To the Editor,
Whole breast irradiation (WBI), with or without a boost dose, is considered to be the standard therapy after breast conserving surgery. However, WBI may, amongst others, induce ischemic heart disease. The incidence of ischemic heart disease appears to be proportional to the mean dose to the heart and starts within a few years after exposure [Citation1]. Furthermore, given its anatomical location, the left anterior descending (LAD) coronary artery is the cardiac artery that is most at risk for developing atherosclerosis after left-sided breast-conserving radiotherapy [Citation2]. It is, therefore, of great importance to define the most optimal radiation treatment technique for left-sided WBI. The aims are achieving the lowest dose in critical structures, the heart and the LAD, as well as administering optimal target coverage.
Using a breath-hold technique during left-sided breast cancer radiotherapy reduces the dose in the heart [Citation3]. We found that tangential beam intensity modulated radiotherapy (IMRT) in combination with a breath-hold technique, resulted in a significantly larger decrease of the dose in the heart and LAD when compared to 3D-CRT with breath-hold [Citation4]. However, others reported that TomoTherapy resulted in less dose in the critical structures when compared to tangential IMRT [Citation5,Citation6]. The question is, does this finding still hold when tangential IMRT is used with a breath-hold technique, since, currently, no breath-hold can be applied when using a TomoTherapy technique. The aim of this comparative planning study, therefore, was to determine whether with a breath-hold technique a further dose reduction to the heart and the LAD-region could be obtained with TomoTherapy when compared to tangential IMRT.
Methods
The study population consisted of 20 consecutive female breast cancer patients (pT1–2; N0–1; M0). All patients underwent breast-conserving surgery. Axillary staging was carried out by performing a sentinel node biopsy. We used the same methods as described in our former treatment planning comparison studies 3D-CRT and tangential IMRT (with and without breath-hold), and comparing tangential IMRT to proton therapy (with and without breath-hold) in the Pinnacle3 planning system (Philips Medical Systems, Cleveland, OH, US). The delineated volumes and the differences between these volumes were described in these studies as well [Citation4,Citation7].
The PTV was retracted 5 mm from the patient surface (PTVtrim) [Citation4,Citation7], in order to be able to compare the same volumes; we applied the same margins to the TomoTherapy plans. For all tangential IMRT and TomoTherapy plans, 97% of the PTVtrim had to be covered by at least 95% of the prescribed dose with a maximum of 2% receiving more than 107% of the prescribed dose [Citation8]. No compromises on the PTV coverage with either of the techniques were made to ensure a fair comparison. The prescribed dose was 42.56 Gy in 16 fractions in all cases. For both, tangential IMRT and TomoTherapy, treatment plans, based on the breath-hold as well as on the free-breathing scans, were compared in all patients. Furthermore, various dose volume parameters of PTVtrim, heart, LAD-region and lung (both lungs as well as the left lung separately) were generated and evaluated, and were the same as in the earlier study [Citation4].
Tangential IMRT-planning
With the applied tangential IMRT technique, approximately 60% of the dose was given with two tangential open fields, and 40% with four inversely planned tangential IMRT fields, using the same gantry angles, with a ‘step-and-shoot’ technique [Citation9]. The nominal energy used was 6 MV in most of the cases, and occasionally 10 MV.
For the PTVtrim the following constraints were used: uniform dose (42.56 Gy), maximum dose (45.5 Gy, point dose) and minimum dose (40.6 Gy). The maximum dose (Dmax) was defined as the maximal dose to a volume of at least 2% of that specific volume; according to ICRU 83.
For treatment optimization, the Direct Machine Parameter Optimization (DMPO) [Citation8] was used with the following criteria: the maximum number of segments was restricted to 12 (to achieve a better sparing of the critical structures; and to keep the same time slot as for conventional treatment, in order to make a breath-hold treatment feasible); the minimum segment area was set to 9 cm2. For the heart we started defining a maximum dose (point dose) of 20 Gy; after which the weights for the heart and LAD-region were set individually per patient to make a maximum sparing of these structures possible [Citation4,Citation7]. All plans were calculated with a Collapsed Cone algorithm.
TomoTherapy planning
The TomoTherapy Hi-ART treatment planning system used a different set of factors than Pinnacle to control the dose administration. For treatment, only ‘tight’ pitch factors were applied between 0.25 and 0.30. The primary collimation jaws were set to a field width of 2.45 cm at isocenter to determine the fan beam width. A modulation factor of 2.0 was used for all plans. Using TomoTherapy for breast cancer cases demands the addition of a constraint to the contralateral breast. As TomoTherapy is a rotational technique, the contralateral breast needs to be avoided. We used the same technique and dose constraints described in a planning comparison study by Reynders et al. [Citation10].
Statistics
A Wilcoxon-signed rank test was carried out to compare dose and volume differences, since the number of eligible cases was less than 30. For the convenience of comparison the values in were averaged over 20 patients. We used SPSS Statistics version 20.0 (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, USA). The level of statistical significance was defined by a p-value of ≤ 0.05 (two-sided) for all tests.
Table I. Dose distribution parameters (averaged over 20 patients).
Results
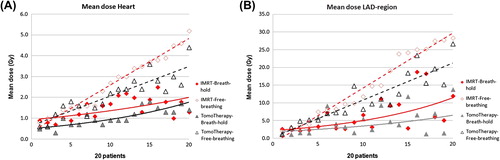
For the mean dose in the heart a significant reduction of the dose was found when using TomoTherapy instead of tangential IMRT in both breath-hold and free-breathing. The mean dose for TomoTherapy in breath-hold was reduced to 1.1 Gy compared to 1.5 Gy when using tangential IMRT. For the LAD- region TomoTherapy in breath-hold, when compared to tangential IMRT in breath-hold, resulted in a significant lower mean dose of 4.9 Gy versus 6.7 Gy, respectively ( and ).
For the dose-volume values V5Gy, V10Gy, V30Gy no significant differences were noted between the two techniques for the heart and LAD-region, when using breath-hold. However, when using TomoTherapy, the V20Gy for the heart was significantly lower compared to tangential IMRT. With breath-hold, compared to free-breathing, in both tangential IMRT and TomoTherapy, a significant lower dose could be achieved in all dose-volume values for the heart and LAD-region ().
The mean doses in the contralateral lung and the mean doses in both lungs were comparable for both techniques in breath-hold; a mean dose of 5.2 Gy and 5.4 Gy was found for the left lung for TomoTherapy and tangential IMRT, respectively. For PTVtrim comparable dose values were found for both techniques as well; however, for the V107% significant lower doses were found when using TomoTherapy in breath-hold ().
Discussion
The results show that, with TomoTherapy, in breath-hold, the mean doses to the heart as well as to the LAD-region could be reduced significantly when compared to tangential IMRT in breath-hold. This was achieved without compromising the doses to the target volumes. For the other dose values both techniques in breath-hold were comparable. The difference between the mean heart doses when using a tangential IMRT technique in breath-hold compared to TomoTherapy in breath-hold, was limited to 1.5 Gy (SD 0.5 Gy) and 1.1 Gy (SD 0.4 Gy), respectively. However, it should be emphasized that the combination of a breath-hold technique with TomoTherapy cannot be performed in daily clinical practice, due to the longer beam-on time (a TomoTherapy treatment session in free-breathing fraction lasts about 20 minutes) and to the rotating technique [Citation10]. Therefore, currently, TomoTherapy can only be applied without breath-hold. With respect to TomoTherapy in free-breathing: we showed, that less dose to the heart and LAD- region can be achieved when tangential IMRT in breath-hold is applied ().
Theoretically, the tangential IMRT technique could even still be optimized. A higher dose reduction to the heart could be achieved by using a multiple field IMRT technique, although Borges et al., reported that this could only be achieved at the expense of a higher dose in organs at risk (OARs) and normal tissue [Citation11].
We did not evaluate the dose in the contralateral breast as this item was analyzed in other studies. Shiau et al. found no significant difference in mean doses in the contralateral breast between Tomo Therapy and tangential IMRT. However, as the low dose (V5Gy) in the contralateral breast was higher for TomoTherapy compared to tangential IMRT, this should be taken into account when using a TomoTherapy technique [Citation6]. Recently, TomoDirect was introduced, allowing the administration of radiation using fixed gantry angles. As Qi et al. described in their study, the TomoDirect technique leads to less dose in the contralateral breast compared to helical TomoTherapy, as used in this study [Citation12]. Finally, we underline the statement of Qi et al., that individualized radiation treatment is of importance and that the appropriate radiation technique needs to be selected according to the patient's risk factors [Citation12].
Conclusion
In daily clinical practice tangential IMRT in breath-hold is the preferred technique to maximally reduce the dose to heart and LAD-region in left-sided WBI since a combination of TomoTherapy and breath-hold is not feasible yet.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Darby SC, Ewertz M, McGale P, Bennet AM, Blom- Goldman U, Bronnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 2013;368:987–98.
- Nilsson G, Holmberg L, Garmo H, Duvernoy O, Sjögren I, Lagerqvist B, et al. Distribution of coronary artery stenosis after radiation for breast cancer. J Clin Oncol 2012; 30:380–6.
- Swanson T, Grills IS, Ye H, Entwistle A, Teahan M, Letts N, et al. Six-year experience routinely using moderate deep inspiration breath-hold for the reduction of cardiac dose in left-sided breast irradiation for patients with early-stage or locally advanced breast cancer. Am J Clin Oncol 2013; 36:24–30.
- Mast ME, van Kempen-Harteveld L, Heijenbrok MW, Kalidien Y, Rozema H, Jansen WP, et al. Left-sided breast cancer radiotherapy with and without breath-hold: Does IMRT reduce the cardiac dose even further? Radiother Oncol 2013;108:248–53.
- Coon AB, Dickler A, Kirk MC, Liao Y, Shah AP, Strauss JB, et al. TomoTherapy and multifield intensity-modulated radiotherapy planning reduce cardiac doses in left-sided breast cancer patients with unfavorable cardiac anatomy. Int J Radiat Oncol Biol Phys 2010; 78:104–10.
- Shiau A, Hsieh C, Tien H, Yeh HP, Lin CT, Shueng PW, et al. Left-sided whole breast irradiation with hybrid-IMRT and helical tomotherapy dosimetric comparison. Biomed Res Int 2014:741326.
- Mast ME, Vredeveld EJ, Credoe H, van Egmond J, Heijenbrok MW, Hug EB, et al. Whole breast proton irradiation for maximal reduction of heart dose in breast cancer patients. Breast Cancer Res Treat 2014;148:33–9.
- Borst GR, Sonke JJ, den Hollander S, Betgen A, Remeijer P, van Giersbergen A, et al. Clinical results of image-guided deep inspiration breath-hold breast irradiation. Int J Radiat Oncol Biol Phys 2010;78:1345–51.
- van Asselen B, Schwarz M, van Vliet-Vroegindeweij C, Lebesque JV, Mijnheer BJ, Damen EM. Intensity-modulated radiotherapy of breast cancer using direct aperture optimization. Radiother Oncol 2006;79:162–9.
- Reynders T, Tournel K, De Coninck P, Heymann S, Vinh-Hung V, Van Parijs H, et al. Dosimetric assessment of static and helical TomoTherapy in the clinical implementation of breast cancer treatments. Radiother Oncol 2009; 93:71–9.
- Borges C, Cunha G, Monteiro-Grillo I, Vaz P, Teixeira N. Comparison of different breast planning techniques and algorithms for radiation therapy treatment. Phys Med 2014; 30:160–70.
- Qi XS, Liu TX, Liu AK, Newman F, Rabinovitch R, Kavanaqh B, et al. Left-sided breast cancer irradiation using rotational and fixed- field radiotherapy. Med Dosim 2014;39:227–34.

