Abstract
Background. Long-course preoperative chemoradiotherapy (chemo-RT) improves outcomes for rectal cancer patients, but acute side effects during treatment may cause considerable patient discomfort and may compromise treatment compliance. We developed a dose-response model for acute urinary toxicity based on a large, single-institution series.
Material and methods. In total 345 patients were treated with (chemo-)RT for primary rectal cancer from January 2007 to May 2012. Urinary toxicity during RT was scored prospectively using the CTCAE v 3.0 cystitis score (grade 0–5). Clinical variables and radiation dose to the bladder were related to graded toxicity using multivariate ordinal logistic regression. Three models were optimized, each containing all available clinical variables and one of three dose metrics: Mean dose (Dmean), equivalent uniform dose (EUD), or relative volume given x Gy or above (dose cut-off model, Vx). The optimal dose metric was chosen using the Akaike Information Criterion (AIC).
Results. Grade 1 cystitis was experienced by 138 (40%), grade 2 by 39 (11%) and grade 3 by two (1%) patients, respectively. Dose metrics were significantly correlated with toxicity in all models, but the dose cut-off model provided the best AIC value. The only significant clinical risk factors in the Vx model were male gender (p = 0.006) and brachytherapy boost (p = 0.02). Reducing the model to include gender, brachytherapy boost and Vx yielded odds ratios ORmale = 1.82 (1.17–2.80), ORbrachy = 1.36 (1.02–1.80 for each 5 Gy), x = 35.1 Gy (28.6–41.5 Gy). The predicted risk of grade 2 and above cystitis ranged from 2% to 26%.
Conclusion. Acute cystitis correlated significantly with radiation dose to the bladder; the dose-cut-off model (V35Gy) was superior to Dmean and EUD models. Male gender and brachytherapy boost increased the risk of toxicity. Wide variation in predicted risks suggests room for treatment optimization using individual dose constraints.
Patients undergoing radiotherapy (RT) for pelvic malignancies will frequently have their bladder partially or fully irradiated to substantial doses, with a resulting risk of acute and late radiation-induced urinary toxicity [Citation1,Citation2]. This risk is relatively well studied in patients treated for bladder [Citation2], prostate [Citation3] and gynecological [Citation4] cancers, but much less so in rectal cancer patients, despite long-course, preoperative (chemo-)RT being part of the standard treatment regimen for locally advanced rectal cancer [Citation5]. Urinary toxicity is, nevertheless, a genuine concern for this patient group [Citation6]. If estimates of the dose-response relationship for urinary toxicity are improved, modern RT planning techniques may allow for optimization of dose distributions to minimize the risk of toxicity [Citation7].
To carry out dose plan optimization, relevant dose constraints and the nature of volume effects in organs at risk have to be established. This has long been the focus of extensive research efforts in other cancer sites [Citation8], but limited work has been performed for preoperative RT of rectal cancer – and what little that has been done has mainly focused on gastrointestinal toxicity. This study examined the relationship between dose to the bladder and the risk of acute toxicity for a large single-institution cohort of patients receiving long-course neoadjuvant RT for locally advanced rectal cancer. Furthermore, we also investigated clinical factors that may affect this dose- response.
Material and methods
This study included patients treated at our institution from January 2007 to May 2012 with long-course (chemo-)RT for rectal cancer. Patients were excluded from the analysis if they were treated post-operatively, were treated for local recurrence of primarily operated tumors, did not have available dose or toxicity data, or received fever than 5 fractions of the planned treatment.
Acute urinary toxicity (cystitis by CTCAE v3.0) was scored prospectively by trained RT nurses during the course of the treatment, with at least weekly evaluation. Grade 1 cystitis is mainly asymptomatic; grade 2 is defined by increased frequency, dysuria, or macroscopic hematuria; and grade 3 indicates a need for IV pain medications, bladder irrigation, or transfusions. All toxicity scores were retrospectively compared with treatment charts and notes from the responsible physicians to ensure the accuracy of the scoring. The highest toxicity score registered during treatment was used for subsequent analysis.
Patient characteristics were extracted retrospectively from patient charts. Disease stage, gender, age, as well as details of chemotherapy, if given, were recorded. Details of RT treatment, including dose/fractions prescribed and delivered, were extracted from the record and verification system in the radiotherapy clinic and confirmed by chart review. Treatment technique and positioning (prone/supine) were verified by individual plan review.
Treatment planning was performed using Oncentra Masterplan (Nucletron, An Elekta Company, Netherlands). Plans consisted of either 3D conformal (3D-CRT) plans, typically using a three-field technique with combined 6 MV posterior fields and lateral 18 MV wedge fields, or intensity-modulated radiotherapy (IMRT) plans using a five- or seven-field technique with 6 MV photon beams. Dose distributions were calculated using a pencil beam convolution algorithm taking tissue heterogeneity into account. Three patients were re-planned with IMRT a few fractions into the treatment; for those patients a weighted sum of the plans were used for the study, and the patients were coded as receiving IMRT. A fraction of the patients received an external boost to the tumor only using conformal beams (see ); in that case the sum of the external treatment plans was used. Another fraction of patients received an intracavitary brachytherapy boost to the tumor, using an endorectal applicator [Citation9,Citation10]. Dose distributions for organs at risk were not available for brachytherapy, and hence brachytherapy dose was included as a separate factor in the analysis (see modeling details below). Treatment plans for patients who did not complete the full course of treatment (typically due to GI toxicity) were altered to reflect the actual dose delivered. No bladder preparation protocol was employed.
Table I. Patient and treatment characteristics.
Bladder delineation was performed by experienced radiation oncologists. The entire bladder, including both the bladder wall and the urine compartment, was delineated as one single structure. Plans, structure sets and dose distributions were imported into the Computational Environment for Radiotherapy Research (CERR) [Citation11], and dose-volume histograms (DVHs) were extracted. No correction for the effect of local fraction size was used in the primary fit; however, see details below for secondary testing for model sensitivity to fraction-size correction.
Multivariate ordinal logistic modeling was used to correlate dose and clinical- or treatment-related factors to graded toxicity scores. The risk p of toxicity of grade i or above was given by
where ORj = exp(bj) are ORs for toxicity in patients with or without clinical variable Yj, and D is a dose metric. Three DVH reduction methods, each producing a single dose metric, were used: Mean dose (Dmean), equivalent uniform dose (EUD), or relative organ volume exposed to x Gy or above (dose cut-off model, Vx). This allowed for examination of dose-volume effects for the bladder. Specifically, the EUD for a dose distribution {vi,di} was calculated as [Citation12]:
where a is a parameter describing the relative importance of high doses: EUD→Dmean for a→1 and EUD→Dmax for a→∞. The following clinical- or treatment-related variables were considered: Gender, use of chemotherapy, planning technique (IMRT vs. 3D-CRT) and positioning (prone vs. supine) were included as binary variables; age and prescribed brachytherapy boost dose as continuous variables. Three multivariate ordinal logistic models, each containing all available clinical variables and a single dose metric (Dmean, EUD or Vx) were optimized separately. For the EUD and dose cut-off models, the DVH reduction method (i.e. the value of a and x parameters) was optimized as part of the full model optimization.
Model parameters were estimated using the maximum likelihood method. The three models were compared using the Akaike Information Criterion (AIC) [Citation13]: AIC = 2*k – 2*ln(L), where k is the number of parameters in the model, ln(L) is the log-likelihood function, and inclusion of dose-volume effects, by either a dose cut-off x or the EUD parameter a, increased the number of parameters by one. The preferred model, i.e. the model which provided the optimal compromise between best fit to data and least complexity, was taken as the one resulting in the lowest AIC value. This model was subsequently refitted with only the clinical variables found to be significant (as estimated using likelihood ratio tests) in the full multivariate model. Model calibration was checked by binning patients into six equally sized risk groups, based on predicted risk of toxicity, and plotting mean predicted risk versus mean observed risk for each group. Goodness-of-fit was examined using the Fagerland-Hosmer test [Citation14], with six risk groups for each response level.
To test model sensitivity to fraction-size effects, the final model was re-fitted, limiting the fit to patients with no external boost, and converting all doses to equieffective dose in 2 Gy fractions, with α/β = 10 Gy, the EQD2αa/β = 10Gy according to the linear-quadratic model. Dependence of the dose cut-off on RT technique was examined by comparing fit quality for a range of dose cut-off values (x) for patients with IMRT and 3D-CRT treatment plans. Furthermore, optimal dose cut-offs were found for IMRT and 3D-CRT, respectively, and the predictive value for an optimal cut-off found for IMRT on 3D-CRT treatments (and visa versa) were examined graphically and by Fagerland-Hosmer test statistics.
All statistical analyses were performed in MATLAB® (2010b, The MathWorks Inc, Natick, MA, USA). Two-sided p-values of 0.05 or less were considered significant. The 95% confidence intervals (CI) for fitted parameter values were obtained from a bootstrapping procedure drawing 104 random samples with replacement from the original dataset and estimating the CI as the range from 2.5th to 97.5th percentile of the bootstrap estimates.
Results
A total of 407 patients were treated in the time period considered, out of which 345 patients were included in the analysis. See Supplementary Figure 1 (available online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2014.923933) for details of patients excluded from the study. Patient and treatment characteristics can be found in . The majority of patients were treated with one of two external beam radiotherapy schedules: Either 50.4 Gy in 28 fractions to both tumor and elective lymph nodes, or 60 Gy to the tumor and 50 Gy to the lymph nodes in 30 fractions, using a concomitant boost technique. Concomitant chemotherapy, administered to 285 patients, was primarily peroral UFT (300 mg/m2) and L-leucovorin (7.5 mg) daily on RT treatment days. The mean dose to the bladder ranged from 14 Gy to 62 Gy, with a fairly wide variation in organ dose distributions (see Supplementary Figure 2, available online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2014.923933). Urinary toxicity was generally mild; with almost half of the patients experiencing no toxicity at all, and only 12% of cases had a score of 2 or higher. Only two patients experienced grade 3 urinary toxicity, and scores were consequently binned as grade 0, grade 1, and grade 2 and above.
All tested models demonstrated a significant relationship between dose to the bladder and toxicity. contains the results for model optimization for each of the three dose-volume metrics. The dose cut-off model, with x = 35 Gy, had the lowest AIC value, and was hence selected for investigation of the effect of clinical factors. shows the relationship between V35Gy and the risk of at least grade 1 or at least grade 2 toxicity (for the sake of illustration, other risk factors have been disregarded so that the figure represents the dose-volume only model).
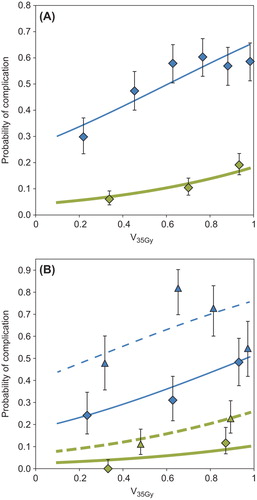
Table II. Model fit quality for different dose metrics.
provides the parameter values for the dose cut-off model fit. Only brachytherapy dose (p = 0.02, OR = 1.41 per 5 Gy) and male gender (p = 0.006, OR = 1.86) significantly increased the risk of urinary toxicity, while age (p = 0.63, OR = 0.95 per 10 years), chemotherapy (p = 0.40, OR = 0.76), treatment planning technique (p = 0.86, OR = 0.95 for IMRT) and positioning (p = 0.11, OR = 0.61) had no significant effect on the dose-response. A reduced model fit taking only V35Gy, brachytherapy dose and gender into account is provided in as well. shows the additional effects of patient- and treatment-related risk factors, by comparing the response functions for patients with highest risk (male, brachytherapy boost) and lowest risk (female, no brachytherapy boost). In contrast to the model in , patients were classified as receiving/not receiving brachytherapy, rather than considering brachytherapy dose as continuous variable, for clarity.
Table III. Ordinal logistic model fits for dose cut-off model.
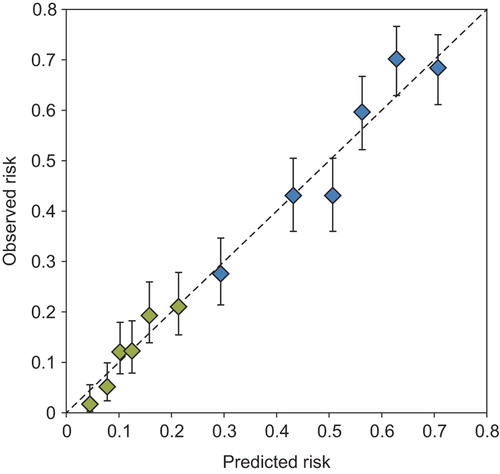
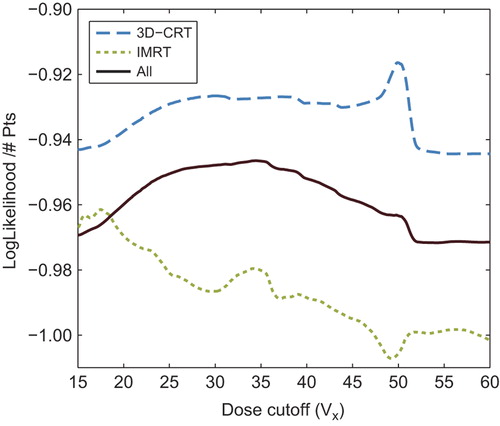
Model performance for the reduced model (V35Gy, gender and brachytherapy dose) is illustrated in , comparing predicted and observed toxicity for increasing levels of predicted risk. The p-value for goodness-of-fit was 0.71, suggesting good agreement between predicted and observed number of events. Adjusting for fraction-size effects did not improve or alter the model: Optimal dose cut-off was found to be x = 33 Gy when correcting all doses to equivalent dose in 2 Gy fractions (EQD2) with α/β = 10 Gy, which is almost exactly EQD2α/β = 10Gy for 35 Gy in 28 fractions. Dependence of the dose cut-off value on treatment technique turned out to be strong: demonstrates model fit quality of the Vx model for a range of dose levels (x), for both the full patient cohort and for 3D-CRT and IMRT treated patients separately. Model fit quality is estimated by the log likelihood divided by the number of patients in the model fit, i.e. higher values indicate better fit to the clinical data. As seen, the optimal dose cut-off found for patients treated with 3D-CRT alone is ∼50 Gy, while the optimal cut-off for IMRT patients is ∼18 Gy. and B illustrate the poor performance of a model based on an optimal cut-off found in one group for predicting toxicity for patients treated with the alternative technique. The Fagerland-Hosmer test using each model on the other group resulted in p < 0.001, indicating clear disagreement between predicted and observed toxicity. shows an apparent improvement of the generalizability of the model based on both treatment techniques (p = 0.49).
![Figure 4. Optimal dose cut-off model for acute toxicity for patients treated with A) intensity-modulated radiotherapy (IMRT, V18Gy), B) 3D conformal radiotherapy (3D-CRT, V50Gy), and C) the total patient cohort (V35Gy). Figure A) and B) additionally show the observed response for the other patient group [3D-CRT in A) and IMRT in B)]. Figure C) shows observed response for all patients (solid diamonds: 3D-CRT, empty diamonds: IMRT). Thin, blue lines and diamonds: Risk of grade 1 or above acute cystitis. Thick, green lines and diamonds: Risk of grade 2 and above acute cystitis. Uncertainty bars indicate 68% confidence levels.](/cms/asset/f565f910-a136-41db-9198-83b02e1e3bf0/ionc_a_923933_f0004_oc.jpg)
Discussion
We have presented the results of dose-response modeling for acute urinary toxicity for a large series of rectal cancer patients treated with long-course (chemo-)RT. We additionally studied dose-volume effects for acute urinary toxicity by examining various DVH reduction methods, and studied patient- and treatment-related factors influencing the dose-response estimations. A dose cut-off of ∼35 Gy yielded the closest correlation with the observed toxicity; male gender and brachytherapy boost increased the risk of side effects.
Dose-volume effects for urinary toxicity have, to the best of our knowledge, not previously been studied for rectal cancer patients. In general, studies of prostate cancer and gynecological cancer patients have struggled to establish dose-response relationships for the bladder [Citation1,Citation15], but those who have succeeded predominantly propose volumes exposed to high doses (> 75 Gy) as the main factor in the development of late toxicity [Citation16]. This may, however, be related to the type of injury (typically focal bladder injury, rather than global injury) which is observed and reported in those dose ranges. A few studies of prostate cancer patients [Citation17,Citation18] have indicated a relationship between low dose levels (V20Gy–V30Gy) and acute and late toxicity, while studies of RT for bladder cancer, where the disease itself may affect the scoring of toxicity, have shown ∼50 Gy to be the limiting dose range for large bladder volumes [Citation2]. The present study included dose distributions with volumes receiving up to 66 Gy, but no influence of those high dose levels was seen.
Clinical factors may hamper the establishment of dose-response relationships for normal tissue toxicity, such as the effects of patient- and treatment- related factors [Citation19]. We found a clear effect of male gender on the observed levels of toxicity, independently of the dose to the bladder. This is in contrast to Bruheim et al. [Citation6], who found a significantly increased level of late urinary toxicity in females after RT for rectal cancer compared to non-irradiated patients; they did not, however, correct for the actual dose delivered to the bladder. We found no interaction between gender and brachytherapy dose (data not shown), hence this is unlikely to explain the increased levels of acute toxicity observed in males in our patient cohort.
Inclusion of a brachytherapy boost in the RT regimen was also found to increase the risk of acute toxicity. Brachytherapy was included as a treatment-related variable, rather than as a contributing factor to the total dose to the bladder. Based on very preliminary experiences from magnetic resonance imaging (MRI)-based brachytherapy at our institution, a 5 Gy brachytherapy fraction will contribute on average ∼1 Gy to the Dmean and ∼2 Gy to the hottest 1 cm3 of the bladder wall. It seems unlikely that the observed OR = 1.4 for each 5 Gy brachytherapy dose can be explained purely by this contribution to the bladder dose. We therefore speculate that irradiation of other sensitive structures, such as the urethra, may play a role.
Up until recently, dose-volume constraints for organs at risk have been of little relevance for rectal cancer dose planning, since even standard 3D-CRT techniques allow for very limited optimization of dose to normal tissue. The introduction of IMRT [Citation20] and similar modern techniques offers possibilities to alter the distribution of dose in the normal tissue [Citation7]. This may prove to be of additional relevance if dose intensification [Citation21] or adaptive treatments [Citation22] are to be attempted. Our patient cohort had predicted incidences of grade 2 and above toxicity ranging from < 5% up to > 20%, which suggests that there could be room for more individual optimization of the planned dose to organs at risk. The modeling results indicate that this could be achieved by minimizing the relative V35Gy to the bladder, potentially with dose constraints stratified for clinical risk groups.
It is worth noting, however, that the current study questions the generalizability of optimization constraints for IMRT based on data from patient populations treated with more traditional techniques. This is in line with the findings of studies in head and neck cancer [Citation23] and lung cancer [Citation24]. As demonstrated in and B, dose cut-offs from 3D-CRT only are not necessarily applicable for IMRT treatments (and visa versa) in our patient cohorts. A larger variation in planning techniques and resulting dose distributions in a dataset allows for better model optimization as well as results that appear more generalizable (). [Note, however, that and B represent true independent validation sets, whereas the patient population (i.e. the data points) in is also the one used in the optimization of the depicted model.] The observed differences between models optimized for 3D-CRT and for IMRT may be due to strong correlations between high and intermediate dose levels for the 3D-CRT treatments (which complicates model optimization). Alternatively, the observations could possibly reflect differences in the interaction between dose distributions and variations in bladder filling and positioning during treatment for the two planning techniques. Thus the results may indicate that the reduction of 3D dose distributions to DVHs, which is performed in almost all studies, is in itself problematic.
In the same vein, the difficulty in establishing dose-response models for urinary toxicity [Citation1] has partly been attributed to the doses derived from the planning computed tomography (CT) scan not being representative for actual dose delivered during the treatment course due to inter- and intra-fraction bladder motion and variation in filling [Citation15]. The present study only considered dose to the bladder as estimated from the planning CT scan. While this is probably a limitation of the ability to accurately understand the dose- response, it will likely reflect the information available at the time of treatment planning in routine clinical practice for many years to come.
Acute toxicity is usually manageable and self-limiting, and the clinical relevance of dose constraints based on acute, low grade urinary toxicity might not be obvious. However, strong correlations have been observed between early and late urinary toxicity, at least in part due to consequential late effects [Citation18,Citation25,Citation26]. Thus examination of acute urinary toxicity may be valuable in providing insight into the factors affecting the organ response to radiation, such as dose-volume effects and the impact of patient- and treatment-related factors. This approach may be even more relevant for rectal cancer patients, where the intervening surgery masks observation and scoring of late complications [Citation27]. From a research perspective, attempting validation of early urinary toxicity as a surrogate marker for late bladder side effects should be considered in series of rectal cancer patients with reliable late toxicity data. Additionally, the impact of treatment-induced urinary toxicity on patient- reported quality of life needs closer study in rectal cancer patient cohorts.
In conclusion, we have demonstrated a significant dose-volume relationship for acute urinary toxicity; among the dose-volume metrics considered the best fit was provided by a V35Gy dose cut-off model. The results are based on a large patient cohort (345 patients), with a good variation in dose distributions to the bladder (including doses > 60 Gy) and with careful toxicity scoring. While the findings should be validated in a prospectively collected, independent cohort – where also the dose-response for late toxicity should be examined – the results represent the current best data for urinary toxicity dose-volume dependence for this patient group. The wide variation in predicted toxicity in our patient cohort leaves ample room for more individualized risk prediction and treatment optimization.
Supplementary material available online
Supplementary Figures 1 and 2 available online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2014.923933
ionc_a_923933_sm8214.pdf
Download PDF (297 KB)Acknowledgments
ALA is supported by CIRRO – The Lundbeck Foundation Center for Interventional Research in Radiation Oncology and The Danish Council for Strategic Research, and by the Region of Southern Denmark. IRV is supported by the Global Excellence in Health program of the Capital Region of Denmark. SMB is supported in part by grant no. P30 CA 134274-04 from the NCI. The authors are thankful for the assistance of Finn Laursen with collection of radiotherapy treatment plans.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Viswanathan AN, Yorke ED, Marks LB, Eifel PJ, Shipley WU. Radiation dose-volume effects of the urinary bladder. Int J Radiat Oncol Biol Phys 2010;76:S116–22.
- Marks LB, Carroll PR, Dugan TC, Anscher MS. The response of the urinary bladder, urethra, and ureter to radiation and chemotherapy. Int J Radiat Oncol Biol Phys 1995;31:1257–80.
- Zelefsky MJ, Levin EJ, Hunt M, Yamada Y, Shippy AM, Jackson A, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2008;70:1124–9.
- Eifel PJ, Levenback C, Wharton JT, Oswald MJ. Time course and incidence of late complications in patients treated with radiation therapy for FIGO stage IB carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys 1995;32:1289–300.
- Schmoll HJ, Van Cutsem E, Stein A, Valentini V, Glimelius B, Haustermans K, et al. ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol 2012;23:2479–516.
- Bruheim K, Guren MG, Skovlund E, Hjermstad MJ, Dahl O, Frykholm G, et al. Late side effects and quality of life after radiotherapy for rectal cancer. Int J Radiat Oncol Biol Phys 2010;76:1005–11.
- Arbea L, Ramos LI, Martínez-Monge R, Moreno M, Aristu J. Intensity-modulated radiation therapy (IMRT) vs. 3D conformal radiotherapy (3DCRT) in locally advanced rectal cancer (LARC): Dosimetric comparison and clinical implications. Radiat Oncol 2010;5:17.
- Deasy JO, Muren LP. Advancing our quantitative understanding of radiotherapy normal tissue morbidity. Acta Oncol 2014;53:577–9.
- Hansen JW, Jakobsen A. The importance of applicator design for intraluminal brachytherapy of rectal cancer. Med Phys 2006;33:3220–4.
- Jakobsen A, Ploen J, Vuong T, Appelt A, Lindebjerg J, Rafaelsen SR. Dose-effect relationship in chemoradiotherapy for locally advanced rectal cancer: A randomized trial comparing two radiation doses. Int J Radiat Oncol Biol Phys 2012;84 :949–54.
- Deasy JO, Blanco AI, Clark VH. CERR: A computational environment for radiotherapy research. Med Phys 2003; 30:979–85.
- Niemierko A. A generalized concept of equivalent uniform dose (EUD). Med Phys 1999;26:1100.
- Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr 1974;19:716–23.
- Fagerland MW, Hosmer DW. A goodness-of-fit test for the proportional odds regression model. Stat Med 2013;32: 2235–49.
- Rosewall T, Catton C, Currie G, Bayley A, Chung P, Wheat J, et al. The relationship between external beam radiotherapy dose and chronic urinary dysfunction – a methodological critique. Radiother Oncol 2010;97:40–7.
- Fiorino C, Valdagni R, Rancati T, Sanguineti G. Dose- volume effects for normal tissues in external radiotherapy: Pelvis. Radiother Oncol 2009;93:153–67.
- Karlsdóttir A, Johannessen DC, Muren LP, Wentzel-Larsen T, Dahl O. Acute morbidity related to treatment volume during 3D-conformal radiation therapy for prostate cancer. Radiother Oncol 2004;71:43–53.
- Harsolia A, Vargas C, Yan D, Brabbins D, Lockman D, Liang J, et al. Predictors for chronic urinary toxicity after the treatment of prostate cancer with adaptive three-dimensional conformal radiotherapy: Dose-volume analysis of a phase II dose-escalation study. Int J Radiat Oncol Biol Phys 2007;69:1100–9.
- Appelt AL, Vogelius IR, Farr KP, Khalil AA, Bentzen SM. Towards individualized dose constraints: Adjusting the QUANTEC radiation pneumonitis model for clinical risk factors. Acta Oncol 2014;53:605–12.
- Samuelian JM, Callister MD, Ashman JB, Young-Fadok TM, Borad MJ, Gunderson LL. Reduced acute bowel toxicity in patients treated with intensity-modulated radiotherapy for rectal cancer. Int J Radiat Oncol Biol Phys 2012;82:1981–7.
- Appelt AL, Pløen J, Vogelius IR, Bentzen SM, Jakobsen A. Radiation dose-response model for locally advanced rectal cancer after preoperative chemoradiation therapy. Int J Radiat Oncol Biol Phys 2013;85:74–80.
- Passoni P, Fiorino C, Slim N, Ronzoni M, Ricci V, Di Palo S, et al. Feasibility of an adaptive strategy in preoperative radiochemotherapy for rectal cancer with image-guided tomotherapy: Boosting the dose to the shrinking tumor. Int J Radiat Oncol Biol Phys 2013;87:67–72.
- Beetz I, Schilstra C, van Luijk P, Christianen MEMC, Doornaert P, Bijl HP, et al. External validation of three dimensional conformal radiotherapy based NTCP models for patient-rated xerostomia and sticky saliva among patients treated with intensity modulated radiotherapy. Radiother Oncol 2012;105:94–100.
- Tucker SL, Mohan R, Liengsawangwong R, Martel MK, Liao Z. Predicting pneumonitis risk: A dosimetric alternative to mean lung dose. Int J Radiat Oncol Biol Phys 2013;85:522–7.
- Dörr W, Bentzen SM. Late functional response of mouse urinary bladder to fractionated X-irradiation. Int J Radiat Biol 1999;75:1307–15.
- Dörr W, Hendry JH. Consequential late effects in normal tissues. Radiother Oncol 2001;61:223–31.
- Wallner C, Lange MM, Bonsing BA, Maas CP, Wallace CN, Dabhoiwala NF, et al. Causes of fecal and urinary incontinence after total mesorectal excision for rectal cancer based on cadaveric surgery: A study from the Cooperative Clinical Investigators of the Dutch total mesorectal excision trial. J Clin Oncol 2008;26:4466–72.

