Abstract
Background.Multidisciplinary rehabilitation programmes can improve physical functioning and help patients with long-term pain back to work. Little is known, however, of the extent to which such rehabilitation also affects life satisfaction, pain severity, and disability. We wanted to evaluate if a 5-week rehabilitation programme for patients with long-term pain improves life satisfaction and decreases pain severity and disability.
Methods. The subjects were 164 patients aged 18–65 years from a pain rehabilitation clinic. Most of them were referred from primary care units. One group of repeated tests was used. Participants were asked to fill out the LiSat-11 checklist and parts of the Multidimensional Pain Inventory (MPI), including pain severity, at admission, at discharge, and 1 year after the rehabilitation programme.
Results. Satisfaction with life as a whole, and six of ten LiSat-11 domains improved during the follow-up, though none reached the levels for the general population. MPI subscales pain severity, pain interference, life control, and affective distress improved, whereas no change was observed for general activity. Patients older than 38 years decreased more in MPI affective distress than younger patients. Gender, pain severity, and work status before the programme did not significantly influence the outcome.
Conclusions. The results indicate that multidisciplinary rehabilitation improves life satisfaction, reduces pain severity, and reduces negative psychological, social, and behavioural effects of pain. These outcome variables relate to domains known to be of interest for patients and should therefore be considered for evaluation of rehabilitation programmes for long-term pain.
Introduction
Pain rehabilitation programmes are offered patients with non-malignant pain for which single interventions such as pharmacological treatment or physiotherapy had been found to be insufficient. Programmes usually have a cognitive behavioural therapy approach, including measures to improve pain behaviour, cognitive restructuring, sleep strategies, stress management, psychosocial training, lifestyle adaptations to pain, pacing, and also physical exercise, ergonomics, body posture and co-ordination, relaxation techniques, Electromyography (EMG)-biofeedback, and strategies to maintain improvements. The length of the programmes varies, but they commonly last for 4–8 weeks. Systematic assessments of treatments for long-term pain (Citation1–6) indicate that multidisciplinary rehabilitation programmes containing a combination of psychological interventions and physical training can improve functioning and help patients back to work. However, little is known of the extent to which such rehabilitation also improves satisfaction with life, reflecting important changes on a truly personal level. The Life Satisfaction checklist (LiSat-11) (Citation7,8) is a self-report checklist reflecting satisfaction with life as a whole as well as satisfaction with 10 specific domains, and is an attempt to approach this ideal. Previous studies have shown that life satisfaction is very low among patients with long-term pain (Citation9,10) and that domains of LiSat-11 improve after pain rehabilitation (Citation11,12).
The primary aim of the present study was to evaluate if multimodal pain rehabilitation can improve life satisfaction and emotional well-being, and reduce disability, in both the short and the long term. A second aim was to test the sensitivity for change of LiSat-11 as a short- and long-term outcome instrument after treatment designed to improve these outcome variables. LiSat-11 results are here combined with the Multidimensional Pain Inventory (MPI) (Citation13), an instrument designed to measure disability and psychological, social, and behavioural aspects of chronic pain. These outcome domains relate to what long-term pain patients themselves believe to be important when evaluating the effectiveness of pain treatment (Citation14). In addition, we studied how the results varied with certain patient factors: gender, age, employment status, and pain severity.
Material and methods
Subjects
The participating subjects were 164 patients diagnosed with long-term non-malignant pain, aged 18–64 years. Subjects were selected from patients consecutively referred to the Uppsala University hospital pain rehabilitation clinic mostly from local general practitioners, company doctors, and hospital specialist clinics. This clinic is well established and has a long tradition in the evaluation and treatment of patients with long-term pain using a multidisciplinary approach.
All patients had their medical and functional status assessed by a multidisciplinary rehabilitation team during two half days. Patients were accepted for the pain rehabilitation programme and this study when the assessment had demonstrated rehabilitation needs related to long-term pain. It was considered realistic to reach improvement for those accepted. Patients with severe depression and/or drug or alcohol abuse were excluded. Additionally, to be eligible for inclusion patients had to be able to speak Swedish and to be able to fill in questionnaires.
Of the 164 patients accepted for the pain rehabilitation programme, 10 (6%) were excluded because they did not complete the first set of questionnaires, and 21 patients (12.8%) because they did not complete the second set at discharge just after the end of the programme (). Sixty-five (40%) did not complete the questionnaire one year after finishing of the programme. Thus, from the 164 patients referred to the programme, 133 completed the follow-up just after the end of the programme and 68 patients completed the 1-year follow-up. Mean duration of pain before the programme was 5.7 years (SD 1,826 days), and about 4 years (SD 1,314 days) for those who responded at one year after the programme. Further patient data including demographic data and main pain location are shown in . A comparison between categories in indicates that the drop-out between baseline and 12-month follow-up was rather evenly distributed between categories.
Figure 1. Flow chart showing those who attended the programme and filled in questionnaires at the different time points.
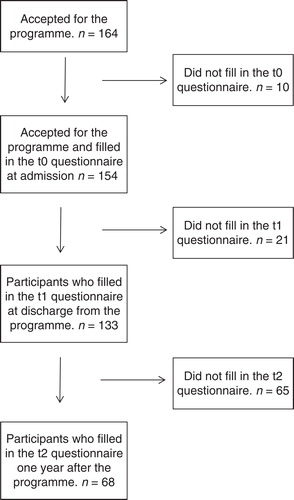
Table I. Demographic data.
Rehabilitation programme and questionnaires
The pain rehabilitation programme in this study followed generally used approaches. Part of the programme had a cognitive behavioural approach. Important ingredients were education, cognitive restructuring, psychosocial training, physical exercise, ergonomics, positioning, balance and co-ordination, relaxation, pacing, body awareness, and practising activity structuring and balancing. Groups of about 8 (range 6–9) patients participated in the programme for 5 weeks, 5 days a week, 7 hours a day. Interventions were performed mostly in groups, led by one or several pain rehabilitation professionals. Self-practice exercises were followed up weekly during the programme. The rehabilitation team consisted of a physician specialized in pain rehabilitation (in charge of the programme), a physiotherapist, an occupational therapist, a social counsellor, a psychologist, and a nurse.
Patients were assessed at admission (t0), at discharge from the programme (t1), and 1 year after the programme (t2). Patients received three sets of questionnaires at three different time points, directly handed over or by mail. Questionnaires were filled in at home before the programme, at the clinic at the end of the programme, and at home 1 year after the programme. No reminders were sent. The questionnaires were parts of the Swedish National Quality Registry for Pain Rehabilitation (NRS). They included socio-demographic data including off-work period, pain duration, The West-Haven Yale Multidimensional Pain Inventory ((WHY)MPI), and the Life Satisfaction checklist (LiSat-11).
The Life Satisfaction checklist (LiSat-11) (Citation7,8) is a self-report checklist. The responses are given on a 6-point numeric scale. Swedish population norms for LiSat-11 can be found in a previously published study (Citation7) for comparison. This earlier study also included tests of construct validity and reliability.
The (WHY)MPI (Citation13) is a self-report questionnaire constructed to describe aspects of dysfunction, disability, and participation restrictions. It is divided in three sections (impact of pain on patients' life, responses of others to patients' communication of pain, and participation in common daily activities). There are 61 items distributed among 13 composite scales. Responses are given on a 7-point Likert scale. The MPI has shown sound psychometric properties (Citation13). A Swedish translation of the original English version provided by the NRS committee, including all 61 questions, was used in the present study. However, only the results of five MPI subscales are reported in the present study: pain severity, pain-related interference in everyday life, perceived life control, affective distress, and general activity level.
Statistics
All statistics were computed using SPSS 11.5 software. A Q-Q plot was used to explore if data for the 10 LiSat-11 domains, and for life as a whole, and MPI scales followed approximate normal distributions. To evaluate changes in Life Satisfaction and MPI over the 1-year follow-up a series of repeated measures analyses of variance (ANOVA) were used. Pairwise comparisons post hoc were performed by using Scheffé's method. The aim of pairwise comparisons was to evaluate contrasts between the measurements. Changes between t0 and t1 were analysed with paired t test. All p Values below 0.05 were considered as statistically significant.
Ethics
A Swedish ethics committee has previously confirmed that the national use of the questionnaires in the NRS register is ethically acceptable. The local ethics committee in Uppsala found that the design of the present study did not require further formal ethical consideration (Dnr 2004: M-381).
Results
There was no statistically significant difference in demographic data such as age and gender, national origin, level of education, and source of income among the patients who completed the questionnaires at 1 year (t2; n = 68) and those that did not (data not presented). Patients responding at t0 reported pain duration of 2,074 days (SD 1,826), and those at t2 1,473 days (SD 1,314).
Paired t tests showed significant improvements between admission (t0) and at discharge just after the end of the programme (t1) regarding satisfaction with life as a whole, vocation, leisure, sexual life, psychological health, and somatic health (). MPI scales showed significant decreases in pain severity, pain interference, life control, and affective distress ().
Table II. Changes in LiSat-11 domains and MPI scales over time.
Repeated measures ANOVAs showed that significant improvement had occurred across 1 year for LiSat-11 life as a whole and the six following LiSat-11 domains: vocation, leisure, contacts, sexual life, somatic health, and psychological health (; ). Absolute numbers showed gradual improvements from t0 to t1, and from t1 to t2 for vocation, leisure, somatic health, sexual life, and psychological health. LiSat-11 life as a whole improved from t0 to t1 and remained unchanged from t1 to t2. LiSat-11 contacts improved from t0 to t2. None of the improvements reached the levels reported for the reference sample (Citation7). Satisfaction with economy, activity of daily life (ADL), family life, and partner relationship did not change significantly.
Figure 2. LiSat-11 outcome over time. Values represent all patients that filled in questionnaires at the different time points. Mean values, 1–6. Reference group = mean life satisfaction calculated from data collected from a nationally representative Swedish sample of 2,533 people (Citation7); * = significant change over time, based on those that responded at all three time points.
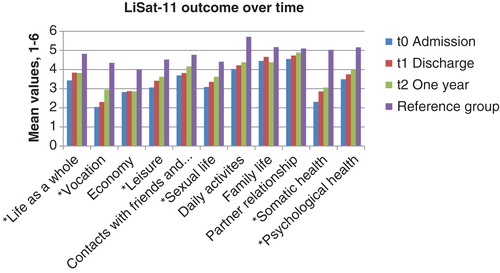
Table III. Changes in LiSat-11 domains and MPI scales over time.
Repeated measures ANOVAs testing of the MPI scales showed that significant improvements had occurred across 1 year for four of the MPI scales: pain severity, interference, life control, and affective distress (; ). Since only two patients provided answers to the index general activity level at 12-month follow-up it was not possible to carry out further statistical analyses with regard to these data.
Figure 3. MPI outcome over time. Values represent all patients that filled in questionnaires at the different time points. Data used for ‘General activity level' ‘after one year' are based on only two patients and were not used for statistical analysis. * = Significant change over time based on those that responded at all three time points.
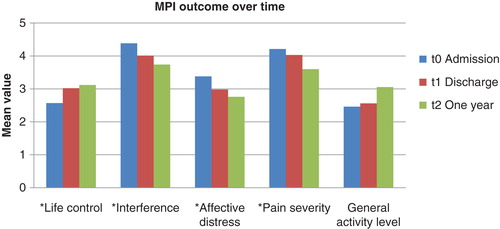
Although the MPI variables except general activity level improved significantly both at t1 and t2 compared with t0, neither gender nor pain severity nor work/not work had an effect on the general outcome of the programme as measured by LiSat-11 and MPI. However, age had a significant effect on the MPI scale affective distress both at discharge immediately after the programme (Wilks's λ = 0.967, F(1, 127) = 4.29, p = 0.04) and across 1 year (Wilks's λ = 0.920, F(1, 55) = 4.78, p = 0.033). Patients aged 38 years (median age in the study group) and above decreased their distress significantly more than patients younger than 38 years.
Discussion
Methodological considerations
The patients participating in this study are not likely to represent patients with long-term pain in general. For example, only those with severe rehabilitation needs were admitted to the programme, and patients with substance abuse and severe depression were excluded. Furthermore, since we lack a formal control group, it is not known to what extent the rehabilitation programme or confounders such as the course of time or other interventions influenced the results. However, as the participants had a mean duration of pain of about 6 years before they started the rehabilitation programme it seems unlikely that the improvements observed during the programme and in the follow-up had other explanations than the rehabilitation intervention itself.
A large proportion of patients responded to the questionnaires at t1 (81.1%), giving the results from t0 to t1 more validity than changes from t1 to t2. The response rate at t2 was considerably lower (41.5%). The reason for the high dropout rate was not analysed but is likely to be due to the long period of no contact and low motivation. Reminders were not sent as this was not included in the research plan. Lack of reminders, shame due to lack of adherence to the rehabilitation plan (e.g. exercises), disappointment of the results, and even the opposite, considerable improvements, may have contributed to the high dropout at t2. Furthermore, non-responders tended to be those with longer pain duration before the programme commenced. The significance and possible causal link of this association are unclear but make the conclusion after 1 year comparatively stronger for those with shorter pain duration. There was no significant difference, however, in demographic data between the patients who completed the questionnaires at 1 year and those who did not.
Life satisfaction
Life satisfaction may be best explained as the degree to which an individual experiences himself as being able to attain his goals (Citation15). This concept implies that the level of overall life satisfaction (life as a whole) is associated with specific life satisfaction domains, depending upon the extent to which individual activity goals are perceived as vital. Improvement in life satisfaction may reflect either improved functioning and/or reduced and more realistic goals. A rehabilitation programme may have both effects. In both cases, the gap between the present situation and the goal the individual experiences himself as being able to attain would have decreased, and hence the life satisfaction increased.
Satisfaction with somatic health gradually improved from t0 to t1, and from t1 to t2. Previous investigators (Citation7,16) reported that satisfaction with health correlated to satisfaction with life as a whole, indicating that satisfaction with somatic health is important for satisfaction with life as a whole. Satisfaction with psychological health gradually increased from t0 to t2. This is likely to be related to improvements in the MPI scales life control, and decreases in affective distress and pain interference. We suggest that the MPI and LiSat-11 partly supplement each other as tools to describe how functional impairments and aspects of disability relate to life satisfaction domains (Citation17). Similar results were found for vocation and leisure.
MPI
A high level of positive correlation has previously been shown for the following LiSat-11 domains/MPI scale pairs: psychological health/life control and negative correlation for psychological health/pain interference and for psychological health/affective distress (Citation17). In accordance with this, the present findings show that changes in these LiSat-11/MPI pairs after a rehabilitation programme seem to be associated in a similar way.
The results of the present study show a decrease in MPI pain severity at discharge directly after the programme, and that this had continued further after 1 year. Previous studies of multidisciplinary pain rehabilitation have shown various results regarding reduction of pain intensity (Citation18–20). Interestingly, a decrease in MPI scale scores for pain severity and interference at discharge immediately after the pain rehabilitation programme decreased the risk of being on full-time sick leave 1 year later (Citation21). It is not possible to infer from the concept ‘pain severity' used in this study to what extent it relates to pain intensity or other aspects of pain, including pain tolerance and suffering.
Effects of age, pain severity, gender, and work/not work
None of the factors pain severity, gender, or work/not work had a significant impact on the general outcome of the programme regarding LiSat-11 life as a whole or the measured MPI- scales. The only factor that emerged was age; patients aged 38 years and above showed significantly less affective distress after the programme compared with patients younger than 38 years. The importance of this single positive statistical finding must be interpreted with caution, but is in accordance with findings by Persson et al. (Citation22). It is possible that older age may be associated with more expectations of pain as a part of everyday life and therefore less affective distress. Thus, as no clear differences between demographic groups were found, it would be illogical to give for instance patients without employment and those with higher age lower priority to programmes such as that in focus in this study.
Women and men did not differ significantly in satisfaction with life as a whole and measured MPI scales after the rehabilitation programme in this study. Previous studies have shown conflicting results (see (Citation23–28)).
There was no difference over time between patients with pain severity above median 4.3 (calculated from index scores) and below in life as a whole and the other measured MPI scales. This result is not in line with previous studies showing that more intense pain was prognostic for greater improvements during rehabilitation (Citation29,30). There is no clear explanation for this discrepancy. Likewise, there was no difference between patients in work compared with those not working across time in life as a whole and the measured MPI scales. This is in keeping with a previous study showing that being at work did not affect improvement after a rehabilitation programme for patients with chronic low back pain (Citation29). However, also these results must be interpreted with caution as only 27% of the patients in our study were engaged in vocational work.
Conclusions
The results of this study indicate that multidisciplinary rehabilitation is an effective method to improve life satisfaction and to reduce pain severity and negative psychological, social, and behavioural effects of pain.
The rehabilitation programme affected Life Satisfaction (LiSat-11) and MPI domains regardless of gender, level of pain severity, work status, and age {18–37 or 38–65 years).
Patient groups with a mean duration of pain of 4 years may experience lasting improvements in functioning and well-being by participating in a multidisciplinary rehabilitation programme.
Acknowledgements
We thank participating patients for answering the questionnaires, the staff at the Pain Rehabilitation Clinic, Uppsala University Hospital for handling the data, Dr Roland Melin and Professor Axel Fugl-Meyer for critical reading of the manuscript, and the Swedish National Institute for Public Health for providing us with data on the Swedish general population. The study was supported by Government funds. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49:221–30.
- Nachemson A, Carlsson C-A, Englund L, Goossens M, Harms-Ringdahl K, Linton S, et al. SBU – The Swedish Council on Technology Assessment in Health Care. 2000;145.
- Schonstein E, Kenny DT, Keating J, Koes BW. Work conditioning, work hardening and functional restoration for workers with back and neck pain. Cochrane Database Syst Rev. 2003;CD001822.
- Nielson WR, Weir R. Biopsychosocial approaches to the treatment of chronic pain. Clin J Pain. 2001;17:S114–27.
- Oliver K. A review of multidisciplinary interventions for fibromyalgia patients: where do we go from here? J Musculoskeletal Pain. 2001;9:63–80.
- Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47:670–8.
- Fugl-Meyer AR, Melin R, Fugl-Meyer KS. Life satisfaction in 18- to 64-year-old Swedes: in relation to gender, age, partner and immigrant status. J Rehabil Med. 2002;34:239–46.
- Melin R, Fugl-Meyer KS, Fugl-Meyer AR. Life satisfaction in 18- to 64-year-old Swedes: in relation to education, employment situation, health and physical activity. J Rehabil Med. 2003;35:84–90.
- Silvemark AJ, Källmén H, Portala K, Molander C. Life satisfaction in patients with long-term non-malignant pain - relation to demographic factors and pain intensity. Disabil Rehabil. 2008;30:1929–37.
- Stålnacke BM. Life satisfaction in patients with chronic pain - relation to pain intensity, disability, and psychological factors. Neuropsychiatr Dis Treat. 2011;7:683–9.
- Merrick D, Sjolund BH. Patients' pretreatment beliefs about recovery influence outcome of a pain rehabilitation program. Eur J Phys Rehabil Med. 2009;45:391–401.
- Merrick D, Sundelin G, Stalnacke BM. One-year follow-up of two different rehabilitation strategies for patients with chronic pain. J Rehabil Med. 2012;44:764–73.
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain. 1985;23:345–56.
- Turk DC, Dworkin RH, Revicki D, Harding G, Burke LB, Cella D, et al. Identifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with pain. Pain. 2008;137:276–85.
- Fugl-Meyer AR, Bränholm I-B, Fugl-Meyer KS. Om tillfredställelse, lycka och rehabilitering [On satisfaction, happiness and rehabilitation]. Socialmed Tidskr. 1992;1:33–41.
- Willits FK, Crider DM. Health rating and life satisfaction in the later middle years. J Gerontol. 1988;43:172–6.
- Silvemark AJ, Källmén H, Portala K, Molander C. Life satisfaction in patients with long-term non-malignant pain - relating LiSat-11 to the Multidimensional Pain Inventory (MPI). Health Qual Life Outcomes. 2008;6:70.
- Härkäpää K, Mellin G, Jarvikoski A, Hurri H. A controlled study on the outcome of inpatient and outpatient treatment of low back pain. Part III. Long-term follow-up of pain, disability, and compliance. Scand J Rehabil Med. 1990;22:181–8.
- Niemistö L, Lahtinen-Suopanki T, Rissanen P, Lindgren KA, Sarna S, Hurri H. A randomized trial of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain. Spine (Phila Pa 1976). 2003;28:2185–91.
- Kääpä EH, Frantsi K, Sarna S, Malmivaara A. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: a randomized trial. Spine (Phila Pa 1976). 2006;31:371–6.
- Nyberg VE, Novo M, Sjölund BH. Do Multidimensional Pain Inventory scale score changes indicate risk of receiving sick leave benefits 1 year after a pain rehabilitation programme? Disabil Rehabil. 2011;33:1548–56.
- Persson E, Lexell J, Eklund M, Rivano-Fischer M. Positive effects of a musculoskeletal pain rehabilitation program regardless of pain duration or diagnosis. PM R. 2012;4:355–66.
- Marnetoft SU, Selander J, Bergroth A, Ekholm J. Factors associated with successful vocational rehabilitation in a Swedish rural area. J Rehabil Med. 2001;33:71–8.
- Keogh E, McCracken LM, Eccleston C. Do men and women differ in their response to interdisciplinary chronic pain management? Pain. 2005;114:37–46.
- Krogstad BS, Jokstad A, Dahl BL, Vassend O. Relationships between risk factors and treatment outcome in a group of patients with temporomandibular disorders. J Orofac Pain. 1996;10:48–53.
- Jensen IB, Bergström G, Ljungquist T, Bodin L, Nygren AL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: are the effects dependent on gender? Pain. 2001;91:65–78.
- Jensen IB, Bergström G, Ljungquist T, Bodin L. A 3-year follow-up of a multidisciplinary rehabilitation programme for back and neck pain. Pain. 2005;115:273–83.
- Sjöström R, Alricsson M, Asplund R. Back to work–evaluation of a multidisciplinary rehabilitation programme with emphasis on musculoskeletal disorders. A two-year follow-up. Disabil Rehabil. 2008;30:649–55.
- van der Hulst M, Vollenbroek-Hutten MM, Groothuis-Oudshoorn KG, Hermens HJ. Multidisciplinary rehabilitation treatment of patients with chronic low back pain: a prognostic model for its outcome. Clin J Pain. 2008;24:421–30.
- Baltov P, Cote J, Truchon M, Feldman DE. Psychosocial and socio-demographic factors associated with outcomes for patients undergoing rehabilitation for chronic whiplash associated disorders: a pilot study. Disabil Rehabil. 2008;30:1947–55.

