Abstract
Background: Image-guided percutaneous ablation methods have proved effective for treatment of benign bone tumors and for palliation of metastases involving the bone. However, the role of these techniques is controversial and has to be better defined in the setting of palliative care.
Methods: A systematic review of the existing data regarding minimally invasive techniques for the pain management of vertebral bone metastases was performed by experts of the European Palliative Care Research Network.
Results: Only five papers were taken into consideration after performing rigorous screening according to inclusion and exclusion criteria (low number of patients, retrospective series, proceedings).
Discussion: According to the present data a recommendation should be made to perform kiphoplasty in patients with vertebral tumors or metastases. However, the strength of this recommendation was based on one randomized controlled study. Several weaknesses and low quality of study design were observed with other techniques.
Conclusion: Further randomized controlled trials are required to improve the strength of evidence available to suggest these procedures on large scale. Until then, the balance of evidence favors the use of these procedures in a small select cohort of patients with severe and disabling back pain refractory to medical therapy.
Metastatic tumors are the most common malignancy of bone, with 10–30% of all cancer patients being affected by bone metastases, with prostate, breast, and lung cancer accounting for the larger number of vertebral metastases. The spine can also be affected by primary tumors, e.g. myeloma. Overall vertebral metastatidc lesions are the most common cause of cancer pain [Citation1]. The progression of untreated lesions results in painful microfractures, risk of vertebral body collapse and spinal cord compression, and are associated with significant pain, disability, and morbidity. In particular, incident bone pain is difficult to manage; it occurs on movement with an higher intensity than background pain, interferes with physical activity and limits patients’ quality of life [Citation2]. Traditional treatments involve a combination of pharmacotherapy, radiotherapy, and surgical procedures [Citation3]. The intensity of incident pain may be reduced by increasing the opioid dose above that one effective for controlling pain at rest. However, this approach could result in the development of adverse effects, and a therapeutic balance between background-breakthrough pain intensity and opioid dosing is necessary, providing breakthrough medication as needed or giving analgesics preemptively [Citation2]. Orthopedic surgery is often inappropriate in these patients, considering the trade off between benefits and risks. In fact, depending on the tumor diagnosis and staging, the average life expectancy in patients with vertebral metastasis can be no longer than one year.
Image-guided percutaneous ablation methods have proved effective for treatment of benign bone tumors and for palliation of metastases involving the bone [Citation4]. Minimally invasive techniques have being increasingly used as options for the management of vertebral metastases. Different techniques have been developed in an attempt to achieve analgesia and to limit procedure-related complications. Percutaneous vertebroplasty (PV) and later kyphoplasty (KP), cryoablation (CA) and radiofrequency, have gained worldwide application as effective minimally invasive treatments for back pain due to osteoporotic and malignant vertebral collapses refractory to conservative treatment [Citation5].
However, the role of these techniques is controversial and has to be better defined in the setting of palliative care. Therefore, we performed a systematic review of the existing data regarding minimally invasive techniques for the pain management of vertebral bone metastases. This work was done within the European Palliative Care Research Network (EPCRN) as part of the project to update the European Association for Palliative Care (EAPC) recommendations for the management of cancer pain. The scope of this initiative for the EAPC is through rigorous and sound methodology to review the evidence of pain strategies in order to provide guidelines for the treatment of cancer pain [Citation6]. The present systematic review was based on the following research question: “in adult patients with vertebral pain due to cancer, what is the evidence to support the performance of percutaneous procedures”?
Methods
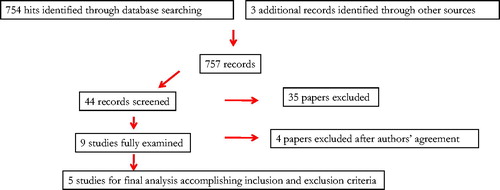
A systematic literature search on MedLine, Embase and Cochrane Central Register of Controlled Trials electronic databases was carried out from each database set-up date to 3 February 2015. Hand search of the references list of identified papers was also performed ().
Table I. Search strategy for vertebral percutaneous procedures.
Studies were included if the interventional techniques were compared with analgesic drugs, or sham procedure, if they were conducted in adult patients with cancer pain, if they contained outcomes on pain, and were written in English language. All data from the eligible trials were analyzed using the GRADE system, to define the quality of the evidence and to determine the strength of the recommendations for clinical practice.
Given the expected paucity of comparative studies, non-comparative observational studies with a minimum set of 50 patients were also considered. Retrospective data or data from mixed cancer and non-cancer population, as well as proceeding abstracts were excluded. Studies were excluded in case of double publications, if related to other clinical indications, or if they were reporting only complications. Interventions were grouped according to the type of procedure.
Titles and abstracts of retrieved citations were reviewed independently by two researchers and potentially relevant papers read in full text. Each abstract was checked at least twice by two of the co-authors and selected according to the inclusion and exclusion criteria. Abstracts that matched the inclusion criteria and those with no clear information to be considered for exclusion were selected for full reading. Inclusion and exclusion criteria were reapplied and all articles that fitted with this review were analyzed. The co-authors discussed and resolved eventual doubts and disagreements regarding the studies of interest. The identified publications were grouped according to the different available techniques.
The studies were graded according to quality scoring system that ranges from +4 or A to +1 or D, where +4 or A=high quality (further evidence is unlikely to change confidence in the estimate of effect), +3 or B=moderate (further research is likely to have an important impact on confidence in the estimate of effect and may change the estimate), +2 or C=low (further research is very likely to have an important impact on confidence in the estimate of effect and may change the estimate), and +1 or D=very low (any estimate of effect is very uncertain) [Citation7]. Randomized controlled studies received an initial score of +4. Points were subtracted or added depending on the quality, consistency, directness, imprecise or sparse data [Citation7,Citation8]. The strength of recommendations were elaborated based on the examined quality of evidence and classified in “strong for using the intervention”, “weak for using the intervention”, “weak against using the intervention”, and “strong against using the intervention”.
Results
The initial search yielded 754 records of which 44 abstracts were found to be of interest. Twenty-five additional records were retrieved by hand search or cross-references. Only nine papers were fully examined after the initial screening according to inclusion and exclusion criteria (low number of patients, retrospective series, proceedings) ().
Radiofrequency ablation (RFA)
No studies with a sufficient number of patients, reporting pain outcomes were found. In total 15 patients prospectively assessed after RFA and surgical stabilization were compared with a historical series of 15 patients treated by radiotherapy and surgical stabilization. RFA resulted more effective than radiotherapy and surgical stabilization [Citation9]. Given the retrospective comparison and the mixed treatment which make difficult to evaluate the outcome, it was decided to withdraw the study from analysis. In another study 52 patients with bone and soft-tissue sarcomas were prospectively assessed after RFA, but no pain outcomes were reported [Citation10].
Kiphoplasty
Two series of 55 and 65 KPs have been reported in patients with vertebral metastases, and with osteolytic fractures associated with myeloma [Citation11,Citation12]. KP was efficacious in the treatment of osteolytic vertebral compression fractures resulting from multiple myeloma [Citation11]. However, in this study the 55 procedures were performed at different levels in 18 patients. Therefore, the study was not considered, according to inclusion criteria of a minimum of 50 patients. One randomized controlled study of 134 patients with vertebral body fractures in patients with cancer was performed. Most untreated patients crossed over to KP after one-month assessment [Citation13]. This study achieved a positive GRADE (+1).
Vertebroplasty
Several observational studies of VP performed in mixed population were retrieved, but only three of them assessed vertebral tumors or metastases. A total of 128 patients with spinal metastases and myeloma were prospectively assessed [Citation14], In another series 52 patients with spinal metastases underwent 59 VP procedures [Citation15]. Finally, 52 patients with myeloma were treated with VP [Citation16].
Cryoablation
In a prospective open-label study, 61 patients received percutaneous image-guided CA [Citation17]. However, the sites were various and vertebral metastases were poorly represented.
Thus, after a further screening selectively fitting inclusion criteria, only five studies were selected for the final analysis, because being comparative or prospective series of a minimum of 50 patients, with vertebral localization, and reporting pain outcomes. The principal findings of these studies are reported in .
Table II. Studies selected.
Discussion
In the last decades, a large number of cancer and non-cancer patients have been treated successfully with percutaneous techniques. A previous cumulative analysis demonstrated a significant reduction in pain after VP of KP in vertebral cancer pain [Citation18]. However, existing data are often limited to series with a low number of patients, retrospective designs, mixed population, or published in congress proceedings. While there are several trials assessing the efficacy of vertebral percutaneous procedures suggesting that these procedures may have a role, the number of the series and quality of data remain quite low, and most of these studies did not provide evident proofs of efficacy in cancer patients with vertebral bone tumors or vertebral metastases. Potential flaws confounding the outcomes include low accrual rate, inclusion of patients with different types of fractures, not-uniform evaluation of fractures, and other pain generators unrelated to the fracture, very problematic eventual sham design, no reported clinical examination to determine the source of pain [Citation19].
Series of cancer patients with vertebral pain have been treated by KP, reporting significant and lasting analgesic effects [Citation12]. Data should be considered with caution, as no data on analgesic consumption were provided. Of concern, cement leakage were reported in 4–12% [Citation11,Citation12], and vertebral fractures in 8% of patients [Citation12]. In the only existing study with a randomized controlled design [Citation13], significant improvement of disability, back pain, and quality of life were reported in patients who underwent the procedure in comparison with untreated patients. Of interest, no specific information on the pharmacological management of pain was given. This study also suffered of important limitations, already reported in studies of non-cancer patients who underwent KP, as investigators and patients were not masked to treatment allocation [Citation20].
Similar observations could be considered for VP. Three observational studies suggested that the procedure was effective in relieving pain and improving disability in cancer patients, although no data on analgesic use were given [Citation14–16]. No controlled study exists. In non-cancer patients two double-blind, randomized, placebo controlled trials of VP have shown that differences in pain relief were neither statistically significant nor clinically meaningful, suggesting that this procedure was no better than a sham intervention, without injection of cement, in relieving pain for patients with vertebral fractures [Citation21–23]. This was in contrast with data from open randomized controlled trials in which VP was compared with conservative medical therapy [Citation24,Citation25]. Individual patient data meta-analysis from two blinded trials of VP failed to show an advantage of VP over placebo [Citation26]. It has been speculated that there were different expectations among patients and investigators in the sham-controlled trials versus the open trial. [Citation27]. In cancer patients only observational studies have reported data with VP. While reporting favorable analgesic effects, often data regarding the use of analgesics were lacking. Of interest, complications were of concern [Citation15,Citation16]. Cement leakage has been reported to occurring in 20–70% of patients receiving VP [Citation14,Citation21,Citation22,Citation28]. Cement embolism was detected in 26% of VP recipients [Citation29]. KP has been reported to be at a lower risk of cement extravasation [Citation20]. Although these complications have rarely been found to be of clinical consequences, dramatic events requiring urgent interventions may occur. A substantial increased risk of subsequent vertebral fracture after VP or KP has been reported compared with patients not receiving either of these procedures [Citation30]. Thus, these procedures carry risk of substantial harm [Citation29].
Equivalence of pain relief between VT and KP have been reported in studies of non-cancer patients. Of interest, it seems that subacute and chronic fractures, which more easily are encountered in palliative care patients, do not respond to vertebral augmentation techniques as dramatically as acute fractures [Citation31]. The relationship of VP, radiotherapy, and surgery is unclear. While complementary, they have different consequences and the therapeutic sequence has never been established [Citation20]. For RF and CA there are no meaningful data available yet. Thus, any judgment should be postponed until new quantitative and qualitative data are generated.
From a palliative care perspective, incident bone pain, a subtype of predictable breakthrough pain has regrettably never been explored in this context. This kind of pain is induced by movement and represents a challenging condition for physicians, as it seriously compromises patients’ quality of life and conditions the use of opioids. In most of these studies, analgesic consumption was rarely or badly reported. Thus, from a clinical point of view it is difficult to estimate the weight of the procedure while not considering the analgesic treatment before and after the procedure. The significant heterogeneity of existing studies suggests that the current literature is delivering inconsistent messages and further trials are needed to delineate confounding variables.
Conclusion
According to the present data a recommendation should be made to perform KP in patients with vertebral tumors or metastases. However, the strength of this recommendation, based on one randomized controlled study, is conditioned by several weaknesses and low quality of study design. For the other techniques recommendations are “weak for using the intervention” for RFA or “weak against using the intervention” for VP and CA. Further randomized controlled trials of VP and KP in cancer patients are required to improve the strength of evidence available to suggest these procedures on large scale. Until then, the balance of evidence favors the use of these procedures in a small select cohort of patients with severe and disabling back pain refractory to medical therapy. Studies should assess how these techniques can specifically improve incident bone pain, which is one of the most important negative predictors of pain outcome [Citation32].
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Caraceni A, Portenoy RK. An international survey of cancer pain characteristics and syndromes. IASP Task Force on Cancer Pain. International Association for the Study of Pain. Pain 1999;82:263–74.
- Mercadante S, Villari P, Ferrera P, Casuccio A. Optimization of opioid therapy for preventing incident pain associated with bone metastases. J Pain Symptom Manage 2004;28:505–10.
- Kassamali RH, Ganeshan A, Hoey ET, Crowe PM, Douis H, Henderson J. Pain management in spinal metastases: The role of percutaneous vertebral augmentation. Ann Oncol 2011;22:782–6.
- Rosenthal D, Callstrom MR. Critical review and state of the art in interventional oncology: Benign and metastatic disease involving bone. Radiology 2012;262:765–80.
- Papanastrassiou ID, Filis AK, Gerochristou MA, Vrionis FD. Controversial issues in kyphoplasty and vertebroplasty in malignant vertebral fractures. Cancer Control 2014;21:151–7.
- Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, Cherny N, et al. Use of opioid analgesics in the treatment of cancer pain: Evidence-based recommendations from the EAPC. European Palliative Care Research Collaborative (EPCRC); European Association for Palliative Care (EAPC). Lancet Oncol 2012;13:e58–68.
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. GRADE Working Group. Grading quality of evidence and strength of recommendations. Br Med J 2004;328:1490.
- GRADE Working Group. Clinical evidence. London: BMJ Publishing Group; 2014. Available from: http://clinicalevidence.bmj.com/x/set/static/ebm/learn/665072.html [cited 2015 Feb 20].
- Di Francesco A, Flamini S, Zugaro L, Zoccali C. Preoperative radiofrequency ablation in painful osteolytic long bone metastases. Acta Orthopaedica Belgica 2012;78:523–30.
- Yamakado K, Matsumine A, Nakamura T, Nakatsuka A, Takaki H, Matsubara T, et al. Radiofrequency ablation for the treatment of recurrent bone and soft-tissue sarcomas in non-surgical candidates. Int J Clin Oncol 2013;19:955–62.
- Dudeney S, Lieberman IH, Reinhardt MK, Hussein M. Kiphoplasty in the treatment of osteolytic vertebral compression fractures as a result of multiple myeloma. J Clin Oncol 2002;20:2382–7.
- Pflugmacher R, Taylor R, Agarwal A, Melcher I, Disch A, Haas NP, et al. Balloon kyphoplasty in the treatment of metastatic disease of the spine: A 2 year prospective evaluation. Eur J Spine 2008;17:1042–8.
- Barenson J, Pfugmacher R, Jarzem P, Zander P, Schechtman K, Tillmann JB, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: A multicentre, randomized controlled trial. Lancet Oncol 2011;12:225–35.
- Chew C, Ritchie M, O’Dwyer PJ, Edwards R. A prospective study of percutaneous vertebroplasty in patients with myeloma and spinal metastases. Clin Radiol 2001;66:1193–6.
- Calmes V, Vallée JN, Rose M, Chiras J. Osteoblastic and mixed spinal metastases: Evaluation of the analgesic efficacy of percutaneous vertebroplasty. Am J Neuroradiol 2007;28:570–4.
- Anselmetti GC, Manca A, Montemurro F, Hirsch J, Chiara G, Grignani G, et al. Percutaneous vertebroplasty in multiple myeloma: Prospective long-term follow-up in 106 consecutive patients. Cardiovasc Intervent Radiol 2012;35:139–45.
- Callstrom MR, Dupuy DE, Solomon SB, Beres RA, Littrup PJ, Davis KW, et al. Percutaneous image-guided cryoablation of painful metastases involving bone. Cancer 2013;119:1033–41.
- McGirt MJ, Parker SL, Wolinsky JP, Witham TF, Bydon A, Gokaslan ZL. Vertebroplasty and kiphoplasty for the treatment of vertebral compression fractures: An evidenced-based review of the literature. Spine J 2009;9:501–8.
- Papanastassiou ID, Philips FM, van Meirhaeghe J, Berenson JR, Andersson BJ, Chung G, et al. Comparing effects of kiphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur J Spine 2012;21:1826–43.
- Papanastassious ID, Filis AK, Gerochristou MA, Vrionis FD. Controversial issues in kyphoplasty and vertebroplasty in malignant vertebral fractures. Cancer Control 2014;21:151–7.
- Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009;361:557–68.
- Buchbinder R, Osborne RH, Kallmes D. Vertebroplasty appears no better than placebo for painful osteoporotic spinal fractures, and has potential to cause harm. Med J Aust 2009;191:476–7.
- Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009;361:569–79.
- Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): An open-label randomized trial. Lancet 2010;376:1085–92.
- Voormolen M, Mali W, Lohle, Fransen H, Lampmann L, van der Graaf Y, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: Short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. Am J Neuroradol 2007;28:555–60.
- Staples MP, Kallmes DF, Comstock BA, Jarvik JG, Osborne RH, Heagerty PJ. Effectiveness of vertebroplasty using individual patient data from two randomized placebo controlled trials: Meta-analysis. Br Med J 2011;343:d3952.
- Hróbjartsson A, Thomsen AS, Emanuelsson F, Tendal B, Hilden J, Boutron I, et al. Observer bias in randomized clinical trials with measurement scale outcomes: A systematic review of trials with both blinded and nonblinded assessors. Can Med Assoc J 2013;185:E201–11.
- Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: A meat-analysis of the literature. Spine J 2008;8:488–97.
- Miller FM, Kallmes DF, Buchbinder R. Vertebroplasty and the placebo response. Radiology 2011;259:621–5.
- Mudano AS, Bian J, Cope JU, Curtis JR, Gross TP, Allison JJ, et al. Vertebroplasty and kyphoplasty are associated with an increased risk of secondary vertebral compression fractures. A population-based cohort study. Osteoporos Int 2009;20:819–26.
- Albers SL, Latchaw RE. The effects of randomized controlled trials on vertebroplasty and kyphoplasty: A square peg in a round hole. Pain Phys 2013;16:E331–48.
- Knudsen AK, Brunelli C, Klepstad P, Aass N, Apolone G, Corli O, et al. Which domains should be included in a cancer pain classification system? Analyses of longitudinal data. Pain 2012;153:696–703.