Abstract
Objective. The objective of this study was to evaluate the effect of an intervention with advance provision of emergency contraceptive pills (ECP), condoms, and extended information to a targeted group of teenage girls, compared with a control group, 12 months after intervention.
Material and methods. A randomized controlled trial among 420 girls, 15–19 years old, requesting emergency contraception at a youth clinic in Sweden was carried out. Data were collected by a questionnaire at the initial visit and structured telephone interviews 12 months after enrolment. Differences between the intervention group and the control group regarding ECP use, time interval from unprotected intercourse to ECP intake, contraceptive use, and sexual risk-taking were analysed.
Results. One year after the intervention 62% of the girls could be reached for follow-up. The girls in the intervention group reported a shorter time interval (mean 15.3 hours) from unprotected intercourse to ECP intake compared to the control group (mean 25.8 hours) (p = 0.019), without any evidence of decreased use of contraceptives or increased sexual risk-taking.
Conclusion. Even up to 12 months following the intervention, advance provision of ECP at one single occasion, to a specific target group of adolescent girls, shortens the time interval from unprotected intercourse to pill intake, without jeopardizing contraceptive use or increasing sexual risk-taking. Considering the clinical relevance of these results, we suggest that advance provision of ECP could be implemented as a routine preventive measure for this target group.
Introduction
A single-dose administration of levonorgestrel 1.5 mg is the most widely used emergency contraceptive pill (ECP) worldwide. Despite few side effects and increased sale statistics, the method has not yet met the expectations regarding reduced abortion rates, especially among teenagers, that many had hoped for (Citation1). ECP is recommended to be taken as soon as possible after unprotected intercourse; however, obstacles for prompt use are many, including: underestimation of pregnancy risk, limited knowledge, worries about side effects, high cost, cultural barriers, and restricted availability. Different strategies and interventions such as information campaigns, over-the-counter sales, subsidies, and advance provision have, therefore, been adopted in order to increase availability and thereby decrease the underutilization (Citation2,3).
Theoretically, advance provision of ECP is a cost-effective method that has the potential to prevent unintended pregnancies (Citation4). Most international studies are concordant; women provided with an advance provision of ECP use them to a greater extent and more rapidly after unprotected intercourse without engaging in increased sexual risk-taking behaviour (Citation5,6).
Since most studies evaluating advance provision of emergency contraception have only conducted a 6-month follow-up post intervention, the aim of this study was to evaluate an intervention of advance provision of ECP to teenage girls, 12 months after enrolment. Main outcome measures were time frames for ECP use, contraceptive use, and sexual risk-taking.
Material and methods
We conducted a randomized controlled trial among teenage girls requesting ECP at a local youth clinic in a medium-sized university town in Sweden. The hypothesis was that advance provision of ECP, condoms, and extended information would reduce the time interval for ECP use and improve contraceptive use among participants in the intervention group. A power calculation based on a previous study by Gold et al. (Citation3) estimated that 150 women in an intervention group (IG) and 150 in a control group (CG) would be needed to detect a difference between the groups of 11 hours' interval before use of ECP after unprotected sex with 80% power, at 5% significance level. We assumed a 30% drop-out rate, which made us include 210 women in each group.
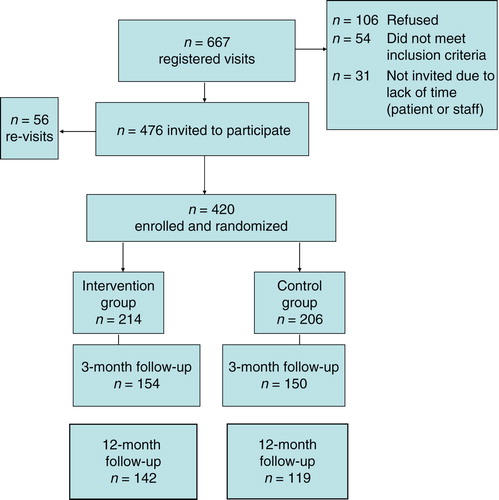
In total 667 girls between 15–19 years who visited the youth clinic in order to get ECP were consecutively invited to participate, and 420 out of those who met the inclusion criteria and accepted participation were randomly assigned to either IG or to CG. Participation rates are shown in .
Girls who met the inclusion criteria and accepted participation received verbal and written information about the study. Participants provided contact information and signed an informed consent. The randomization procedure was organized in blocks of four. Pre-coded envelopes were sequentially labelled with a study identification number that had been generated by a table of random digits and handed out consecutively to the participants, allocating them into IG or CG. The envelopes contained a baseline questionnaire, which the participants completed in a private area at the clinic, before receiving the requested ECP. The CG received standard care, including ECP (1.5 mg levonorgestrel in a single dose). Additionally to the standard care, participants in the IG were provided with an intervention kit containing one extra package of ECP, ten condoms, and a specially designed leaflet with information of protection against unwanted pregnancy and sexually transmitted infections (STI). The girls were followed up after 3, 6, and 12 months by a structured telephone interview with 12 questions regarding contraceptive use and sexual risk-taking behaviour. Data from the 3- and 6-month follow-up have been published previously (Citation7). The study was approved by the local Medical Research Committee in Uppsala.
The baseline questionnaire, before the intervention, consisted of 29 questions covering the following areas: demographic data, reproductive and sexual health history, contraceptive use, and sexual risk-taking behaviour.
There were no differences between the groups concerning socio-demographic background at baseline, or at follow up 1 year later. At the 12-month follow-up, the mean age was 18 years in both groups, 95.1% in the IG and 94.1% in the CG were of Nordic origin, 20.4% in the IG and 21.0% in the CG had immigrant parents, 88.6% in the IG and 83.9% in the CG were students, and 20.4% in the IG and 18.5% in the CG were daily smokers. Their previous sexual experiences were also similar; first intercourse was reported at a mean age of 15.2 years in the IG and 15.4 in the CG, condom use at first intercourse was reported by 76.1% in the IG and 65.5% in the CG, the mean number of sexual partners was 4.3 in the IG and 4.6 in the CG, 8.5% in the IG and 6.9% in the CG had a history of STI, 6.3% in the IG and 7.6% in the CG had experienced an abortion, and 48.6% in the IG and 49.6% in the CG had used ECP before inclusion into the trial. Girls who were lost after 1 year differed from those who completed the study only with respect to their own and their parents' origin. Furthermore, girls who completed the study were more likely to have a Nordic origin, 94.6% compared with 88.1% (p = 0.02) of those lost to follow-up. Of the girls who completed the study 20.7% had parents with an immigrant background compared with 34.0% (p = 0.01) of the girls who dropped out. There were no differences in sexual experiences between those who completed the study and those who were lost to follow-up.
Data analysis
The Statistical Package for Social Sciences (SPSS) for Windows (14.0) was used when entering and analysing data. Differences between groups were tested using Student's t test, Fischer's exact test, and Pearson's chi-square test for two independent samples. Differences were considered significant if p < 0.05.
Results
During the study period 667 adolescent girls requested ECP at the selected youth clinic. A total of 54 girls did not meet the inclusion criteria (50 were not within the age span, 2 did not speak Swedish, and 2 were excluded for other unspecified reasons); 31 were not invited due to staff's lack of time. Of the remaining girls, 106 refused to participate, and 56 were revisits who had already been invited. After 12 months 72 girls in the intervention group and 87 girls in the control group were lost to follow-up, leaving a 62% follow-up rate (n = 142 versus n = 119) ().
The main outcome measure, the time interval for intake of ECP after an unprotected intercourse at the follow-up after 12 months, was markedly reduced in the IG when compared with that in the CG ().
Table I. Time interval in hours (mean, SD) from unprotected intercourse to ECP intake in the Intervention group versus the Control group.
Almost half, 45% (n = 64) of the girls in the IG had not used their extra ECP package, 40% (n = 57) had used it, 8% (n = 11) had given it to a friend, and 7% (n = 10) did not remember or were unsure if they had used it.
After 12 months, there were no differences in contraceptive use and sexual risk-taking between the two groups. In total 83.1% in the IG and 89.1% in the CG had used oral contraception and/or condom at their latest intercourse, but 18.3% in the IG and 23.7% in the CG had at some time during the last 3 months been engaged in unprotected sex ().
Table II. Contraceptive use and sexual risk-taking at 12-month follow-up in the Intervention group versus the Control group.
Discussion
By directing the intervention to a special group, at high risk for unintended pregnancies, our aim was to evaluate if this one-dose advance supply of ECP would make any difference in time frames for ECP intake, contraceptive use, and sexual risk-taking behaviour. Our study sample did not have the power to show any differences in pregnancy or abortion rates between groups; however, this was not the aim of the study.
The most important finding was that even with this limited intervention, a difference between the groups in the time interval from unprotected intercourse to ECP intake was still notable after 1 year. Concerns about increased sexual risk-taking in the IG were not confirmed, which is congruent with our previous results from the 3-month and the 6-month follow-up. However, there was still considerable risk-taking among all girls regardless of group allocation, indicating that girls requesting ECP are well-suited candidates for advance provision of ECP.
Some girls had not used the extra dose themselves, but had given it to a friend, which was a positive finding, since it could have helped another girl to prevent an unwanted pregnancy. Advance provision of ECP as a routine preventive measure could therefore be beneficial for this target group, especially since youth clinics in Sweden, where ECP is distributed to young people free of charge, are only open during week days and the need for ECP may arise at all times of the week.
The benefits of increased availability was also discussed by Polis et al. (Citation5), who concluded that women should have easy access to emergency contraception because it can decrease unwanted pregnancies. How this could be best implemented remains to be demonstrated. In a widespread community-based study by Glasier et al. (Citation8) five courses of ECP were distributed to 17,800 women aged 16–29 years. Despite the large sample size and the generous intervention, no effect on the abortion rates could be demonstrated; consequently, the authors raised the question whether they targeted the right women.
It is most likely not cost-effective to provide ECP in advance to every woman. Instead, choosing certain groups at high risk for unintended pregnancies could be a better strategy. The potential clinical feasibility of this patient-oriented trial was therefore considered important. In order to enhance a clinical implementation the advance ECP supply was limited to one dose only together with condoms and some extra information. We did several follow-ups in order to evaluate both short- and long-term effects. Our conclusion that teenage girls requesting ECP could benefit from an advance supply of ECP is supported by other researchers, who have also suggested other potential target groups such as women who undergo a legal abortion, condom users, and women who have recently given birth (Citation9-12).
Girls were scheduled for a structured telephone interview at 3, 6, and 12 months post enrolment. The follow-up procedure of this quite mobile target group of teenage girls required therefore thorough logistics and a flexible and creative set-up. In order to minimize drop-outs each girl received a notifying text message before the scheduled telephone call. Several attempts to call back were made in case the girls did not answer the first time or if they wished to reschedule the call to a different day or time. Having in mind the mobility of this age group, the drop-out rate of 38% 1 year after enrolment must be deemed as reasonable.
Research has shown that telephone interviews are equally reliable as face to face interviews (Citation13). It is our impression that most girls responded openly and honestly to our questions and were eager to provide information for the study, also 12 months post enrolment. It cannot be ruled out that the three follow-up calls had an effect on the girls, regardless of group belonging, and that awareness of contraception and emergency contraception may have improved during the study.
Our previous study on advance provision of ECP to teenage girls showed significantly quicker use of ECP at follow-up 3 and 6 months post intervention. From the results in this paper, we conclude that the results were maintained even after 12 months; one-dose advance supply of ECP to teenage girls requesting ECP shortens the time interval from unprotected intercourse to pill intake, without jeopardizing contraceptive use and/or increasing sexual risk-taking. Considering the clinical relevance of these results, we suggest that advance provision of ECP could be implemented as a routine preventive measure for this target group.
Acknowledgements
Funding from the Swedish Research Council and contribution from Bayer-Schering made this study possible.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Baecher L, Weaver MA, Raymond EG. Increased access to emergency contraception: why it may fail. Hum Reprod. 2009;24:815–19.
- Raine TR, Harper CC, Rocca CH, Fischer R, Padian N, Klausner JD, et al. Direct access to emergency contraception through pharmacies and effect on unintended pregnancy and STIs: a randomized controlled trial. JAMA. 2005;293:54–62.
- Gold MA, Wolford JE, Smith KA, Parker AM. The effects of advance provision of emergency contraception on adolescent women's sexual and contraceptive behaviors. J Pediatr Adolesc Gynecol. 2004;17:87–96.
- Foster DG, Raine TR, Brindis C, Rostovtseva DP, Darney PD. Should providers give women advance provision of emergency contraceptive pills? A cost-effectiveness analysis. Womens Health Issues. 2010;20:242–7.
- Polis CB, Schaffer K, Blanchard K, Glasier A, Harper CC, Grimes DA. Advance provision of emergency contraception for pregnancy prevention. Cochrane Database Syst Rev. 2007;18:CD005497.
- Meyer JL, Gold MA, Haggerty CL. Advance provision of emergency contraception among adolescent and young adult women: a systematic review of literature. J Pediatr Adolesc Gynecol. 2011;24:2–9.
- Ekstrand M, Larsson M, Darj E, Tydén T. Advance provision of emergency contraceptive pills reduces treatment delay: a randomised controlled trial among Swedish teenage girls. Acta Obstet Gynecol Scand. 2008;87:354–9.
- Glasier A, Fairhurst K, Wyke S, Ziebland S, Seaman P, Walker J, et al. Advanced provision of emergency contraception does not reduce abortion rates. Contraception. 2004;69:361–6.
- Falk G, Falk L, Hanson U, Milsom I. Young women requesting emergency contraception are, despite contraceptive counseling, a high risk group for new unintended pregnancies. Contraception. 2001;64:23–7.
- Nelson AL. Recent use of condoms and emergency contraception by women who selected condoms as their contraceptive method. Am J Obstet Gynecol. 2006;194:1710–15. discussion 1715–16.
- Larsson M, Aneblom G, Eurenius K, Westerling R, Tydén T. Limited impact of an intervention regarding emergency contraceptive pills in Sweden—repeated surveys among abortion applicants. Eur J Contracept Reprod Health Care. 2006;11:270–6.
- Schreiber CA, Ratcliffe SJ, Barnhart KT. A randomized controlled trial of the effect of advanced supply of emergency contraception in postpartum teens: a feasibility study. Contraception. 2010;81:435–40.
- Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qual Res. 2004;4:107–18.