Abstract
To compare adverse effects and toxicity in men with high-risk or locally advanced prostate cancer when adding intensity-modulated radiotherapy (IMRT) technique to the pelvis.
Patients and methods. In this prospective follow-up study 180 patients treated with conformal radiotherapy (RAD) to the prostate and vesiculae seminales (boost volumes; PV) and long-term androgen deprivation therapy (LADT), were compared to 90 patients managed by LADT, RAD to the PV and additionally pelvic IMRT. Adverse effects were self-reported at baseline, at 3- and 12-month follow-up. At each time point, the patients rated a questionnaire covering urinary, bowel, and sexual function and bother, quality of life, fatigue, and mental distress.
Results. At 3-month follow-up urinary and bowel functions were significantly decreased among IMRT compared to RAD. At 12-month follow-up both groups showed the same reductions within the urinary, bowel and sexual domains. RAD patients had more mental distress than IMRT patients. The scores on quality of life, fatigue and mental distress hardly influenced function or bother within the urinary, bowel or sexual domains.
Conclusions. Men treated for high-risk or locally advanced prostate cancer with a combination of LADT, RAD and IMRT including PV and pelvic structures had considerably more acute side effects at 3 months than men treated with LADT and RAD to the PV only. However, at 12-month follow-up, the observed genitourinary and gastrointestinal function and bother were similar in both groups.
Despite improvements in long-term outcome for patients with high-risk localized (PCa) and locally advanced prostate cancer (LAPC) [Citation1,Citation2], inclusion of the pelvis in the radiation field remains a matter of debate [Citation3–5] both due to the fear of increased toxicity and lack of unambiguous evidence for clinical benefit. The documentation of adverse effects concerning urinary, bowel and sexual function and bother addressing the patient's perspective with established questionnaires are often not sufficiently embedded in former studies. Contemporary series showed only moderate increase in treatment-induced toxicity in the combined treatment group applying radiotherapy (RAD) to the whole pelvis [Citation1,Citation6]. However, in studies introducing modern conformal RAD techniques have led to substantial reduction of patient-rated adverse effects in men with PCa and LAPC [Citation7,Citation8].
Still, there is obviously reluctance in the oncological community to encompass pelvic structures and thereby increase the field size. At many institutions only conformal RAD to the prostate/vesiculae seminales (target volumes; PV) is considered. Alternatively, these patients are treated with long-term androgen deprivation therapy (LADT) only for assumed systemic disease [Citation9]. As a consequence, a substantial number of patients with LAPC could be potentially undertreated, counteracting the aim of local control [Citation10].
Currently, most patients with LAPC receive LADT combined with a conventional radiation dose. So far, several studies in men with high-risk or LAPC have shown lower rates of acute adverse effects to the gastrointestinal and genitourinary system when applying modern intensity-modulated radiotherapy (IMRT) [Citation11–13].
However, enlarging the field size by including pelvic structures could potentially increase the risk of developing adverse effects [Citation9,Citation13]. Therefore, sufficient follow-up time and patient-based reports are essential for assessment of adverse effects when introducing new treatment approaches. The purpose of this prospective follow-up study was to study self-reported adverse effects by encompassing pelvic structures into the treatment volume used by IMRT and IMRT/RAD to the PV and to compare the results to those of conformal RAD to the PV only, while both groups getting LADT.
Changes over three time points of self-assessed function and bother in the urinary, bowel and sexual domains (from baseline to 3- and 12-month follow- up) were studied. We hypothesized that function and bother at 12 months in the pelvic irradiation treatment sample (IMRT) would be similar to those reported previously by Stensvold et al. [Citation14] in patients treated with conformal RAD.
Patients and methods
Sample characteristics
This study only concerns the patients treated with IMRT or RAD who filled in the questionnaires at baseline, 3-, and 12-month follow-up.
IMRT patients
Sampling and criteria. The IMRT cohort has been described recently [Citation15]. Initially, 120 patients were eligible according to the protocol, however, 30 patients deviated from the protocol: 16 were not invited by their doctor, 11 did not return the questionnaire, two died shortly after inclusion and one received irradiation to the prostate only. Therefore the IMRT group consisted of 90 patients. The IMRT protocol was approved by the local Ethics Committee, and all patients gave written informed consent.
In addition to the anatomical grading using the TNM/UICC stage classification [Citation16], the inclusion criteria were: Age < 75 years, no previous invasive cancer, initial PCa diagnosis made during the last 6 months, pN+ M0 or a calculated N+ risk ≥ 15% using the Memorial Sloan-Kettering Cancer Center nomogram [Citation17] and prognostic high-risk disease defined by D’Amico's classification [Citation18]. During the recruitment period a trend towards radiographic N- assessment was seen due to inappropriate lymph node sampling when applying lymphadenectomy [Citation19].
IMRT planning and delivery. The CTV for the pelvic nodes was delineated by contouring a 0.7 cm radial area around the pelvic iliac vessels and adding a margin to planning target volume. The medial portion of the presacral nodal area was left out in the delineation of lymph nodes, aiming to spare the recto- sigmodeum, otherwise the countering was much alike the recommendation by the Radiation Therapy Oncology Group Web site (http://www.rtog.org.). At the initiation of the study no clear consensus for lymph node irradiation was available. The upper external iliac vessel delineation also included the lateral presacral nodal chain and the upper part of the sacral (S1–S2). However, delineation of the pelvic lymph nodes was modified and slightly deviated from the today's ASTRO-guidelines due to practice to perform surgical obturatorius staging at that time and the expected low risk of lymph node affection in this area (< 10%).
The rectum was delineated from the anus to the rectosigmoid flexure. In the approved IMRT protocol predefined protocol-stated dose constraints to the OARs were mandatory. The use of three-dimensional (3D) CRT and IMRT in PCa permits dose escalation strategies with improved sparing of normal tissue. The following dose constraints as stated in our IMRT protocol were used: 70 Gy or more and 60 Gy or more to maximum 30% and 50%, respectively, of the volume of the rectum, and 70 Gy or more and 65 Gy or more to maximum 20% and 50%, respectively, of the volume of the bladder.
Inverse planning software was applied (Nucleotron, Veenendal, The Netherlands). Treatment plans were generated by seven coplanar fields to the delineated pelvic structures up to a total dose of 50 Gy encompassing the prostate and vesiculae seminales (target volumes; PV), by use of 15-MV photon beams. Radiation of the boost volume (24 Gy to the seminal vesicles and the prostate for T3b; 24 Gy to the prostate for ≤ T3a) was done by a four-field box technique. Patients were instructed to empty the rectum and keep the bladder filled during the course of RAD. The radiation dose was described at the isocenter according to the International Commission on Radiation Units and Measurements Reports 62 (ICRU Report 62, www.icru.org).
RAD patients
Sampling and criteria. Between December 2004 and July 2007 there was carried out a study of all patients who received curative treatment for PCa at Department of Oncology, and Oncological Surgery, Oslo University Hospital, Radiumhospitalet [Citation20]. The study was approved by the regional committee for medical ethics, and all patients gave written informed consent. For this study the sub-sample of patients (N = 180) with high-risk disease according to D’Amico was used [Citation18]. The inclusion criteria were similar to the IMRT patients: Age < 75 years, no previous invasive cancer and initial PCa diagnosis made during the last 6 months.
RAD planning and delivery. Patients in the high-risk group were treated with conformal four-field box radiation technique to the target volumes (50 Gy to the seminal vesicles and prostate and boost 24 Gy to the prostate for ≤ T3a or 24 Gy to the prostate and seminal vesicles for T3b). Like for IMRT, the rectum was delineated from the anus to the rectosigmoid flexure and patients were instructed to empty the rectum and keep the bladder filled during the course of RAD.
ADT. All patients started neo-adjuvant ADT 6 months prior to IMRT, and this treatment was continued to a maximum of 2.5 years in some patients with pN+ and a prognostic high-risk profile. We applied a 3-month depot injection with gosereline (Zoladex® 10.8 mg sc). As prophylaxis against flare-ups, bicalutamide 50 mg × 1 orally was given for 30 days, beginning 1 week prior to first injection of gosereline. All patients received the questionnaire at pre-treatment (baseline) and again at 3- and 12-month follow-up. Acute toxicity was defined as a time period up to 90 days after finished radiation.
Questionnaire instruments and variables
The UCLA-PCI. With a time frame of the last 4 weeks [Citation21] the patients reported on function (several items) and bother (1 item) in the urinary, bowel and sexual domains. The scoring alternatives were: no problem (5), very small problem (4) small problem (3), moderate problem (2) and big problem (1). The scorings were converted to scales ranging from 100 (no bother, maximum function) to 0 (maximum bother, minimum function) according to established algorithms. Functions and bother were considered as continuous variables.
The Hospital Anxiety and Depression Scale (HADS). The HADS consists of seven items each on the anxiety and depression sub-scales. The item scores range from 0 (not present) to 3 (highly present) last week, so the sub-scale scores range from 0 (low) to 21 (high) [Citation22].
The Fatigue Questionnaire (FQ). The FQ contains 11 items covering mental and physical fatigue items the last 4 weeks each rated from 0 (as before) to 3 (very much more). The total fatigue score ranges from 0 to 33, with higher scores implying more fatigue [Citation23,Citation24].
The UCLA-PCI, the HADS and the FQ showed adequate internal consistency with Cronbach's coefficient ≥ 0.65 at baseline.
The Short Form 12 (SF-12). The SF-12 questionnaire covers physical and mental quality of life (QoL), expressed as the Physical (PCS) and Mental Composite Summary scores (MCS). Based on T-transformations of the scorings, the mean PCS and MCS scores in the general Norwegian male population are 50 points. One standard deviation covers 10 points [Citation25,Citation26].
Other variables. Current paired relationship meant being married or cohabiting versus non-paired relationships, level of basic education was dichotomized into low (< 13 years) and high (≥ 13 years) and current work status was dichotomized into paid work versus not in paid work.
Somatic co-morbidity was recorded if one or more of the diseases covered by the UCLA-PCI were present at baseline.
Statistics
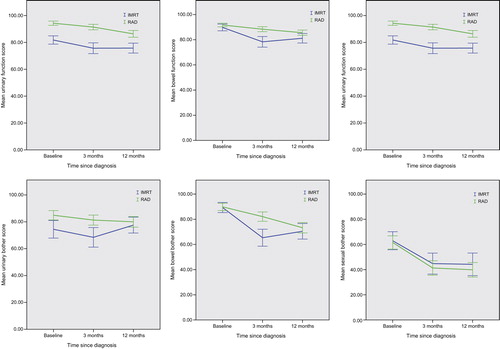
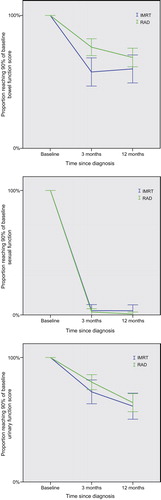
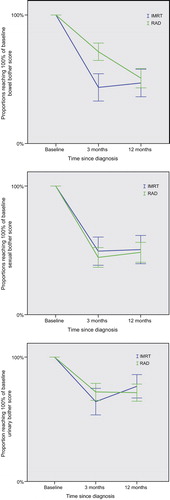
The statistical assessment used for our study has been comprehensively published recently [Citation14]. In short, cross-sectional differences between the IMRT and RAD groups were analyzed with t-tests for continuous variables, and in case of skewed distributions the Mann Whitney U-test was used. Categorical differences were analyzed with χ2-tests. For longitudinal analyses paired sample t-tests were used to analyze the changes in function and bother scores at the three time points. Outcomes were also assessed according to Malcolm et al. [Citation27] by the proportion of patients who reached 90% of their baseline function scores (PBS-90) at the post-treatment time points. In agreement with Malcolm et al. patients with a baseline function score < 30 were excluded from the analyses because they could have a high PBS-90 with a low absolute score. Accordingly, bother patients with baseline score < 25 were excluded for the same reason. The cut-off < 25 for bother was chosen since bother was rated with single questions for urine, bowel and sexuality that are converted to (0–25–50–75–100).The proportion of patients who had returned to 100% of their baseline bother score (PBS-100) were calculated at 3- and 12-month follow-up [Citation27]. The 95% confidence intervals were shown on the group scores of the figures. show the mean scores of function and bother in the IMRT and RAD groups, while show the proportions reaching PBS-90 of function. depict the proportions reaching PBS-100 of bother. Due to technical reasons the carry a note of information. A p-value < 0.05 was regarded as statistically significant, and all tests were two-sided. The data were analyzed with the PASW 18.0 software.
Results
Characteristics of the samples
No significant differences were observed concerning demographic variables and duration of ADT between the IMRT and the RAD groups (). As for mental health and QoL, the RAD group showed a significantly higher level of anxiety compared to the IMRT group. Concerning PCa-related variables the IMRT group showed higher mean PSA level, higher clinical tumor stage, a higher proportion with Gleason score > 7, and a lower proportion lymph nodes without malignancy ().
Table I. Demographic and clinical characteristics at baseline of the IMRT sample (N = 90) and the RAD sample (N = 180).
Changes of function and bother mean scores over time (longitudinal analyses)
For the IMRT group mean urinary, bowel and sexual function scores were significantly reduced from baseline to 3-month follow-up, and they did not improve significantly from 3 to 12 months (). In contrast, the mean function scores of the RAD group were significantly reduced from baseline to 3 months and then became further significantly reduced at 12-month follow-up. These patterns of changes over time concerning function mean scores are depicted in .
Table II. Mean function and bother scores of IMRT and RAD patients at baseline, 3- and 12-months follow-up.
In the IMRT group sexual and bowel bother were significantly increased (lower values) from baseline to 3-month follow-up, with small changes from 3 to 12 months. Urinary bother followed with significant increase at 3 months and then significant decrease of bother from 3 to 12 months.
The RAD group showed another pattern in which urinary and sexual bother both were significantly increased (lower mean values) from baseline to 3 months, but with no further changes from 3 to 12 months. In contrast bowel bother showed significant further increase between 3 and 12 months. These patterns of changes over time concerning function and bother mean scores are depicted in .
The proportions of patients who returned to ≥ 90% of their baseline function scores at 3- and 12-month follow-up are shown in . In the IMRT group we observed for all functions a significant reduction at 3 months compared to baseline and no significant change from 3 to 12 months. The same pattern was found for the urinary, bowel and sexual function in the RAD group.
Table III. Return rates to 90% baseline score for functions and 100% bother scores in IMRT and RAD patients at 3- and 12-months follow-up.
For bother we studied return to 100% of baseline level. In the IMRT group 51% of the patients had returned to baseline level of sexual bother at 3 months and for bowel bother the proportion was 44%. These proportions were minimally higher at 12 months. In contrast, 66% of the patients had regained urinary baseline bother level at 3 months and 77% at 12 months. In the RAD group baseline level was reached at 3 months by 73% for urinary bother and 72% for bowel bother. Urinary bother was stabile to 12 months, while the proportion reaching baseline for bowel bother at 12 months was significantly lower (51%). Forty-five percent of the patients reached baseline for sexual bother at 3 months with closely the same percentage at 12 months (48%).
These patterns of changes over time concerning function and bother mean scores are depicted in .
Cross-sectional comparisons of the IMRT and RAD groups
When compared cross sectionally at every time points the IMRT group had significantly lower urinary function scores than the RAD group, and the urinary bother was significantly higher in the IMRT group at baseline and 3 months (). Bowel function was significantly lower in the IMRT group at 3- and 12-month, and bowel bother higher at 3 months compared to the RAD group. No between-group differences were observed concerning sexual function or bother at any time points.
The only significant finding between group differences were observed at 3 months when the IMRT group had significantly lower proportion reaching baseline level for bowel bother (IMRT 44% vs. RAD 72%, p < 0.05).
Differences in psychosocial variables between the IMRT and RAD groups
Longitudinal findings. Anxiety, fatigue, and QoL (PCS-12 and MCS-12) showed significant changes over time in both the IMRT and RAD groups, while that was not the case for depression in any of the groups ().
Table IV. Psychosocial scores in IMRT and RAD patients at baseline, 3- and 12-month follow-up.
Cross-sectional data. The level of anxiety was higher in the RAD group compared to IMRT group at all time points. At 3 months the IMRT group showed significantly better mental and physical QoL.
Adjusted findings and findings at 12 months
We adjusted the significance between-group differences shown in for the significance between group variables shown in . Adjustment made no changes concerning the significance between-group differences shown in .
Discussion
The current study represents to our knowledge the first comprehensive report on the patients’ self-rating perspective on function and bother when adding IMRT to the pelvis with conformal RAD to the boost volume compared to conformal RAD to the PV only. All patients received LADT. Our hypothesis of no significant differences in adverse effects between the IMRT and RAD groups at 12-month follow-up was partially supported as significant between-group differences were observed for urinary and bowel functions only. Using the proportion of return to baseline calculation method, the hypothesis was fully supported since no significant differences in adverse effects were found. The fear of additional toxicity in patients referred to pelvic irradiation due to enlarge treatment volumes and the risk of accumulative toxicity after pelvic lymph node dissection is a real matter of concern in daily RAD practice. The logic behind our study was to detect any increase in unacceptable short- and longer term toxicity in our IMRT-cohort.
Taking a longitudinal perspective on mean scores in the IMRT group most functions showed a significant reduction and most bother a significant increase from baseline to 3-month follow-up with no further significant changes from 3 to 12 months. The only exception concerned urinary bother that improved significantly from 3 to 12 months. In contrast the RAD group showed further reduction in function and increase in bother from 3 to 12 months, the exceptions being urinary and sexual bother. The proportions of return to baseline methods showed significant change from baseline to 3 months but not further on to 12 months for all functions and bothers in the IMRT group, and the same pattern in the RAD group except for urinary function and bowel bother that both became significantly worse from 3 to 12 months.
Sanda et al. [Citation28] among others investigated the impact of ADT duration as an essential factor on sexual function and QoL. They reported long-lasting symptoms and worse bowel and sexual QoL scores 2 years after RAD than baseline scores. In our sample, patients in both groups had impaired sexual function and increased bother during follow-up possibly due to LADT.
The distribution of more advanced cancer to the IMRT-cohort than in the RAD group may reflect the intention of the protocol to introduce a new radiation technique without possibly increased harm to the patients. This concept might have had influenced the attitude of the patients enrolled into this study. As seen, mental QoL actually improved significantly at both 3 and 12 months and was better in the IMRT cohort compared to RAD group. The positive influence of regular visits may be supported by the finding of decreased anxiety in the IMRT group compared to the RAD group throughout the observation period. This result might be biased by a follow-up schedule in the IMRT cohort encountering trained personal at the clinic to support coping strategies and the fact that treatment for a prognostically poor cancer has taken place. Physical QoL in contrast was significantly increased at 3 months perhaps for the same reason, while as reduced functions drag on a significant reduction is seen from 3- to 12-month follow-up.
One year with follow-up may be sufficiently representative to detect the major adverse effect profiles in men treated with RAD. In one of our recent studies Stensvold et al. could show that function scores at 6 months were significantly associated with function scores at 24 months [Citation29].
Our results are comparable to published series using IMRT to the target volumes [Citation7] and more favorable compared to studies involving non-IMRT techniques to the whole pelvis. In contrast to Pervez et al. we did noticed a decline in urinary function from baseline to 1-year follow-up [Citation8]. Interestingly, the decrease in this domain was not equivalently transformed with substantial bother at follow-up.
One major restrictive issue for implementation of pelvic irradiation is the possible risk of increased adverse effects. In a previous study Pinkawa and colleagues compared clinician rated adverse effects after whole pelvic to prostate-only RAD [Citation4]. They found a significant decline in bowel function scores in the acute and chronic phase after encompassing pelvic structures compared to those receiving limited prostate irradiation. In contrast, in our study patients receiving IMRT including the pelvis had more reduced bowel function and bother during the acute phase, but the situation improved considerably at 12-month follow-up. At that time point the patients had improved mean scores in the bowel domain. Thus, it is not unreasonable to presume that the introduction of a better conformal technique as done by IMRT contributed to the seen improvement. Still, we have to acknowledge that many centers are now using IMRT to the prostate as a standard rather than four-field treatment. Since we applied conformal RAD in both groups to the PV our study is not biased but one could expect in general less toxicity using IMRT compared to our results.
Summarized, in our work the acute urinary and bowel-associated adverse effect profiles as rated by patients were significantly increased for the IMRT group and less in the conformal RAD group. The phase of acute adverse effects lasted for a couple of months in the former but improved during the 6- and 12-month period. Persisting urinary, bowel and sexual side effects resembled both groups at 1-year follow-up. Similar, patient-reported bother in the urinary or bowel domain was declining more rapid in the IMRT group, but at last follow-up these patients had not more reduced QoL compared to men treated with RAD. In light of our results it appears safe to introduce pelvic irradiation for men with LAPC, but outcome data have to support an eventual general recommendation. So far our experience with enlarged fields using a modern RAD technique can pave the way for more pro-active inclusion of areas with potential spread beyond the primary tumor in those patients.
Strength and limitations
In our previous study about adverse affects and IMRT we found by attrition analysis that our results could probably be extended to our whole sample [Citation15]. Further, reliability of our approach is supported by the used of established instruments with well-documented psychometric properties. In addition, we obtained psychosocial variables from all patients. Our patients stayed with us through the study period since most of them did their ratings at every time point. However, our results have to be considered in the light of some limitations. Our sample is considerable, but not large. The study was designed to assess adverse effects and without regard for oncological outcomes. This will be done in a planned future project.
Conclusion
On the whole, the adverse side effect profiles in patients on LADT with LAPC including pelvic structures applying IMRT and RAD to the target volumes are very similar to that observed in limited field irradiation in high-risk patients applying RAD and LADT. Still, patients report more bother in the acute phase for urinary and bowel domain despite of IMRT technique. Regularly follow-ups and rigorous intervention seem to be beneficial in these patients.
Acknowledgments
We also thank study nurse Melanie-Birte Schulz for excellent study coordination.
The support of the study by a grant from the Olav Raagholt and Gerd Meidel Foundation, and from The Norwegian Cancer Society is greatly appreciated.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Warde P, Mason M, Ding K, Kirkbride P, Brundage M, Cowan R, et al. Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: A randomised, phase 3 trial. Lancet 2011;378:2104–11.
- Widmark A, Klepp O, Solberg A, Damber JE, Angelsen A, Fransson P, et al. Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): An open randomised phase III trial. Lancet 2009;373:301–8.
- Nguyen PL, D’Amico AV. Targeting pelvic lymph nodes in men with intermediate- and high-risk prostate cancer despite two negative randomized trials. J Clin Oncol 2008;26: 2055–6.
- Pinkawa M, Piroth MD, Holy R, Djukic V, Klotz J, Krenkel B, et al. Combination of dose escalation with technological advances (intensity-modulated and image-guided radiotherapy) is not associated with increased morbidity for patients with prostate cancer. Strahlenther Onkol 2011; 187:479–84.
- Morikawa LK, Roach M, III. Pelvic nodal radiotherapy in patients with unfavorable intermediate and high-risk prostate cancer: Evidence, rationale, and future directions. Int J Radiat Oncol Biol Phys 2011;80:6–16.
- Fransson P, Lund JA, Damber JE, Klepp O, Wiklund F, Fossa S, et al. Quality of life in patients with locally advanced prostate cancer given endocrine treatment with or without radiotherapy: 4-year follow-up of SPCG-7/SFUO-3, an open-label, randomised, phase III trial. Lancet Oncol 2009; 10:370–80.
- Lips I, Dehnad H, Kruger AB, van MJ, van der HU, Battermann J, et al. Health-related quality of life in patients with locally advanced prostate cancer after 76 Gy intensity-modulated radiotherapy vs. 70 Gy conformal radiotherapy in a prospective and longitudinal study. Int J Radiat Oncol Biol Phys 2007;69:656–61.
- Pervez N, Krauze AV, Yee D, Parliament M, Mihai A, Ghosh S, et al. Quality-of-life outcomes in high-risk prostate cancer patients treated with helical tomotherapy in a hypofractionated radiation schedule with long-term androgen suppression. Curr Oncol 2012;19:e201–10.
- Aizer AA, Yu JB, McKeon AM, Decker RH, Colberg JW, Peschel RE. Whole pelvic radiotherapy versus prostate only radiotherapy in the management of locally advanced or aggressive prostate adenocarcinoma. Int J Radiat Oncol Biol Phys 2009;75:1344–9.
- Sridharan S, Warde P. The importance of local control in high-risk locally advanced prostate cancer. Curr Oncol 2012;19:S6–12.
- Al-Mamgani A, Heemsbergen WD, Peeters ST, Lebesque JV. Role of intensity-modulated radiotherapy in reducing toxicity in dose escalation for localized prostate cancer. Int J Radiat Oncol Biol Phys 2009;73:685–91.
- Peschel RE, Colberg JW. Surgery, brachytherapy, and external-beam radiotherapy for early prostate cancer. Lancet Oncol 2003;4:233–41.
- Zelefsky MJ, Levin EJ, Hunt M, Yamada Y, Shippy AM, Jackson A, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2008;70:1124–9.
- Stensvold A, Dahl AA, Brennhovd B, Smastuen MC, Fossa SD, Lilleby W, et al. Bother problems in prostate cancer patients after curative treatment. Urol Oncol 2013;31: 1067–78.
- Lilleby W, Stensvold A, Dahl AA. Intensity-modulated radiotherapy to the pelvis and androgen deprivation in men with locally advanced prostate cancer: A study of adverse effects and their relation to quality of life. Prostate 2013;73: 1038–47.
- Wittekind C, Compton CC, Greene FL, Sobin LH. TNM residual tumor classification revisited. Cancer 2002;94: 2511–6.
- Roach M, III, Weinberg V, Nash M, Sandler HM, McLaughlin PW, Kattan MW. Defining high risk prostate cancer with risk groups and nomograms: Implications for designing clinical trials. J Urol 2006;176: S16–20.
- D’Amico AV, Moul J, Carroll PR, Sun L, Lubeck D, Chen MH. Cancer-specific mortality after surgery or radiation for patients with clinically localized prostate cancer managed during the prostate-specific antigen era. J Clin Oncol 2003;21:2163–72.
- Berg A, Lilleby W, Bruland OS, Fossa SD. 10-year survival and quality of life in patients with high-risk pN0 prostate cancer following definitive radiotherapy. Int J Radiat Oncol Biol Phys 2007;69:1074–83.
- Stensvold A, Dahl AA, Fossa SD, Axcrona K, Lilleby W, Brennhovd B, et al. Clinicians’ use of guidelines as illustrated by curative treatment of prostate cancer at a comprehensive cancer center. Acta Oncol 2011;50:408–14.
- Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA Prostate Cancer Index: Development, reliability, and validity of a health-related quality of life measure. Med Care 1998;36:1002–12.
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77.
- Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, et al. Development of a fatigue scale. J Psychosom Res 1993;37:147–53.
- Loge JH, Ekeberg O, Kaasa S. Fatigue in the general Norwegian population: Normative data and associations. J Psychosom Res 1998;45:53–65.
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998;51:1171–8.
- Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short- Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care 1996;34: 220–33.
- Malcolm JB, Fabrizio MD, Barone BB, Given RW, Lance RS, Lynch DF, et al. Quality of life after open or robotic prostatectomy, cryoablation or brachytherapy for localized prostate cancer. J Urol 2010;183:1822–8.
- Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med 2008;358:1250–61.
- Stensvold A, Dahl AA, Brennhovd B, Cvancarova M, Fossa SD, Lilleby W, et al. Methods for prospective studies of adverse effects as applied to prostate cancer patients treated with surgery or radiotherapy without hormones. Prostate 2012;72:668–76.