Abstract
This paper addresses: 1) Situations where human behaviour is involved in relation to antibiotics, focusing on providers and consumers; 2) Theories about human behaviour and factors influencing behaviour in relation to antibiotics; 3) How behaviour in relation to antibiotics can change; and, 4) Antibiotic mainstreaming as an approach to facilitate changes in human behaviour as regards antibiotics. Influencing human behaviour in relation to antibiotics is a complex process which includes factors like knowledge, attitudes, social norms, socio-economic conditions, peer pressure, experiences, and bio-physical and socio-behavioural environment. Further, key concepts are often perceived in different ways by different individuals. While designing and implementing projects or programmes for behavioural change with respect to antibiotics for professionals or consumers it is helpful to consider theories or models of behaviour change, e.g. the ‘stages of change model', including pre-contemplation, contemplation, preparation, action, and maintenance. People in different stages of change are susceptible to different behaviour modification strategies. Application of marketing principles to ‘global good', so-called ‘social marketing', to improve ‘welfare of the individual and society' is gaining increased attention in public health. In conclusion, just providing correct knowledge is not sufficient although it is a pre-requisite for behaviour modification in the desired direction. We can never change the behaviour of any other human, but we can facilitate for others to change their own behaviour. One possibility is to implement ‘antibiotic mainstreaming' as a potentially effective way for behaviour modification, i.e. to address consequences for maintaining effective antibiotics in all activities and decisions in society.
Introduction
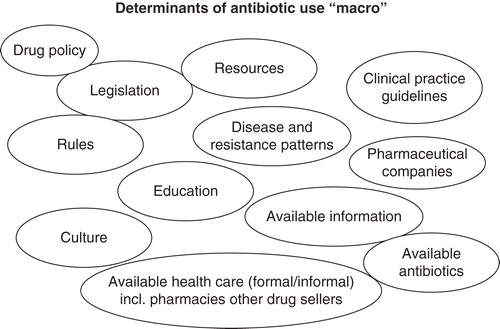
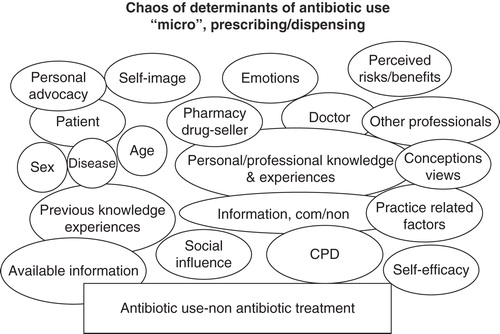
International as well as national strategies to manage antibiotic resistance often recommend awareness education for health care providers (e.g. doctors, pharmacists, nurses) as well as the public (Citation1–5). It is implicit in such strategies that they besides providing information should also lead to behaviour modification with regard to antibiotic prescribing, dispensing, or use and also include infection prevention and control. Interventions are, however, more likely to be effective if they while aiming at changing behaviour also take into account appropriate theories on behaviour changes as summarized in e.g. Finch et al. (Citation6) and utilize theories from behavioural and social sciences like ‘social marketing' (Citation7,8). Further, they need to acknowledge that people have varying understanding of concepts like ‘antibacterial resistance'. Qualitative studies among Swedish physicians show variations in views on antibacterial resistance from regarding it as ‘non-important in everyday practice' and also in the long-term perspective ‘a serious threat' both today and in the future (Citation9–11). It is increasingly acknowledged that a vast number of various intrinsic and extrinsic factors are involved in prescribing decisions (Citation12) as summarized in and . Variations have been observed in views among consumers for their own health-seeking (Citation13,14) and as care-takers regarding health-seeking behaviour in relation to childhood infections (Citation15). A similar variation in views of the problem of bacterial resistance and treatment of infections exists in varying settings and cultural contexts and among providers as well as consumers (Citation16–19) and is likely to occur also elsewhere. Such variations in views need to be understood and addressed when designing successful interventions aiming at changing human behaviour in relation to antibiotics.
Figure 2. Factors influencing prescribing or dispensing decisions at the micro level. Com/non: Commercial/non commercial
The aim of this paper is to present some theories on: 1) human behaviour, and on 2) changing behaviour of providers and consumers with respect to antibiotics and further to suggest some approaches for behaviour modification.
Behaviour definitions
There is no consensus on how to define behaviour. One attempt, however, based on a meta-analysis suggests that ‘behaviour is the internally coordinated responses (actions or inactions) of whole living organisms (individuals or groups) to internal and/or external stimuli' (Citation20).
Behaviours can be either innate (i.e. unreflected) or learned (unreflected or reflected) and can be regarded as any action of an organism that changes its relationship to its environment. Behaviour provides ‘outputs from the organism to the environment' (Citation21). Human behaviour refers to the range of behaviours performed by humans, influenced by a wide range of factors like culture, attitudes, emotions, values, ethics, authority, rapport, persuasion, coercion, and/or genetics. The way a human being acts is based on different factors like genetics, social norms, core faith, and attitudes (Citation16–19,22).
Situations where human behaviour is involved in relation to antibiotics and antibiotic resistance
Before antibiotics are prescribed, dispensed, consumed, or discarded, one or many decisions are taken influencing subsequent human behaviour. Someone, be it a physician, another human health care provider (Citation3,5,6,12,23), a veterinarian, an animal provider (Citation23–27), a consumer, or a parent (Citation13–15,28), is always involved. Non-human use of antibiotics, e.g. in animal husbandry, industries, and agriculture, is often not given the attention it deserves (Citation25) despite the fact that it constitutes an important part of the total antibiotic consumption and is very much influenced by human behaviour. Likewise, human behaviour is involved in the research, development, manufacturing, and sales of antibiotics, but that is not specifically addressed in this paper except as sales promotion influencing prescribing or dispensing ( and ). There is also involvement of human behaviour in the environmental spread and pollution with antibiotics and antibiotic-resistant bacteria or genetic element [e.g. (Citation29–32).]. Thus, modification of human behaviour is needed with respect to the environment as well. Other examples of involvement are infection prevention and control and hygiene (Citation33), in the decision to send a sample for culture, and in the laboratory in culturing bacteria, determining their susceptibility and communicating the results to the provider. These are all important areas where human behaviour is involved, but they are not specifically addressed in this paper.
Theories about human behaviour and factors influencing behaviour with regard to antibiotics
There are many different theories on human behaviour and behaviour modification. It has also been much debated why and how changes in behaviour occur and how various types of factors influence such changes. Some of these theories will be presented briefly below, and they have been related to changes in human behaviour in relation to antibiotics.
‘What determines human behaviour, and how do we explain that behaviour?' are helpful questions we can address as we try to figure out what motivates people to modify their behaviour and to accept suggestions for modification. As we understand this, we can also look into behaviour changes from all aspects of antibiotic prescribing, dispensing, use, and handling and also look into causes that lead to unnecessary use of antibiotics and think of ways and means to modify human behaviour to achieve our objectives.
Human behaviour can be influenced by a number of factors at a number of levels (Citation34). In relation to antibiotics there are five main levels: 1) Individual level—knowledge, attitudes, beliefs, and personality, which are summarized as individual motivation, e.g. in relation to prescribing when there is diagnostic uncertainty; 2) Interpersonal level—social identity, support, roles (formal role like a head in a work-place, or informal leader like information provider in a neighbourhood); an example in this area is the doctor–patient relationship in a prescribing situation; 3) Institutional level—rules, guidelines, regulations, and informal structures, where one example could be prescribing guidelines; 4) Community level—social networks, norms, e.g. liberal or restrictive prescribing; and 5) Public policy level—regulations and laws, for example if antibiotics are ‘prescription only drugs’ and if so, if that rule is followed.
All of these levels play a role in influencing how people behave in general and in relation to prevention and control of communicable diseases and prescription for antibiotics in particular. They thus need to be considered and addressed when behaviour changes for providers or consumers in relation to antibiotics are aimed at (Citation8,35,36).
How can provider behaviour in relation to antibiotics change?
Educational approaches
The traditional model of changing provider behaviour has been continuing medical education (CME), nowadays often referred to as continuing professional development (CPD), which often consists of ‘information passing', described as ‘pouring or pot-filling' from ‘teacher' to ‘student'. The sole application of such a model was criticized as early as in 1993 by Coles and Holm (Citation37) as such a linear communication cannot be considered optimal in the communication with providers who are often highly skilled professionals with vast experience. It has been known for long that providers' experiences and expectations (Citation38) as well as their values and norms (Citation22) are important to incorporate or address in educational programmes, but still often considered as a focus of research and not implemented in wider programmes (Citation8,39).
Educational models, encouraging reflection on practice, the use of feedback, and small-group learning including discussions are more likely to change behaviour. For quite some time, learning based on experiences and the necessity to link new knowledge or new ways of behaviour to already existing practices has been stressed (Citation38,40–42). Schön's model emphasizes ‘knowledge in action' and ‘surprise' as important drivers for professional change. The need to link theory to educational interventions aiming at changing antibiotic behaviour has also been emphasized (Citation6,8,43).
Utilizing theories for facilitating individual change
The ‘stages of change theory' or ‘the trans-theoretical model' was originally developed, describing the process a person goes through when giving up drinking or smoking (Citation44). However, the five stages in this theory, ‘pre-contemplation' (unaware of the problem, i.e. not thinking about change), ‘contemplation' (considering change in the future, but not ready for action), ‘preparation/decision' (planning for change), ‘action' (change is initiated), and ‘maintenance of changed behaviour' (i.e. repetition of the desired behaviour), could equally well be applied for a change in prescribing behaviour in general (Citation45,46) and prescribing of antibiotics in particular (Citation6). Persons in different stages of change are likely to be susceptible to different intervention strategies (Citation11). For those in the pre-contemplation phase must become aware, i.e. we need to give information and bring the problem and solution we are suggesting to their attention. People in the contemplation stage are aware of the dangers, e.g. of prescribing fluoroquinolones and how that can contribute to the resistance problem. They are thinking about changing in the future, but they have not as yet begun to change. A cognitive shift is occurring, but they have not tried the new behaviour as yet. They need some further inducement for change. The preparation/decision/determination stage is where people actually decide to change and they are ready to change their prescribing practices. As communicators, our task is to provide these people with background information and help them determine what the behavioural steps are. For example, how they practically can change prescribing behaviour. Can they substitute one unwanted antibiotic with a recommended one, or can they give the patient some advice instead of prescribing? The next stage of change is the action phase. People are now engaging in the new behaviour we are advocating. The new behaviour has to be practically implementable in their everyday life and the complex challenges they face in work, life, and society. If patients are not satisfied, or adverse effects occur, they need to know how to handle that. Finally, in the maintenance stage, people are repeating the desired behaviour they have chosen. It is one thing to try the new prescribing practice for a few times. It is much more challenging to continue the new practice and not relapse even when there is resistance from the environment, e.g. in the form of pharmaceutical promotion. If relapse occurs the whole process from pre-contemplation or contemplation may need to start again.
Changes in prescribing behaviour could also be seen in relation to the concept of the prescribers' ‘evoked set' of drugs (Citation47) and the process it takes to introduce a new drug within the evoked set. It might be relevant to compare ‘evoked sets' with pre-set alternatives in computers. Choosing one of these pre-set alternatives is easy, while it is very difficult to choose something which is not among these alternatives. From this theory it can also be envisaged that it is easier to substitute one drug with another one rather than to abstain from prescribing.
Utilizing theories for facilitating individual and system changes
The so-called Precede/Proceed (Precede: ‘Predisposing', ‘Reinforcing', ‘Enabling' ‘Constructs' in ‘Educational/ Environmental', ‘Diagnosis', ‘Evaluation'; and Proceed; ‘Policy', ‘Regulatory', ‘Organizational', ‘Constructs', ‘Educational', ‘Environmental', ‘Development') model was developed for adult health education programmes (Citation48). In this model, predisposing, enabling, and reinforcing factors are related to behavioural change. The model is used both for delivery of programmes in practice settings and when conducting behaviour change interventions. It offers a framework within which individual-level theories, community-level theories, interpersonal communication, interactive technologies, media campaigns, and grass roots organizing can be utilized. Predisposing factors are knowledge and attitudes, which promote or inhibit a specific behaviour, such as knowledge about resistance. Enabling factors are individual or organizational factors that facilitate an action, e.g. the availability of easily applicable treatment algorithms for various infectious diseases. Reinforcing factors are rewards or punishments that follow a particular behaviour. For example, when a new behavioural pattern is tried, e.g. prescribing in a different way than before, reinforcing factors could be positive comments on the new therapy by peers or positive feedback from patients. Such reinforcing factors are often necessary to establish the new behaviour (Citation49,50). These kinds of factors are related to motivation and to overcome barriers for changes, as described by Gray (Citation51).
Utilizing theories of interdependence for facilitating individual change
The relationship between the person, the behaviour, and the environment and an emphasis on self-directed learning as a natural process was described in the ‘social learning theory' (Citation52). Six concepts are important for the ways people learn to behave by watching others: 1) behavioural capability; 2) expectations; 3) self-efficacy; 4) observational learning; 5) reinforcement; and 6) social support. Social learning theory explains human behaviour in terms of continuous reciprocal interaction between cognitive, behavioural, and environmental influences. ‘Behavioural capability' includes how people watch others behave in a certain way and find that behaviour appeals, e.g. following a prescribing guideline. As public health change advocates we need to provide information and training, i.e. the knowledge and skills needed to motivate behaviour change about any new behaviour we want to implement, like for example suggesting ‘delayed' instead of ‘immediate' prescription. We also need to understand that people have ‘expectations' or beliefs about what they think will happen when they engage in the new behaviour. It is important to discuss what the likely results of the new behaviour will be and provide encouragement. This will give people a sense of the effects that will result when they change. The third concept is ‘self-efficacy', i.e. the belief a person has in his/her own ability to complete tasks and reach goals. It is, however, important not to suggest that people take action in situations where they do not have the control necessary to take those actions. We need to help people succeed by pointing out their strengths. Where do they have a good track record? Where are they already doing things similar to what we are suggesting? It is difficult to suggest abstaining from prescribing antibiotics even in what is likely to be a viral disease if it is not easy for the patient or parent to come back to the prescriber if the situation worsens. Then small group discussions might be helpful, where prescribers can listen to others who talk about how they tried to not prescribe antibiotics by giving testimonies and telling stories about following the guidelines and what worked for them.
The next concept of social learning is that of ‘observational learning'. If you observe other persons who are similar to you, like your peers, and see them behaving in the recommended way with good results, that will be a strong motivator for you to change, also referred to as a ‘role model'. We need to point out the experiences of others and point out the specific changes others have accomplished and give people realistic role models.
‘Reinforcement' is a fifth concept of the social learning model. The responses that people get to their behaviour are likely to influence whether they will engage in the new behaviour in the future or not. Positive reinforcement gives people a sense of encouragement, and provides incentives or rewards to continue that behaviour. Negative responses will have the opposite effect (compare above with the Precede/Proceed model).
Finally, the concept of social support is extremely important. Albrecht and Adelman (Citation53) have described this ‘as the kind of communication process that occurs between people, between providers of support and recipients of support that functions very specifically to help people reduce the uncertainty they face'. When uncertainty is reduced to a manageable level, particularly in situations of stress or a lack of confidence, then a sense of personal control results, which brings us back to self-efficacy because it is at that point that people feel they can engage in the change we are advocating. Further, awareness of a problem or a need on the part of the prospective adopter of a new technology was seen as important in a study on physicians' views of change processes (Citation54). As can be seen from the above, concepts and thoughts from the different models and theories are closely inter-linked and overlap. Common themes in all these models are the importance of other persons for inducing change and that change is a multifactorial event, complex to elicit.
Academic detailing
‘Academic detailing' is a concept introduced in the beginning of the 1980s in the area of educational outreach to improve drug prescribing (Citation55). It was originally based on the social marketing approach and includes elements of most of the above-mentioned theories. Theories on adult learning are, however, not explicitly addressed. Academic detailing has been summarized as follows (Citation55): 1) assessment of motivation for current practices and barriers to change; 2) focusing on specific physician categories; 3) developing objectives for the education; 4) establishing credibility; 5) encouraging participation; 6) using concise educational material; 7) repeating key messages; and 8) ideally providing reinforcement through more than one visit.
Academic detailing is often considered among the most effective ways of changing prescriber behaviour, as has been shown, for example, in relation to antibiotic behaviour in ambulatory care (Citation56). In general, higher complexity models often referred to as multi-faceted models seem to be effective in ambulatory care (Citation8,43,56). It is pointed out that behaviour and social science research are under-utilized in the development of prescribing interventions (Citation8). In hospital care several types of interventions were shown to be effective (Citation57). However, it should be pointed out that the design of the studies as well as the selected outcome measures may affect the possibility to interpret and generalize the results.
Advantages of educational approaches
It is important to note that educational interventions are relatively easy to implement in all kinds of settings as they can use local resource persons, which is relatively less costly (Citation2,58). Interventions or intervention models applicable to educated professionals can also, in modified versions, be implemented for less educated providers (Citation59,60).
How can consumer behaviour in relation to antibiotics change?
Consumers are of course in many ways similar to providers when it comes to changing behaviour, and all the theories mentioned above are more or less applicable to consumers as well. As mentioned above, the ‘trans-theoretical' or ‘stages-of-change model' (Citation44) was originally developed for changing the behaviour of laymen.
There are, however, some features of consumers that need to be considered. Firstly, they can be divided into at least three groups: 1) community members, not currently sick; 2) patients; and 3) parents of sick children. These three groups need partly different types of messages. Also within the groups there are wide variations in knowledge and previous experiences as well as in socio-economic background and other variables such as language. Further, consumers are many more compared with professionals. Thus, mass-communication strategies are more important. TV supported by radio, posters for health facilities, leaflets, etc. are often used in combination (Citation6,13). Social marketing is an increasingly recognized behaviour science approach to promote public health changes in individuals, groups, and societies and has been suggested, for example, in the prevention and control of communicable diseases (Citation61). The framework has also been suggested for the development, implementation, and evaluation of public campaigns on antibiotic use (Citation62).
There is an intricate web of interactions within the consumer group as well as between the professional and consumer group. Providers' perceptions of patients' demand for antibiotics as well as an actual demand by consumers of antibiotics influence antibiotic prescribing and dispensing (Citation10,12,16,17,35). Self-medication with antibiotics is a global issue (Citation13,16,17) which increases the access to antibiotics but also imposes an increased risk of unnecessary use of antibiotics, a trade-off which needs special attention. One possibility in areas with low access to formal health care providers is to acknowledge the importance of informal providers or non-physicians and educate them regarding, for example, antibiotic use as has been done in Tanzania (Citation63). It is, however, not certain that such initiatives lead to recommended behaviour (Citation63).
Earlier theories that have been suggested are e.g. Rogers's ‘diffusion of innovation' that was first described for the introduction of a new antibiotic (Citation64). In this theory people are divided into five groups depending on how quick they are to accept innovations, which could be a physical product as well as a new behaviour: innovators (2.5%), early adopters (13.5%), early majority (34%), late majority (34%), and laggards (16%). The change process is then characterized by several aspects. One is whether or not people perceive a ‘relative advantage'; what are the relative advantages and the unique benefits of the change? Is there some prestige associated with it? What is the cost or the saving? A second aspect is ‘compatibility'. The changes we suggest need to fit with the target groups' existing values, habits, experiences, and needs. ‘Complexity' is a third aspect. People are not likely even to try if the change is too complex or difficult to understand. The new behaviour has to be fairly uncomplicated, easy to perform and understand. ‘Trialability' is a key aspect; people must be able to try before they change completely. Otherwise the willingness to undertake the risk of change is usually limited. Further, change needs to be ‘observable'. It is the extent to which we perceive benefits of the change in tangible or visible results.
Antibiotic mainstreaming—a way to facilitate change?
Gender mainstreaming has been accepted as a concept for some time (Citation65). ‘Mainstreaming' for other issues like HIV/AIDS has also been attempted (Citation66). The original idea with mainstreaming is: 1) always to make the issue that is mainstreamed an integral part of all planning; 2) always to analyse each and every decision in society from the perspective of the mainstreaming issue; and 3) always to make visible the consequences arising out of it. Mainstreaming could be a useful approach for facilitating behaviour modification to maintain the continued effectiveness of antibiotics. It might decrease inappropriate and unnecessary antibiotic use. Antibiotic mainstreaming could potentially be a very successful, useful, helpful, valuable, effective, strong, and forceful way to facilitate all types of behaviour modifications that are needed in societies to maintain effective antibiotics. Mainstreaming can be implemented at different levels, e.g. at the programmatic, organizational, internal, inter-organizational, and educational level. One definition of mainstreaming at the organizational level is ‘mainstreaming is a strategy for policy implementation'. Although the exact definition of the term can be debated, its contents are fairly clear: that the issue at hand must be considered in all projects and lines of work in an organization. Hence, mainstreaming is the opposite of the alternative strategy of having specialized groups or units taking entire responsibility for a theme or issue. Mainstreaming, on the contrary, demands that the entirety of an organization's staff be involved in the implementation of a policy. A mainstreaming strategy could be viable to maintain the effectiveness of antibiotics. In all policy implementation and decisions in health care as well as in society as a whole, all decisions should be analysed if they have consequences for antibiotics or antibiotic resistance and if so how the resistance problem could be mitigated or the use of antibiotics could be as rational as possible. Mainstreaming would make the issue very visible and would facilitate for behaviour change. A few examples of how ‘antibiotic mainstreaming' could work will be given below, just to illustrate this new idea. The most obvious examples are from health care: in all decisions from cleaning to food handling, to the more obvious cases of disease management guidelines including prescribing recommendations, to recruitment of staff. Everywhere and always the consequences for infection prevention and control, antibiotic prescribing and antibiotic resistance must be considered. Also in the educational sector, for teachers, for parents, for day care centres, infection prevention and control as well as management of common childhood infections need to be emphasized together with how to identify danger signs to avoid delayed care-seeking in serious situations. Further, in city planning and environmental discussions, the potential spread of antibiotics and antibiotic-resistant bacteria and how to stop it, as well as how to implement effective infection prevention and control strategies need to be considered. In all types of reports and planning documents there should be a heading like ‘Implications for availability of effective antibiotics in the future'. For consumer products an ‘Antibiotic approval' like the ‘Environmental friendly' marking could be decided and implemented. Obviously a contextually appropriate perspective needs to be taken, and the considerations cannot be the same in all contexts (Citation67).
Concluding remarks
We can never change the behaviour of any other human being, but we can facilitate for others to modify their own behaviour. How can we best apply these theories and specific determinants presented above to our target groups, providers and consumers? The most effective way is to turn them into questions. For example, does self-efficacy affect behaviour X for the particular target population we are addressing? If it does, why? If not, why not? Theories, principles, and concepts are all about helping us to explain what we see happening or what we do not see happening. Changing providers' and/or consumers' behaviour is a complex process. Providing knowledge in the form of evidence is in itself not enough, even though it is in most cases a prerequisite for acquiring a required behaviour. In all cases, as unambiguous messages as possible need to be given to avoid misunderstanding. The application of theories of behavioural change in intervention studies as well as in implementation of interventions is an important strategy to attain successful changes in outcomes. Studies evaluating the effectiveness of various types of interventions are needed. However, as in all implementation research, the context is of great importance, whereas local validations of interventions will always be required. Antibiotic mainstreaming, i.e. always to consider the effects of various types of interventions and various types of decisions on future availability of antibiotics, could be a means to raise awareness and integrate potential behaviour modification with respect to antibiotics in all aspects of society. Antibiotic mainstreaming could thus be a successful, useful, helpful, valuable, effective, strong, and forceful way to facilitate all types of behaviour modifications that are needed in societies to maintain effective antibiotics.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- World Health Organization. Global strategy for containment of antimicrobial resistance. Geneva: World Health Organization; 2001.
- Okeke IN, Klugman KP, Bhutta ZA, Duse AG, Jenkins P, O'Brien TF, et al. Antimicrobial resistance in developing countries. Part II. Strategies for containment. Lancet Infect Dis. 2005;5:568–80.
- Mölstad S, Erntell M, Hanberger H, Melander E, Norman C, Skoog G, et al. Sustained reduction of antibiotic use and low bacterial resistance. A ten year follow-up of the Swedish STRAMA programme. Lancet Infect Dis. 2008;8:125–32.
- World Health Organization. The evolving threat of antimicrobial resistance: options for action. Geneva: World Health Organization; 2012. Available at http://whqlibdoc.who.int/publications/2012/9789241503181_eng.pdf. (accessed 20 January 2014).
- Chan YH, Fan MM, Fok CM, Lok ZL, Ni M, Sin CF, et al. Antibiotics nonadherence and knowledge in a community with the world's leading prevalence of antibiotics resistance: implications for public health intervention. Am J Infect Control. 2012;40:113–17.
- Finch RG, Metlay JP, Davey PG, Baker LJ; International Forum on Antibiotic Resistance colloquium (2002). Educational interventions to improve antibiotic use in the community: report from the International Forum on Antibiotic Resistance (IFAR) colloquium, 2002. Lancet Infect Dis. 2004;4:44–53.
- Stead M, Gordon R, Angus K, McDermott L. A systematic review of social marketing effectiveness. Health Educ. 2007;107:126–91.
- Charani E, Edwards R, Sevdalis N, Alexandrou B, Sibley E, Mullett D, et al. Behavior change strategies to influence antimicrobial prescribing in acute care: a systematic review. Clin Infect Dis. 2011;53:651–62.
- Bjorkman I, Erntell M, Roing M, Stalsby Lundborg C. Infectious disease management in primary care: perceptions of GPs. BMC Fam Pract. 2011;12:1.
- Björkman I, Berg J, Viberg N, Stålsby Lundborg C. Awareness of antibiotic resistance a prerequisite for restrictive antibiotic prescribing in UTI treatment. A qualitative study among primary care physicians in southern Sweden. Scand J Prim Health Care. 2013;31:50–5.
- Björkman I, Berg J, Röing M, Erntell M, Stålsby Lundborg C. Perceptions among Swedish hospital physicians on prescribing of antibiotics and antibiotic resistance. Qual Saf Health Care. 2010;19:e8.
- Teixeira Rodrigues A, Roque F, Falcão A, Figueiras A, Herdeiro MT. Understanding physician antibiotic prescribing behaviour: a systematic review of qualitative studies. Int J Antimicrob Agents. 2013;41:203–12.
- Sihavong A, Stålsby Lundborg C, Syhakhang L, Akkhavong K, Tomson G, Wahlström R. Antimicrobial self-medication for reproductive tract infections in two provinces in Lao PDR. Sex Transm Infect. 2006;82:182–6.
- Lan PT, Stålsby Lundborg C, Mogren I, Phuc HD, Chuc NTK. Lack of knowledge about sexually transmitted infections among women in North rural Vietnam. BMC Infect Dis. 2009;9:85.
- Hoa NQ, Öhman A, Stålsby Lundborg C, Chuc NTK. Drug use and health-seeking behavior for childhood illness in Vietnam - a qualitative study. Health Policy. 2007;82:320–9.
- Deschepper R, Grigoryan L, Stalsby Lundborg C, Hofstede G, Cohen J, Van Der Kelen G, et al. Are cultural dimensions relevant for explaining cross-national differences in antibiotic use in Europe? BMC Health Serv Res. 2008;8:123.
- Kotwani A, Wattal C, Katewa S, Joshi PC, Holloway K. Factors influencing primary care physicians to prescribe antibiotics in Delhi India. Fam Pract. 2010;27:684–90.
- Chandy SJ, Mathai E, Thomas K, Faruqui AR, Holloway K, Lundborg CS. Antibiotic use and resistance: perceptions and ethical challenges among doctors, pharmacists and the public in Vellore, south India. Indian J Med Ethics. 2013;10:20–7.
- Borg MA. National cultural dimensions as drivers of inappropriate ambulatory care consumption of antibiotics in Europe and their relevance to awareness campaigns. J Antimicrob Chemother. 2012;67:763–7.
- Levitis DA, Lidicker WZ, Freund G. Behavioural biologists don't agree on what constitutes behaviour. Anim Behav. 2009;78:103–10.
- Dusenbery DB. Living at micro scale. Cambridge, MA: Harvard University Press; 2009. p 124.
- Ajzen I. Attitudes, personality and behavior. Chicago, IL: Dorsey Press; 1988.
- Chandra Sahoo K, Tamhankar AJ, Johansson E, Stalsby Lundborg C. Antibiotic use, resistance development and environmental factors: a qualitative study among healthcare professionals in Orissa, India. BMC Public Health. 2010;10:629.
- Redding LE, Barg FK, Smith G, Galligan DT, Levy MZ, Hennessy S. The role of veterinarians and feed-store vendors in the prescription and use of antibiotics on small dairy farms in rural Peru. J Dairy Sci. 2013;96:7349–54.
- Tamhankar AJ, Nerkar SS, Patwardhan AP, Stalsby Lundborg C. Rural India perceives that use of antibiotic use in farm animals must be influencing antibiotic resistance development in humans: do the regulators think so? In Lawrence R, editor. Antimicrobial resistance: from emerging threat to reality. New Delhi, Chennai, Mumbai, Kolkata: Narosa Publishing House; 2009. p 118–28.
- Kvaale MK, Grave K, Kristoffersen AB, Norström M. The prescription rate of antibacterial agents in dogs in Norway - geographical patterns and trends during the period 2004-2008. J Vet Pharmacol Ther. 2013;36:285–91.
- Eltayb A, Barakat S, Marrone G, Shaddad S, Stålsby Lundborg C. Antibiotic use and resistance in animal farming: a quantitative and qualitative study on knowledge and practices among farmers in Khartoum, Sudan. Zoonoses Public Health. 2012;59:330–8.
- Sahoo KC, Tamhankar AJ, Johansson E, Stålsby Lundborg C. Community perceptions of infectious diseases, antibiotic use and antibiotic resistance in context of environmental changes: a study in Odisha, India. Health Expect. 2012; Epub ahead of print.
- Diwan V, Chandran S, Tamhankar AJ, Stalsby Lundborg C, Macaden R. Identification of ESBL and quinolone resistance genes in Escherichia coli isolated from hospital waste water from Central India. J Antimicrob Chemother. 2012;67:857–9.
- Diwan V, Stålsby Lundborg C, Tamhankar AJ. Seasonal and temporal variation in release of antibiotics in hospital wastewater: estimation using continuous and grab sampling. PLoS ONE. 2013;8:e68715.
- Diwan V, Tamhankar AJ, Khandal RK, Sen S, Aggarwal M, Marothi Y, et al. Antibiotics and antibiotic-resistant bacteria in waters associated with a hospital in Ujjain, India. BMC Public Health. 2010;10:414.
- Sahoo KC, Tamhankar AJ, Sahoo S, Sahu PS, Rosales Klintz S, Stålsby Lundborg C. Geographical variation in antibiotic-resistant Escherichia coli isolates from stool, cow-dung and drinking water. Int J Environ Res Public Health. 2012;9:746–59.
- Joshi SC, Diwan V, Tamhankar AJ, Joshi R, Shah H, Sharma M, et al. Qualitative study on perceptions of hand hygiene among hospital staff in a rural teaching hospital in India. J Hosp Infect. 2012;80:340–4.
- Rimer BK, Glanz K. Theory at a glance. A guide for health promotion practice, 2nd ed. U.S. Department of Health and Human Services. National Institute of Health. National Cancer Institute; 2005. p 35–43. Available at http://www.cancer.gov/cancertopics/cancerlibrary/theory.pdf. (accessed 20 January 2014).
- Oxford J, Goossens H, Schedler M, Sefton A, Sessa A, van der Velden A. Factors influencing inappropriate antibiotic prescription in Europe. Educ Prim Care. 2013;24:291–3.
- Harris DJ. Initiatives to improve appropriate antibiotic prescribing in primary care. J Antimicrob Chemother. 2013;68:2424–7.
- Coles C, Holm HA. Learning in medicine: towards a theory of medical education. In Coles C, Holm HA, editors. Learning in medicine. Oslo: Scandinavian University Press; 1993.
- Schön DA. Educating the reflective practitioner. New York: Jossey-Bass; 1987.
- Yardley L, Douglas E, Anthierens S, Tonkin-Crine S, O'Reilly G, Stuart B, et al. Evaluation of a web-based intervention to reduce antibiotic prescribing for LRTI in six European countries: quantitative process analysis of the GRACE/INTRO randomised controlled trial. Implement Sci. 2013;8:134.
- Schön DA. The reflective practitioner: how professionals think in action. New York: Basic Books; 1983.
- Mann KV. Educating medical students: lessons from research in continuing education. Acad Med. 1994;69:41–7.
- Ramsden P. Learning to teach in higher education. London: Rowntree; 1992.
- Stålsby Lundborg C. Information and interaction - influencing drug prescribing in swedish primary care. Stockholm: Karolinska Institutet; 1999.
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–14.
- Thomson O'Brien MA, Oxman AD, Davis DA, Haynes RB, Freemantle N, Harvey EL. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2000;(2): CD000409.
- Shirazi M, Zeinaloo AA, Parikh SV, Sadeghi M, Taghva A, Arbabi M, et al. Effects on readiness to change of an educational intervention on depressive disorders for general physicians in primary care based on a modified Prochaska model—a randomized controlled study. Fam Pract. 2008;25:98–104.
- Denig P. Drug choice in medical practice rationales, routines and remedies (dissertation). Groningen: Rijksuniversitet Groningen; 1994.
- Green LW, Eriksen MP, Schor EL. Preventive practices by physicians: behavioral determinants and potential interventions. Am J Prev Med. 1988;4:101–7.
- Tamblyn R, Battista R. Changing clinical practice: which interventions work? J Contin Educ Health Prof. 1993;13:273–88.
- Soumerai SB, Lipton HL. Evaluating and improving physician prescribing. In Strom BL, editor. Pharmacoepidemiology. 3rd ed. Chichester: John Wiley & Sons Ltd; 2000. p 483–503.
- Gray JAM. Evidence-based healthcare. How to make health policy and management decisions. Edinburgh: Churchill Livingstone; 1997.
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1977.
- Albrecht TL, Adelman MB. Communicating social support. Newbury Park, CA: Sage Publications; 1987.
- Geertsma RH, Parker RC, Krauss Whitbourne S. How physicians view the process of change in their practice behaviour. J Med Educ. 1982;57:752–68.
- Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing') to improve clinical decision making. JAMA. 1990;263:549–56.
- Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev. 2005:CD003539.
- Davey P, Brown E, Fenelon L, Finch R, Gould I, Hartman G, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. 2005:CD003543.
- Santoso B, Suryawti S, Prawaitasari JE. Small group intervention vs formal seminar for improving appropriate drug use. Soc Sci Med. 1996;42:1163–8.
- Chuc NTK, Larsson M, Falkenberg T, Do NT, Binh NT, Tomson G. Management of childhood acute respiratory infections at private pharmacies in Vietnam. Ann Pharmacother. 2001;35:1283–8.
- Stenson B, Syhakhang L, Stålsby Lundborg C, Eriksson B, Tomson G. Private pharmacy practice and regulation - a randomised trial in Lao P.D.R. Int J Technol Assess Health Care. 2001;17:579–89.
- MacDonald L, Cairns G, Angus K, Stead M. Evidence review: social marketing for the prevention and control of communicable disease. Stockholm: ECDC; 2012.
- Rosales S, Saliba EAM, Zacharias C, Stålsby Lundborg C. Course on the development, implementation and evaluation of prudent antibiotic use campaigns; Stockholm: ECDC; European Centre for Disease Prevention and Control (accepted for publication 2013).
- Minzi O, Manyilizu V. Application of basic pharmacology and dispensing practice of antibiotics in accredited drug-dispensing outlets in Tanzania. Drug Healthc Patient Saf. 2013;5:5–11.
- Rogers EM. Diffusion of innovations. 4th ed. New York, NY: Free Press; 1995.
- Ravindran TK, Kelkar-Khambete A. Gender mainstreaming in health: looking back, looking forward. Glob Public Health. 2008;3:121–42.
- Elsey H, Tolhurst R, Theobald S. Mainstreaming HIV/AIDS in development sectors: have we learnt the lessons from gender mainstreaming? AIDS Care. 2005;17:988–98.
- Tamhankar AJ. Location Specific Integrated Antibiotic Resistance Management Strategy (LIARMS). In Raghunath D, Nagaraja V, Durgarao C, editors. Antimicrobial resistance—the modern epidemic—current status and research issues. Bangalore: Macmillan Publishers; 2009. p 390–9.