To the Editor,
Erdheim-Chester disease (ECD) is a very rare, non-Langerhans form of histiocytosis of unknown origin, characterized by infiltration of foamy histiocytes within the bone and soft tissues, often displaying BRAF V600E mutations [Citation1]. With unknown incidence, the number of diagnosed patients has risen due to increased knowledge of the disease [Citation2]. Initial symptoms vary: bone pain, exophthalmos, diabetes insipidus and more general symptoms are seen, e.g. fever and weight loss [Citation2]. The clinical course of ECD may range from asymptomatic bone lesions to multi-systemic, life threatening disease [Citation2]. Jaw lesions have only been reported in a few patients [Citation3–7]. Treatment modalities directed to the inflammatory and immunological process include a number of regimes. Interferon-alfa (IFN-a) is the best documented treatment [Citation4]. Local radiotherapy, cladribine [Citation8], recombinant human interleukin-1 receptor inhibitor, anakinra [Citation9], and recently the BRAF inhibitor vemurafinib [Citation10], have in small patient materials also been reported. We report a case of ECD where periodontal infiltration of the jaw was seen as the first symptom. We describe our so far successful course of treatment for this subject, where the conditions now are stable.
Case history
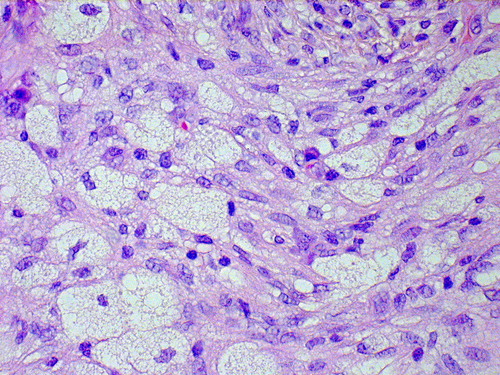
A 37-year-old male, previously healthy, was admitted to our periodontal department in 2004 due to a one-year history of progressive atypical periodontitis including severe root resorption in both jaws (). Surprisingly, gingival and bone biopsies revealed ECD with an infiltrate of foamy non-Langerhans histiocytes positive for marker CD68 (, Supplementary Figure 1, available online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2015.1023463) but negative for CD1a and S-100. Sleep disturbances due to excessive urination troubled the subject and slight bilateral exophthalmos was noted. A marrow biopsy from the iliac crest showed ECD involvement. No BRAF mutation was found. Plain radiography and bone scintigraphy of the jaw () and femur showed typical osteosclerotic lesions. Magnetic resonance imaging (MRI) of the heart was normal and MRI of abdomen did not show any infiltrations around the aorta or the aortic branches. Laboratory showed signs of inflammation with sedimentation rate (SR) of 40 mm/h, C-reactive protein (CRP) of 30 mg/l and further tests revealed diabetes insipidus and hypogonadism. Desmopressin and testosterone injections were initiated and given monthly.

Treatment with cytostatic agent cladribine (10 mg s.c. for five days each month) was initiated in 2004, but without improvement of laboratory values or histology from a new gingival biopsy. For tumor control, pegylated IFN-a 50 ug/w (Introna R) was started in February 2005, together with clodronate 50 mg × 1, in an attempt to reduce bone resorption. This treatment lasted for six years with manageable side effects, such as tiredness. No progression of disease was seen during this period, but some loose teeth were extracted (when clodronate was paused some months). CRP was at the same level as before IFN-a treatment. Computed tomography (CT) scans showed stable disease and repeated gingival biopsies showed residual lesions without signs of improvement. For further monitoring, a fluorodeoxyglucose (18F)-positron emission tomography (FDG-PET) scan was performed in 2008 showing multiple pathological isotope uptakes in the jaw, ribs, base of the skull and the long bones.
Local radiotherapy to the mandible, 1 Gy/fraction to a total dose of 10 Gy, was given to the mandible in an attempt to improve the periodontitis and to further decrease bone loss. New PET-scans after radiotherapy showed less activity, but still increased, in the irradiated area.
In January 2011 the IFN-a/bisphosphonate treatment was stopped and changed to an interleukin-1 receptor inhibitor, anakinra 100 mg s.c daily [Citation9], which immediately normalized CRP and SR. A PET scan in November 2011 showed slightly lower activity in the skeleton. The alveolar bone loss has now stopped, but gingival biopsies have revealed residual disease (, Supplementary Figure 2, available online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2015.1023463). Prosthodontics rehabilitation with dental implants is being discussed in the mandible, as the situation now is stable. Anakinra treatment is still ongoing.
Discussion
ECD may show a variety of initial symptoms and we report a case of rapidly progressive periodontitis, which has not been described earlier. The subject had a systemic disease with multiple skeletal lesions, diabetes insipidus and hypogonadism.
Evaluation of given therapies is a well known problem in ECD. It is obvious that our subject had benefit from IFN-a due to the lack of progression (besides periodontitis) during the six years of treatment. Arnaud et al. have showed the efficiency of IFN-a [Citation11]. Retrospectively, treatment with IFN-a was identified as an independent positive predictor of survival in 53 ECD patients. Mossetti et al. [Citation12] suggested, and we combined IFN-a treatment with per oral bisphosphonates as a treatment combination for ECD. The value of bisphosphonates is however questionable especially with the now known rising problems of osteonecrosis of the jaws.
Interleukin 1a inhibitor, anakinra, was more efficient and more tolerable, than IFN-a in normalizing the inflammatory laboratory values and thus giving slight radiologic improvement [Citation1]. The rationale for anakinra therapy (only few patients in the world have been treated) is based on increased expression of IL-1α in monocytes in ECD patients, overlapping mechanisms of the IFN-a action. Recently treatment with vemurafinib, a BRAF inhibitor, has shown dramatic responses in patients with advanced life threatening ECD [Citation10]. Our patient lacked BRAF V600E mutation. Even if the mutation would have been present, there was no reason to change therapy due to the absence of side effects and signs of improvement with anakinra, also with hope that the periodontal status will improve with further therapy.
Radiotherapy has been used as palliative treatment especially against pain [Citation13] but does not seem to have long standing effect. PET/CT seemed to be the most valuable monitoring modality besides measurement of the unspecific inflammatory laboratory blood samples like SR and CRP.
The oral prosthetic therapy for our and other affected ECD-subjects may be a challenge [Citation4]. Our findings correlate with Valdez et al. in that once teeth in affected areas are lost, there is marked alveolar ridge resorption with pronounced bone loss, which may affect subsequent success of prosthetic treatment [Citation14].
Conclusion
Periodontitis can be the presenting symptom in ECD and has in our subject been the main problem. Treatment with IFN-a and anakinra as well as local radiotherapy, seem to lower disease progression. Anakinra was found to be more efficient than IFN-a for our subject. The evaluation of treatment is difficult in ECD but PET/CT may be a useful technique.
Supplementary material available online
Supplementary Figure 1 and 2, available online at: http://informahealthcare.com/doi/abs/10.3109/0284186X.2015.1023463.
ionc_a_1023463_sm1449.pdf
Download PDF (1.8 MB)Acknowledgments
We thank the department of Oral Pathology at Malmö University, Professors Åke Larsson and Gunnar Warfvinge, for help with diagnosis and preparation of histological illustrations.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Diamond EL, Dagna L, Hyman DM, Cavalli G, Janku F, Estrada-Veras J, et al. Consensus guidelines for the diagnosis and clinical management of Erdheim-Chester disease. Blood 2014:124;483–92.
- Haroche J, Arnaud L, Amoura Z. Erdheim-Chester disease. Curr Opin Rheumatol 2012;24:53–9.
- Nagatsuka H, Han PP, Taguchi K, Tsujigiwa H, Gunduz M, Fukunaga J, et al. Erdheim-Chester disease in a child presenting with multiple jaw lesions. J Oral Pathol Med 2005;34:420–2.
- Petrikowski CG, McGaw WT. Erdheim-Chester disease of the jaws: literature review and case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90: 389–98.
- Valdez IH, Katz RW, Travis WD. Premature alveolar bone loss in Erdheim-Chester disease. Oral Surg Oral Med Oral Pathol 1990;70:294–6.
- Matsui K, Nagata Y, Hiraoka M. Radiotherapy for Erdheim-Chester disease. Int J Clin Oncol 2007;12:238–41.
- Brahim JS, Guckes AD, Rudy SF. Implant rehabilitation in Erdheim-Chester disease: a clinical report. J Prosthet Dent 1992;68:399–401.
- Adam Z, Koukalova R, Sprlakova A, Rehak Z, Cervinek L, Szturz P, et al.[Successful treatment of Erdheim-Chester disease by 2-chlorodeoxyadenosine-based chemotherapy. Two case studies and a literature review]. Vnitrni lekarstvi 2011;57:576–89.
- Aouba A, Georgin-Lavialle S, Pagnoux C, Martin Silva N, Renand A, Galateau-Salle F, et al. Rationale and efficacy of interleukin-1 targeting in Erdheim-Chester disease. Blood 2010;116:4070–6.
- Haroche J, Cohen-Aubart F, Emile JF, Arnaud L, Maksud P, Charlotte F, et al. Dramatic efficacy of vemurafenib in both multisystemic and refractory Erdheim-Chester disease and Langerhans cell histiocytosis harboring the BRAF V600E mutation. Blood 2013;121:1495–500.
- Arnaud L, Hervier B, Neel A, Hamidou MA, Kahn JE, Wechsler B, et al. CNS involvement and treatment with interferon-alpha are independent prognostic factors in Erdheim-Chester disease: a multicenter survival analysis of 53 patients. Blood 2011;117:2778–82.
- Mossetti G, Rendina D, Numis FG, Somma P, Postiglione L, Nunziata V. Biochemical markers of bone turnover, serum levels of interleukin-6/interleukin-6 soluble receptor and bisphosphonate treatment in Erdheim-Chester disease. Clin Exp Rheumatol 2003;21:232–6.
- Miller RC, Villa S, Kamer S, Pasquier D, Poortmans P, Micke O, et al. Palliative treatment of Erdheim-Chester disease with radiotherapy: a Rare Cancer Network study. Radiother Oncol 2006;80:323–6.
- Abrahim JS, Guckes AD, Rudy SF. Implant rehabilitation in Erdheim-Chester disease: a clinical report. J Prosthet Dent 1992;68:399–401.


