaire based on clinometrically atomized patient-reported outcomes [Citation15] to survey factors associated with dyspareunia in a cohort of irradiated gynecological cancer survivors and analyzed these data.
Methods
Participants
The Swedish registry system provides nearly everyone living in Sweden with a personal identity number [Citation16]. Through this system, we identified 1800 women who had received radiation treatment in the pelvic region for gynecological malignancies between March 1991 and December 2003 at Radiumhemmet Karolinska University Hospital, Stockholm, or between December 1994 and December 2003 at Sahlgrenska University Hospital, Gothenburg. Inclusion criteria were no evidence of recurrence, age < 80 years, and able to read and understand Swedish. The study was approved by respective regional ethics committee and the women gave both oral and written consent to participate.
Study preparation and data collection
We applied clinical epidemiological methods to systematically recognize the possible causes of bias in each step of the research process [Citation17]. The questionnaire used in the study was developed by our division according to a well established clinometric method focused on atomizing symptoms [Citation18–20]. Detailed information about the study-specific questionnaire and the specific treatments for this group was described by Lind et al. in a previous publication [Citation21]. The questionnaire for this study was based on interviews with gynecological cancer survivors and validated face-to-face using women within the study population, ensuring that the questions were understood the way they were intended. The questionnaire was also tested for participation rate and for rate of missing values. The questionnaire included 351 questions and was divided into different sections covering demographic data, information concerning disease and treatment, quality of life, physical symptoms of the pelvic region, and social functioning. Of these questions, 59 dealt with sexuality. Information regarding cancer diagnoses, stage of disease, and treatment techniques regarding surgery, radiation treatment, and chemotherapy was collected from medical records.
Measurements
The questions were phrased to represent the previous six months regardless of when the treatment took place and thus able to detect long-term effects. Dyspareunia was assessed by asking “During the previous six months, have you had pain in the vaginal membranes or vaginal introitus (superficial dyspareunia) during intercourse?” and “During the previous six months, have you felt pain in the vagina and in the pelvis (deep dyspareunia) with intercourse?” with anchors “No, not at all”, “Yes, a little”, “Yes, quite a bit”, and “Yes, very much”. Questions regarding dyspareunia were dichotomized into “dyspareunia” and “no dyspareunia”. Questions related to potentially associated factors were dichotomized to “no/little dysfunction” or “moderate/high dysfunction” during the previous six months. Here, only the answer “no” was classified as not having dyspareunia. For both these questions there was also an alternative to respond “Not relevant, I have not had intercourse during the previous six months”.
Questions regarding potentially associated factors were: “During the previous six months, how has your vaginal elasticity been?” with anchors “None at all”, “Poor”, “Moderate”, and “Good”. In the analyses, we classified “None at all” and “Poor” as reduced vaginal elasticity and “Moderate” and “Good” as normal elasticity. We also analyzed the question “During the previous six months, has your vagina become moist during sexual arousal?” with anchors “Not relevant, I have not been sexually aroused during the previous six months”, “No, not at all”, “Yes, a little”, “Yes, quite a bit”, and “Yes, very much”. In the analyses, the responses “No, not at all” and “Yes, a little” were classified as having reduced lubrication. Finally, “In the previous six months, during sexual arousal, have you noticed if labia, clitoris or outer parts of the vagina have felt swollen and engorged?” with anchors “Not relevant, I have not been sexually aroused during the previous six months”, “No, never”, “Yes, less than half the time when I have been sexually aroused”, “Yes, more than half the times”, and “Yes, every time”. In the analyses, we classified “No never” and “Yes, less than half the time when I have been sexually aroused” as reporting reduced genital engorgement.
Statistical analysis
Statistical analyses include descriptive statistics of the women's sociodemographic and treatment related characteristics (). We calculated the percentage of respondents in each category of the potentially associated factors with outcome and formed ratios of these percentages (relative risks) as a measure of the strength of the association between the independent variable and the outcome with 95% corresponding confidence intervals (CI) (). We analyzed the association between potentially associated factors (elasticity, lubrication, engorgement) and the outcomes of superficial and deep dyspareunia, respectively, using multiple imputations by chained equations (MICE) in combination with Bayesian Model Averaging yielding a percentage, the Posterior Probability Value (PPV). PPV values show levels of existing statistically significant associations: > 99% as very strong, 95–99% as strong, 75–95% as positive, and 50–75% as a weak association. We used multiple imputations for the following variables: marital status, parity, age, smoking, genital engorgement, vaginal lubrication, and vaginal elasticity. Calculations were performed using the SAS statistical software version 9.2 (SAS Institute Inc, Cary, NC, USA).
Table I. Demographic characteristics of gynecological cancer survivors (n = 616).
Table II. Late symptoms with intercourse during the past six months among gynecological cancer survivors treated with pelvic radiation therapy with or without surgery (n = 243).
Results
Participants
Data were collected from 616 gynecological cancer survivors (78% participation rate) treated with external radiation therapy. Of these, 243 women (39%) reported having had sexual intercourse during the previous six months (). Median time between end of radiation treatment and follow-up time was seven years for women who had had intercourse during the previous six months and eight years for those not engaging in intercourse. Time range from treatment to data collection was 3–15 years. Most survivors (90%) had been treated with surgery plus radiation treatment and the remaining had received radiation treatment only. Eighty-one percent of the women also had undergone brachytherapy. Chemotherapy treatment had been added for 33% of the women. The two largest groups of diagnoses were endometrial and cervical cancer ().
Deep and superficial dyspareunia
In the group of sexually active women (n = 243), 55% reported superficial dyspareunia, 40% reported deep dyspareunia, 36% reported both superficial and deep dyspareunia, and 34% reported no dyspareunia (, ). Sixty-one percent of the women reported not having had intercourse during the previous six months. Seven percent declined to answer the question on dyspareunia (). Of all women who reported they had had sexual intercourse, the response rates ranged from 93% to 95% for the questions regarding dyspareunia, vaginal elasticity, lubrication, and genital engorgement. Dyspareunia affected 164 of 243 women (67%). Of those who reported having had intercourse during the previous six months, 145 women (60%) reported intercourse up to twice per month, and 98 women (40%) reported intercourse more often (Data not shown in table). The relative risk of deep dyspareunia was 1.87 (1.41–2.49) with impaired patient-reported elasticity (none or poor) compared to those who reported moderate or good elasticity and the relative risk of superficial dyspareunia was 1.58 (1.29–1.93) with impaired elasticity (). Bayesian Model Averaging yielded lubrication (PPV100%) and swollen lower abdomen (PPV 87%) as variables associated with superficial dyspareunia and the variable found to be associated with deep dyspareunia was vaginal elasticity with a posterior probability of 100%) (Data not shown). Age was a separate risk factor for deep dyspareunia and both of these effects remain after adjusting for each of them separately and together (). We found no statistically significant correlation between grade of genital engorgement with arousal and dyspareunia. There was no statistically significant correlation between impaired vaginal elasticity and superficial dyspareunia after adjusting for impaired lubrication (). Nearly 50% of the respondents answered “not relevant” when possible. When no such response alternative was available, the rate of missing answers was higher. At the most, it was 20%.
Discussion
The relative risk of deep dyspareunia was almost twice as high among women who reported impaired elasticity (none or poor) compared to those who reported moderate or good elasticity. To prevent or relieve deep dyspareunia, we need to find means to increase vaginal elasticity. To prevent or relieve superficial dyspareunia, we need to find means to increase lubrication and reduce atrophy with friction being the major problem in this population of gynecological cancer survivors.
It is difficult to find comparable results in the literature since to our knowledge only one prior study has distinguished superficial dyspareunia from deep dyspareunia. In the study by Bergmark and colleagues, comprising 256 women with early stages of cervical cancer (stages IB or IIA), vaginal shortness was found to be associated with deep as well as superficial dyspareunia whereas reduced vaginal elasticity and lubrication were associated with superficial dyspareunia only [Citation7]. Several factors may explain the differences in these results. First, women's demographic characteristics differed in the two studies. In comparison with the survivors in the study presented here who were diagnosed with different types of gynecological cancer, Bergmark's data set comprised women with cervical cancer only and most of them had had surgery for cervical cancer which in itself shortens the vagina by 2–3 cm, and thus possibly, may give rise to a sense of reduced elasticity. Moreover, 158 women in Bergmark's study (61%) were treated with radiation treatment (the rest were treated with surgery only) whereas in this study, all 616 women had undergone radiation treatment. In addition, even though Bergmark's is the only identified study that has taken both superficial and deep dyspareunia into account, we are unable to exclude the possibility of misclassification as the questions in the two studies were not identical. As such, the results may not be entirely comparable.
Without fully comparable results, we reasoned that one may consider reduced vaginal length as the extreme form of reduced elasticity lengthwise, hence, with caution we may use reduced vaginal length as a proximal variable for reduced elasticity. To that end, we found a number of publications linking shortened vagina with unspecified dyspareunia [Citation8,Citation10,Citation22]. In one longitudinal study, Jensen and colleagues found persistent sexual dysfunction up to two years after radiation treatment (n = 118) [Citation8]. There was a high prevalence of dyspareunia in this group of women (50–60%), and significant differences between women treated with radiation treatment and the control group (p 0.024–< 0.001). Forty-eight percent of the women reported a smaller vaginal dimension (p = 0.002) at 12 months after end of radiation treatment in comparison with levels before the cancer diagnosis, seven of 24 (29%) reported a bothersome size of the vagina at 12 months, and four of 24 (17%) reported quite a bit to very much dyspareunia [Citation8]. However, this study did not distinguish deep dyspareunia from superficial dyspareunia. Also, the follow-up time since treatment was different from our study as Jensen and colleagues followed their survivors from termination of radiation treatment until two years later whereas the data in our study were collected at least three years or more after end of radiation treatment. Nonetheless, even though the follow-up time was different from our study, their results along with a persistent pattern of low or no sexual interest offer insight to how tightly intertwined the symptoms are in addition to the profound role they play in recovering one's sexual health after radiation treatment. We identified age, reduced lubrication, and lower abdominal swelling as potential confounders of superficial and deep dyspareunia, respectively and have thus adjusted for these in the analyses [Citation23,Citation24].
The proportion of women who reported not having had intercourse in the previous six months deserves mentioning. We do not know the reason for abstaining from intercourse. For those who have a partner, one possibility may be that they abstain as a result of previous experience with pain associated with this type of sexual activity. Fear of cancer in general [Citation25], and in particular of gynecological cancer as a threat against the most inner core of what commonly embodies a sense of being a woman, may contribute to the women avoiding intercourse altogether. Layered on this is the preconceived societal notion that older women “should not” be sexually active, thus labeling the desire for intercourse something to be ashamed of [Citation26], a stigma certainly not conducive to actively seeking support and treatment for this problem. As a result, it would be plausible if women may simply “give up trying” and opt for avoiding intercourse. Hence, we speculate that the rate of intercourse reported by the participants could reflect a population experiencing a pronounced sexual dysfunction. Indeed, the high response rate of these intimate, very private questions in this study clearly reflects that these are concerns that women regardless of age do have.
Our study is strengthened by a fairly large number of participants and a reasonably high participation rate. Using a national population-based registry, we believe that the risk for selection-induced errors was minimized. Moreover, the use of the national registry gave us full control of the denominator when calculating the participation rate. As the participants responded to our carefully designed and constructed questionnaire in private, we may likely have reduced the risk for measurement errors and as well as any interview-induced bias. Also, using detailed face-to-face validated questions concerning these symptoms shows that women are able to distinguish between superficial and deep dyspareunia. Nonetheless, there are limitations to our study. First, we cannot exclude the possibility that the results would have differed if all eligible women would have responded to the questionnaire. Second, we do not have information on important reasons for superficial dyspareunia including genital atrophy or estrogen treatment. Third, approximately half of the women reported that they had not had intercourse during the previous six months. Thus, they were included in the descriptive portion of this report however not part of the analytic part. Regardless of reason for refraining from intercourse, however, this would likely deviate the prevalence ratio towards 1.0. Fourth, this study lacks information on the frequency of dyspareunia among the women experiencing this symptom. In order to simplify for the women, we chose not to ask them the percentage of painful episodes and instead chose to ask them about the intensity (severity) of their dyspareunia. Irrespective of treatment modality, we believe that the effect of deep dyspareunia is largely mediated by vaginal elasticity. That is, aspects of treatment are not possible confounders. They are not confounders but rather associated with the independent factor of study (vaginal elasticity). Women who had not had sexual intercourse during the previous six months answered “Not relevant, I have not had sexual intercourse during the previous six months” on questions concerning reduced vaginal elasticity and deep dyspareunia. As such, we have no information from them: our finding primarily concerns women who had had sexual intercourse. For some questions, for example concerning vaginal elasticity, we overlooked to provide an anchor for women who were not sexually active. As a result, there is a higher rate of missing answers for these questions. Finally, we do not have sufficient information to evaluate hormonal status of the women in this group, a factor which well may affect a woman's vaginal atrophy and lubrication capacity [Citation27] and, thus, experience of superficial dyspareunia.
We found that deep dyspareunia was primarily associated with reduced vaginal elasticity and that superficial dyspareunia was primarily associated with reduced lubrication. One way to move this field forward is to learn how to prevent and treat reduced vaginal elasticity and reduced lubrication. If we wish to treat or even prevent deep dyspareunia in women with gynecological cancer, we may use our knowledge of the pathophysiology of deep dyspareunia and increasingly provide dilators together with instructions on how to use them for stretching exercises in order to retain vaginal elasticity. To prevent reduced lubrication for superficial dyspareunia, we may consider finding means to increase lubrication by better understanding the underlying causes of reduced lubrication. In our aim to treat reduced lubrication, however, we may consider providing information about suitable topical hormonal creams, which help to maintain the vaginal mucous membrane. In research, our results highlight the need for randomized controlled studies that aim to minimize the physical and psychological morbidity as a result of radiation treatment for gynecological cancer. One such intervention was carried out in Australia in which women were provided with dilators and the follow-up thereafter was carried out through a combination of nursing consultants and telephone peer support [Citation28] and a similar study conducted in the US [Citation29]. Results from these studies are pending but may provide needed new insight to these problems affecting thousands of women today.
Acknowledgments
We would like to thank the women who made this study possible by bravely sharing their experiences with us. This study was funded by grants from the Swedish Cancer Society, the Cancer Research Funds of Radiumhemmet, the King Gustav V Jubilee Clinic Cancer Foundation, Gothenburg, and the Swedish State under the ALF agreement, Stockholm and Gothenburg. We declare that we have no conflict of interest. The funding sources had no role in study design, data collection, data interpretation, or the writing of this article. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Dunberger G, Lind H, Steineck G, Waldenström AC, Nyberg T, al-Abany M, et al. Fecal incontinence affecting quality of life and social functioning among long-term gynecological cancer survivors. Int J Gynecol Cancer 2010;20:449–60.
- Dunberger G, Lind H, Steineck G, Waldenström AC, Nyberg T, al-Abany M, et al. Lower limb lymphedema in gynecological cancer survivors – effect on daily life functioning. Support Care Cancer 2013;21:3063–70.
- Lefkowits C, Rabow WM, Sherman EA, Kiet KT, Ruskin R, Chan JK, et al. Predictors of high symptom burden in gynecologic oncology outpatients: Who should be referred to outpatient palliative care? Gynecol Oncol 2014;132:698–702.
- Ferrandina G, Petrillo M, Mantegna G, Fuoco G, Terzano S, Venditti L, et al. Evaluation of quality of life and emotional distress in endometrial cancer patients: A 2-year prospective, longitudinal study. Gynecol Oncol 2014;133:518–25.
- Ye S, Yang J, Cao D, Lang J, Shen K. A systematic review of quality of life and sexual function of patients with cervical cancer after treatment. Int J Gynecol Cancer 2014;24:1146–57.
- Andersen BL, van Der Does J. Surviving gynecologic cancer and coping with sexual morbidity: An international problem. Int J Gynecol Cancer 1994;4:225–40.
- Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med 1999;340:1383–9.
- Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys 2003;56:937–49.
- Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Early-stage cervical carcinoma, radical hysterectomy, and sexual function. A longitudinal study. Cancer 2004;100:97–106.
- Flay LD, Matthews JH. The effects of radiotherapy and surgery on the sexual function of women treated for cervical cancer. Int J Radiat Oncol Biol Phys 1995;31:399–404.
- Park, SY, Bae DS, Nam JH, Park CT, Cho CH, Lee JM, et al. Quality of life and sexual problems in disease-free survivors of cervical cancer compared with the general population. Cancer 2007;110:2716–25.
- Frumovitz M, Sun CC, Schover LR, Munsell MF, Jhingran A, Wharton JT, et al. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol 2005;23:7428–36.
- Greimel ER, Winter R, Kapp KS, Haas J. Quality of life and sexual functioning after cervical cancer treatment: A long-term follow-up study. Psychooncology 2009;18:476–82.
- Abbott-Anderson K, Kwekkeboom KL. A systematic review of sexual concerns reported by gynecological cancer survivors. Gynecol Oncol 2012;124:477–89.
- Steineck G, Bergmark K, Henningsohn L, al-Abany M, Dickman PW, Helgason A. Symptom documentation in cancer survivors as a basis for therapy modifications. Acta Oncol 2002;41:244–52.
- Sweden S. Statistical yearbook of Sweden. Stockholm: Statistics Sweden; 2013.
- Steineck G, Hunt H, Adolfsson J. A hierarchical step-model for causation of bias-evaluating cancer treatment with epidemiological methods. Acta Oncol 2006;45:421–9.
- Kreicbergs U, Valdimarsdóttir U, Onelöv E, Henter JI, Steineck G. Talking about death with children who have severe malignant disease. N Engl J Med 2004;351: 1175–86.
- Bylund Grenklo T, Kreicbergs U, Hauksdóttir A, Valdimarsdóttir UA, Nyberg T, Steineck G, et al. Self-injury in teenagers who lost a parent to cancer: A nationwide, population-based, long-term follow-up. JAMA Pediatr 2013;167:133–40.
- Omerov P, Steineck G, Runeson B, Christensson A, Kreicbergs U, Pettersén R, et al. Preparatory studies to a population-based survey of suicide-bereaved parents in Sweden. Crisis 2013;34:200–10.
- Lind H, Waldenström AC, Dunberger G, al-Abany M, Alevronta E, Johansson KA, et al. Late symptoms in long-term gynaecological cancer survivors after radiation therapy: A population-based cohort study. Br J Cancer 2011;105:737–45.
- Noronha AF, Mello de Figueiredo E, Rossi de Figueiredo Franco TM, Cândido EB, Silva-Filho AL. Treatments for invasive carcinoma of the cervix: What are their impacts on the pelvic floor functions? Int Braz J Urol 2013;39: 46–54.
- Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Lymphedema and bladder-emptying difficulties after radical hysterectomy for early cervical cancer and among population controls. Int J Gynecol Cancer 2006; 16:1130–9.
- Beesley V, Janda M, Eakin E, Obermair A, Battistutta D. Lymphedema after gynecological cancer treatment: Prevalence, correlates, and supportive care needs. Cancer 2007;109:2607–14.
- Clarke JN, Everest MM. Cancer in the mass print media: Fear, uncertainty and the medical model. Soc Sci Med 2006;62:2591–600.
- McCallum M, Lefebvre M, Jolicoeur L, Maheu C, Lebel S. Sexual health and gynecological cancer: Conceptualizing patient needs and overcoming barriers to seeking and accessing services. J Psychosom Obstet Gynaecol 2012;33:135–42.
- Fernandes T, Costa-Paiva TH, Pinto-Neto AM. Efficacy of vaginally applied estrogen, testosterone, or polyacrylic acid on sexual function in postmenopausal women: A randomized controlled trial. J Sex Med 2014;11:1262–70.
- Schofield P, Juraskova I, Bergin R, Gough K, Mileshkin L, Krishnasamy M, et al. A nurse- and peer-led support program to assist women in gynaecological oncology receiving curative radiotherapy, the PeNTAGOn study (peer and nurse support trial to assist women in gynaecological oncology): Study protocol for a randomised controlled trial. Trials 2013;14:39.
- Decruze SB, Guthrie D, Magnani R. Prevention of vaginal stenosis in patients following vaginal brachytherapy. Clin Oncol (R Coll Radiol) 1999;11:46–8.