Abstract
Purpose. Anterior plate fixation has been reported to provide satisfactory results in cervical spine distractive flexion (DF) injuries stages 1 and 2, but will result in a substantial failure rate in more unstable stage 3 and above. The aim of this investigation was to determine the biomechanical properties of different fixation techniques in a DF-3 injury model where all structures responsible for the posterior tension band mechanism are torn.
Methods. The multidirectional three-dimensional stiffness of the subaxial cervical spine was measured in eight cadaveric specimens with a simulated DF-3 injury at C5–C6, stabilized with four different fixation techniques: anterior plate alone, anterior plate combined with posterior wire, transarticular facet screws, and a pedicle screw–rod construct, respectively.
Results. The anterior plate alone did not improve stability compared to the intact spine condition, thus allowing considerable range of motion around all three cardinal axes (p > 0.05). The anterior plate combined with posterior wire technique improved flexion–extension stiffness (p = 0.023), but not in axial rotation and lateral bending. When the anterior plate was combined with transarticular facet screws or with a pedicle screws–rod instrumentation, the stability improved in flexion–extension, lateral bending, and in axial rotation (p < 0.05).
Conclusions. These findings imply that the use of anterior fixation alone is insufficient for fixation of the highly unstable DF-3 injury. In these situations, the use of anterior fixation combined with a competent posterior tension band reconstruction (e.g. transarticular screws or a posterior pedicle screws–rod device) improves segmental stability.
Introduction
Distractive flexion stage 3 injury (DF-3) of the cervical spine is characterized by rupture of the posterior soft tissue elements causing instability in flexion (Citation1). Both facet joints are dislocated, and there is a translational deformity not exceeding 50% (). In order to dislocate both facet joints all posterior structures including the posterior annulus fibrosus and the posterior longitudinal ligament (PLL) must be ruptured (Citation2). There still is a clinical debate on how best to manage these injuries surgically. An anterior approach has obvious advantages. However, when the posterior annulus is ruptured, disk fragments may shift into the spinal canal when the facet joints are reduced (Citation3-9). An anterior plate fixation is technically simple, and the fusion is under compression, thus optimizing bone healing. The anterior approach leaves the patient with less pain and stiffness (Citation10), and provides acceptable clinical outcomes (Citation11). Also, the patient does not have to be turned to the prone position with a highly unstable injury, when placed on the operation table.
Figure 1. Schematic drawing of the distractive–flexion stage 3 injury, DF-3. The upper vertebra is dislocated in flexion in relation to the lower one. Both facet joints are dislocated, but the overall anterior displacement is less the 50%. An observation from the creation of the injury in the specimen was that the posterior longitudinal ligament had to be torn in order to allow dislocation of the joints.

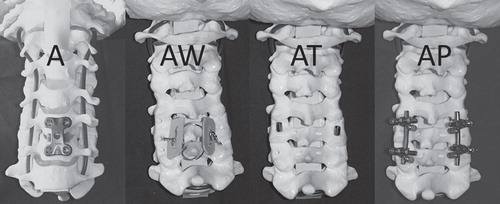
However, Koller et al. (Citation12) reported a 31% incidence of construct failure in patients treated with an anterior plate alone, and Henriques et al. (Citation13) also reported high failure rates in patients with DF-3 injuries and concomitant severe neurological injury when managed with anterior reconstruction alone. From a biomechanical standpoint, it is hypothesized that anterior fixation alone is less than ideal for a DF-3 stage injury—characterized by significant posterior column disruption. When the posterior tension band fails, the only remaining stabilizing structures are located anteriorly. A stand-alone anterior plate reconstruction technique will be positioned close to these structures—providing suboptimal stability for a posterior column injury. Angle stable screws that lock to the plate will improve stabilization of the construct (Citation14); however, the addition of posterior fixation will create a more ideal biomechanical situation (Citation15-23). Using an in vitro human cadaveric cervical spine model with distractive–flexion stage 3 injury at C5–C6, the present study aims to quantify the multidirectional stability provided by four different reconstruction techniques: anterior plate fixation alone (A), and combined with one of three posterior fixation techniques—triple wire technique (Citation24) (AW), transarticular facet joint screws (Citation25) (AT), or a posterior pedicle screw–rod device (AP).
Materials and methods
Preparation and experimental groups
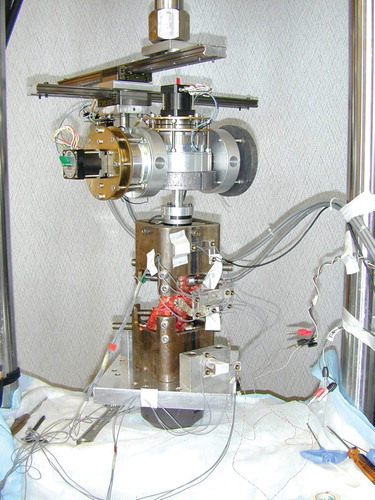
Eight human cadaveric spines from C1 to T2 were harvested from fresh cadavers (5 males and 3 females; age range 49–82 years, mean 67 years), frozen immediately in double-wrapped plastic bags and stored at −20°C until testing. Pre-experimentation radiographs were obtained to identify and exclude any specimen that demonstrated spinal pathology. Prior to biomechanical testing, the specimens were thawed to room temperature and the surrounding soft tissue and muscles were removed, with care being taken to preserve osseous and pertinent ligamentous structures. Prior to biomechanical testing, all specimens were sectioned at C2–C3 proximally and T1–T2 interbody levels. The C3–C4 (proximal) and C7–T1 (distal) motion segments were rigidly fixed with bone screws, with care taken not to disrupt the operative C5–C6 site and adjacent proximal (C4–C5) and distal (C6–C7) intervertebral levels. The specimens were mounted to the six-degree-of-freedom spine simulator with transfixation pins and polyester adhesive resin (Bondo®, 3M Corporation, St. Paul, MN, USA) at C3–4 and C7–T1, respectively, leaving the motion segments C4–C5, C5–C6, and C6–C7 unconstrained (). The specimens were kept moistened with saline during the mechanical testing, which never exceeded 8 hours (Citation26).
To enable each specimen to serve as its own control, the specimens were first tested intact and then tested after destabilization and reconstruction at the C5–C6 level. The destabilization consisted of simulating a distractive flexion injury stage 3 (DF-3) by transecting the C5–C6 supraspinous ligament, interspinous ligament, facet joint capsules, ligamentum flavum, posterior longitudinal ligament, and the posterior half of annulus fibrosus. The facet joints were then manually dislocated and reduced.
Spinal constructs
The spinal specimens were reconstructed and tested in the following order.
Anterior plate (A): Anterior plate reconstruction with the cervical spine locking plate (CSLP, DePuy-Synthes, Inc. Raynham, MA, USA) device and tricortical interbody bone graft between C5 and C6. The CSLP plate has monocortical angle stiff locking screws. Angle stable screws improve stability compared to plates with non-locking screws (Citation20). This necessitated transecting of the remaining annulus fibrosus and the anterior longitudinal ligament. The bone graft was harvested from the parietal bone of the cranium of the same cadaver that was tested.
Anterior plate–wire (AW): The anterior plate was left in place. A Bohlman triple wire reconstruction using 1-mm stainless steel wire and bone graft from the parietal bone of the cranium of the same specimen was added (Citation24). The wire was tightened manually with pliers until just before the wire started to cut into the bone substance. To standardize this procedure, the same surgeon performed the wire application in all specimens, trying to use the same force each time.
Anterior plate–transarticular facet screws (AT): The posterior wire reconstruction was removed, and 3.5-mm standard bone screws were applied as transarticular facet joint screws bilaterally over the C5–C6 facet joints. The screw holes were drilled with a 2.5-mm drill bit. The screw hole was tapped with an appropriate tap both in the proximal and distal facets.
Anterior plate–pedicle screw instrumentation (AP): The OC Fixation System was utilized (Anatomica AB, Göteborg, Sweden). The transarticular screws were removed, and 4.0-mm pedicle screws were implanted into C5 and C6 bilaterally. The screw holes were prepared according to the recommendation by the manufacturer by first probing the pedicles with a blunt probe, then tapping the hole with the appropriate tap. Longitudinal 3.5-mm rods were then applied to complete the fixation device ().
Multidirectional flexibility analysis
Multidirectional flexibility testing was performed utilizing a custom-designed six-degree-of-freedom spine simulator interfaced with an OptoTrak 3020 motion analysis system (OptoTrak 3020, Northern Digital Inc., Waterloo, Ontario, Canada) and Labview Software (National Instruments Corporation, Austin, TX, USA). The six-degree-of-freedom gimbal apparatus contains three independent stepper motors, harmonic drives, and electromagnetic clutches, which apply pure, unconstrained rotational moments (±) about three axes—X, Y, and Z. Unconstrained translations (±) are permitted using linear bearing guide rails (X and Z) and 858 Bionix Materials Testing System (MTS) servo-controlled linear actuator (Y axis) (MTS Systems Corporation, Eden Prairie, MN, USA) (). The intact and reconstructed cervical motion segments were evaluated under axial rotation (Y axis, ±1.5 Nm), flexion/extension (X axis, ±1.5 Nm), and lateral bending (Z axis, ±1.5 Nm) testing modes using a pure moment loading condition. Intersegmental motion was quantified using specialized rig markers containing three non-co-linear infrared light-emitting diodes (LEDs) rigidly attached to the vertebral elements at C5 and C6 and oriented to permit detection by an optoelectronic motion analysis system. Each test was repeated for three loading and unloading cycles at a rate of three degrees/second, with data from the third cycle used for computational analysis.
Statistical analysis
For non-destructive multidirectional flexibility analysis, the peak intervertebral range of motion (Euler angles, degrees) for each loading mode was calculated as the sum of motions [maximum ± rotation for torsion, flexion–extension, and left + right bending (degrees)] observed at the third loading cycle range-of-motion (RoM). The raw data set consisted of angle measurements around three axes (FE: flexion–extension, LB: lateral bending, and AR: axial rotation) for the intact condition and following reconstruction using four different preparations: A, AW, AT, and AP. The analysis data set was created from the raw data set by normalizing the angles dividing them by the corresponding value for the intact specimen, e.g. (FE, angular plate angle)/(FE, intact angle). The resulting value was expressed as a percentage. Thus, the value 100 indicates that the angle was identical to the corresponding angle for the intact condition. The three rotational axes (FE, LB, and AR) were analyzed separately. For each axis, the four stabilization methods were compared pairwise. As the data failed to show normality when examined with the Shapiro–Wilk W test, the Wilcoxon signed ranks test for paired data was utilized. The target parameter is the pseudomedian for the difference in percentage discussed above. The pseudomedian of a variable x is the median of (x–y)/2, where y is an independent copy of x. For symmetric distributions, it coincides with the ordinary median. Results are presented as 95% confidence intervals. No correction has been made for multiple testing. The missing value for specimen 1, FE, AP is disregarded in these analyses. Thus, comparisons to this group have been made on seven pairs only, as opposed to the other ones, performed on eight pairs. One should note that the statistical power of these analyses is limited due to the small sample size. Hence, moderately large p values should not be interpreted as strong evidence against any difference between the groups.
The data analysis was performed using R version 3.0.2.
Results
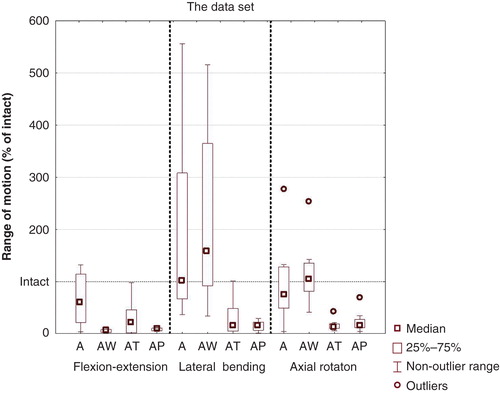
During the multidirectional testing of the reconstruction with anterior plate alone, the 95% CI of range-of-motion (RoM) was 19–116 percentage points (pp) of the intact spine in flexion–extension which was close to but not significant (p = 0.15) (; ). A closer analysis of the data revealed that the anterior plate alone provided stability mainly in extension whereas the stability in flexion was poorer. The 95% CI for the RoM for lateral bending was 67–375 pp of intact (p = 0.38), and for axial rotation it was 34–180 pp of intact (p = 0.55). Thus, in none of the tested modes did the anterior plate alone provide improved stability compared to the normal mobility of the intact spine.
Table I. The data set. Values are percentages (angle/ intact angle).
Figure 4. Boxplots of the data set for the different testing moments. Data have been normalized and expressed as the percentage of range-of-motion for the intact specimen for each test sequence.
Flexion–extension
When posterior instrumentation was added to the anterior plate alone construct (A), the stability improved for all the applied techniques: with Bohlman wire construct (AW) the segmental range of motion decreased by 59 pp compared to A (p = 0.023), with the transarticular screws (AT) it decreased by 28 pp compared to A (p = 0.008), and with the pedicle screw construct (AP) it decreased by 66 pp compared to A (p = 0.031). There were no significant differences between the different posterior techniques in flexion–extension (p = 0.22) ().
Table II. Analysis of flexion–extension. Reconstruction methods in the left column have been compared to methods in the top row. Thus, values above zero mean that the method to the left gives larger values than the method above. Entries are: Estimate (CI) p.
Lateral bending
When the anterior plate stabilization was supplemented with the Bohlman wire construct (AW) there was no improvement in stability in lateral bending compared to the stability provided by the anterior plate alone (p = 0.38). When the anterior plate was combined with transarticular facet screws (AT) or a pedicle screw construct (AP), the segmental range of motion decreased by 121 pp compared to A (p = 0.039) and 131 pp compared to A (p = 0.008), respectively. The AT (–158 pp; p = 0.016) and AP constructs (–171 pp; p = 0.008) were significantly more stable when compared to the AW construct. There was no difference between the AT and AP constructs in lateral bending (p = 0.25) ().
Table III. Analysis of lateral bending. Reconstruction methods in the left column have been compared to methods in the top row. Thus, values above zero mean that the method to the left gives larger values than the method above. Entries are: Estimate (CI) p.
Axial rotation
When the anterior plate stabilization was supplemented with the Bohlman wire construct (AW) there was no improvement in stability in axial rotation compared to the stability provided by the anterior plate alone (p = 0.31). When the anterior plate was combined with transarticular facet screws (AT) or a pedicle screw construct (AP) the segmental range of motion decreased by 71 pp compared to A (p = 0.016) and 62 pp compared to A (p = 0.039), respectively. The AT (–94 pp; p = 0.008) and AP constructs (–86 pp; p = 0.008) were significantly more stable when compared to the AW construct. There was no difference between the AT and AP constructs in axial rotation (p = 0.64) ().
Table IV. Analysis of axial rotation. Reconstruction methods in the left column have been compared to methods in the top row. Thus, values above zero mean that the method to the left gives larger values than the method above. Entries are: Estimate (CI) p.
Discussion
Methodology—DF-3 injury procedure
In patients traumatized with a DF-3 injury, the extent of insufficiency of the posterior tension band mechanism probably varies, resulting in a pronounced instability. In order to dislocate both facets on the specimen, all posterior ligaments including the PLL and the posterior part of the intervertebral disc were transected. In further preparation, the anterior longitudinal ligament was sectioned and anterior disc removed in order to place the bone graft, leaving only the anterolateral remnants of annulus fibrosus to stabilize the operative motion segment. Hence, the tested specimens were more unstable than most clinical cases where the muscles and fasciae may contribute to stability (Citation27). Also, the tested specimens were most likely older and with a decreased bone quality compared to the average patient, which correlates with inferior purchase of screws (Citation28).
Due to the scarcity of human cadaver specimens, we chose to perform non-destructive testing and omitted cyclic loading in spite of the known importance of this as shown by Weis et al. in a bovine DF-3 model. They described fatigue failure in extension–flexion in two out of six specimens with posterior wire fixation, and in one specimen with anterior plate alone (Citation19). Thus, our study probably overestimates the stabilization provided by anterior plate alone and anterior plate combined with posterior wiring.
The purpose of this study was to evaluate how the stability was affected by adding different posterior fixations to an anterior fixation. In the clinical situation anterior exploration has certain advantages and may therefore be some surgeons’ first choice, although many would consider a ‘posterior alone’ fixation for these injuries, especially when a previous MRI has shown that no disk fragment has been dislodged to the spinal canal. We are also fully aware that posterior wire techniques probably have very little clinical use nowadays, but we wanted to see the effect of this technique mainly as a historical reflection.
Stability of the cervical reconstructions
Anterior plate alone
When reconstructed with A, the range of motion equaled the intact spine in axial rotation and lateral bending, whereas the stability in flexion–extension was only marginally improved. A detailed analysis of the flexion–extension data revealed that the anterior plate stabilized foremost in extension, and was poorer in flexion. In a DF-3 injury, the posterior tension band mechanism is absent. Therefore, a flexural moment will rotate the motion segment anteriorly, separating its posterior structures. An anterior plate will resist the moment close to the axis of segmental rotation. As a result, the fixation device by itself has to withstand the flexion moment. In extension, on the other hand, the posterior structures are compressing the bone graft, and the anterior plate will serve to improve stability of the anterior tension band mechanism. The fact that an anterior plate only stabilizes the motion segment at one point probably explains why the device performs comparably poorly in axial rotation and lateral bending.
In agreement with the present results and clinical experience (Citation12,13), several studies have indicated poor properties of an anterior plate alone for reconstruction of a three-column ligamentous injury, in contrast to some reports on good clinical results (Citation11,29-32). One explanation may be that in a series of patients the severity of the injuries varies also within the same fracture class. Incomplete disruption of the PLL may provide enough posterior tension band to allow a successful result with an anterior plate alone. Another explanation may be that the stability provided by an anterior plate, although weaker than the combined reconstructions, may be sufficient for patients where the bone stock is of good quality. Some support for this latter hypothesis is provided by a biomechanical report in a DF-3 injury model (Citation33). However, their specimens were all male and considerably younger (mean age 44 years, range 21–65) compared to those utilized in the current study 67 years (range 49–82), which could indicate better bone quality.
Anterior plate and Bohlman triple wire technique
This two-point fixation (one anteriorly, one posteriorly) is effective in restricting motions in extension–flexion compared to when the spine is fixed with an anterior plate alone, as the posterior tension band mechanism is reconstructed. The wires connect to the spinous processes providing a longer lever arm for the posterior component compared to the other posterior fixation techniques in the study, which may explain the slightly higher stiffness in extension–flexion compared to these techniques. However, the reduced stabilization demonstrated in axial rotation loading may be secondary to the inability to tighten a stainless steel wire, creating enough compression, and thus friction, between the bone surfaces. The wire resists tension loads, whereas axial and lateral bending moments are poorly controlled. In axial rotation, the geometry of the triple wire construct is almost 90 degrees with respect to the rotational moment, thus explaining the poor results.
Anterior plate and transarticular facet screws or pedicle screw–rod fixation
The combination of an anterior plate with transarticular facet screws or pedicle screw–rod device rigidly stabilizes at three circumferential points around the operative motion segment. This three-point fixation effectively controls the applied rotational moments as no significant difference could be detected between these two fixation techniques. Hence, from a biomechanical point of view they are similar, but they differ significantly from a clinical point of view. The transarticular facet screw technique is difficult to implant superior to C4 due to the prominence of the occiput. It is often difficult to locate the correct screw trajectory, without coming in conflict with the cranium. Also, the facets have to be perfectly reduced in order for this screw technique to be applicable. If the facets are subluxed, too little bone may be available for the screw canal, posing a risk for fracture or nerve root compromise when the screw is inserted.
The cervical pedicle screw technique described by Abumi and Kaneda (Citation34), on the other hand, can be applied superior to C4. It permits for segmental compression over the rod, thus aiding in the facet reduction. This technique has been demonstrated to improve segmental fixation and stability (Citation35) and probably offers the best purchase in the cervical spine (Citation36). There are obvious neurovascular risks involved in placing cervical pedicle screws, and from a clinical point of view safer techniques such as lateral mass screws have been shown to be sufficient (Citation37). However, for the present study, pedicle screws were included as they probably offer the best stabilization that can be achieved in the cervical spine.
It is possible that other anterior constructs, e.g. utilizing plates with bicortical screws and/or other designs of the bone graft may have yielded better results for the ‘anterior fixation alone’, but as we do not have any data on such constructs we cannot comment on this any further. Other fixation devices primarily designed for anterior cervical fusion in degenerative conditions have also been tested biomechanically in fracture models. Two low-profile devices—intracorporal cages with locked and variable angle screw anchorage, respectively—were compared in a recent study (Citation38). Both devices had very similar features. The authors concluded that the stability provided by the locked screw device probably was sufficient for distractive-flexion stage 3 injury if combined with an external immobilization, while the device with variable angle screws was not suited for patients with distractive-flexion injuries.
Conclusions
In this in vitro study using human spine specimens we evaluated four fixation methods in a DF-3 injury of the cervical spine. We found that anterior plate fixation alone is not sufficient to stabilize a DF-3, but by combining it with a competent posterior tension band reconstruction, i.e. transarticular facet screws or pedicle screw–rod instrumentation, segmental stability is improved.
Acknowledgements
Funding was provided by Orthopaedic Associates Research Foundation, Inc., Towson, Maryland, USA. Cervical spinal implants were provided by Anatomica AB, Göteborg, Sweden. The statistical analysis was performed by Lars Lindhagen, PhD, biostatistician at Uppsala Clinical Research Center, Uppsala, Sweden.
Declaration of interest: None of the authors has any conflict of interest with regard to the content of this article.
References
- Allen BL, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7:1–27.
- Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilibrand AS, Albert TJ. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine. 2001;26:1866–72.
- Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991;73:1555–60.
- Olerud C, Jónsson H. Compression of the cervical spine cord after reduction of fracture dislocations. Report of 2 cases. Acta Orthop Scand. 1991;62:599–601.
- Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg Br. 1992;74:224–7.
- Berrington NR, van Staden JF, Willers JG, van der Westhuizen J. Cervical intervertebral disc prolapse associated with traumatic facet dislocations. Surg Neurol. 1993;40:395–9.
- Doran SE, Papadopoulos SM, Ducker TB, Lillehei KO. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79:341–5.
- Moraes AC, Serdeira A, Pereira Filho A, Zardo E, Deitos J. Soft tissue injuries associated with traumatic locked facets in the cervical spine. Paraplegia. 1995;33:434–6.
- Vaccaro AR, Falatyn SP, Flanders AE, Balderston RA, Northrup BE, Cotler JM. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine. 1999;24:1210–17.
- Jónsson H, Cesarini K, Petrén-Mallmin M, Rauschning W. Locking screw-plate fixation of cervical spine fractures with and without ancillary posterior plating. Arch Orthop Trauma Surg. 1991;111:1–12.
- Kim KH, Cho DC, Sung JK. The management of bilateral interfacetal dislocation with anterior fixation in cervical spine: comparison with combined antero-posterior fixation. J Korean Neurosurg Soc. 2007;42:305–10.
- Koller H, Reynolds J, Zenner J, Forstner R, Hempfing A, Maislinger I, et al. Mid- to long-term outcome of instrumented anterior cervical fusion for subaxial injuries. Eur Spine J. 2009;18:630–53.
- Henriques T, Olerud C, Bergman A, Jónsson H. Distractive flexion injuries of the subaxial cervical spine treated with anterior plate alone. J Spinal Disord Tech. 2004;17:1–7.
- Spivak JM, Chen D, Kummer FJ. The effect of locking fixation screws on the stability of anterior cervical plating. Spine. 1999;24:334–8.
- Sutterlin CE, McAfee PC, Warden KE, Rey RM, Farey ID. A biomechanical evaluation of cervical spinal stabilization methods in a bovine model. Static and cyclical loading. Spine. 1988;13:795–802.
- Coe JD, Warden KE, Sutterlin CE, McAfee PC. Biomechanical evaluation of cervical spinal stabilization methods in a human cadaveric model. Spine. 1989;14:1122–31.
- McLain RF, Aretakis A, Moseley TA, Ser P, Benson DR. Sub-axial cervical dissociation. Anatomic and biomechanical principles of stabilization. Spine. 1994;19:653–9.
- Bueff HU, Lotz JC, Colliou OK, Khapchik V, Ashford F, Hu SS, et al. Instrumentation of the cervicothoracic junction after destabilization. Spine. 1995;20:1789–92.
- Weis JC, Cunningham BW, Kanayama M, Parker L, McAfee PC. In vitro biomechanical comparison of multistrand cables with conventional cervical stabilization. Spine. 1996;21:2108–14.
- Spivak JM, Bharam S, Chen D, Kummer FJ. Internal fixation of cervical trauma following corpectomy and reconstruction. The effects of posterior element injury. Bull Hosp Jt Dis. 2000;59:47–51.
- Do Koh Y, Lim TH, Won You J, Eck J, An HS. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine. 2001;26:15–21.
- Kim SM, Lim TJ, Paterno J, Park J, Kim DH. A biomechanical comparison of three surgical approaches in bilateral subaxial cervical facet dislocation. J Neurosurg Spine. 2004;1:108–15.
- Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VK, Papadopoulos SM, et al. Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine. 2005;30:915–22.
- Stathoulis B, Govender S. The triple wire technique for bifacet dislocation of the cervical spine. Injury. 1997;28:123–5.
- Klekamp JW, Ugbo JL, Heller JG, Hutton WC. Cervical transfacet versus lateral mass screws: a biomechanical comparison. J Spinal Disord. 2000;13:515–18.
- Panjabi MM, Krag M, Summers D, Videman T. Biomechanical time-tolerance of fresh cadaveric human spine specimens. J Orthop Res. 1985;3:292–300.
- Nolan JP, Sherk HH. Biomechanical evaluation of the extensor musculature of the cervical spine. Spine. 1988;13:9–11.
- Ryken TC, Clausen JD, Traynelis VC, Goel VK. Biomechanical analysis of bone mineral density, insertion technique, screw torque, and holding strength of anterior cervical plate screws. J Neurosurg. 1995;83:325–9.
- Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989;25:491–502.
- Aebi M, Zuber K, Marchesi D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine. 1991;16:S38–45.
- Ripa DR, Kowall MG, Meyer PR, Rusin JJ. Series of ninety-two traumatic cervical spine injuries stabilized with anterior ASIF plate fusion technique. Spine. 1991;16:S46–55.
- Moerman J, Harth A, Van Trimpont I, Uyttendaele D, Verdonk R, Claessens H, et al. Treatment of unstable fractures, dislocations and fracture-dislocations of the cervical spine with Senegas plate fixation. Acta Orthop Belg. 1994;60:30–5.
- Paxinos O, Ghanayem AJ, Zindrick MR, Voronov LI, Havey RM, Carandang G, et al. Anterior cervical discectomy and fusion with a locked plate and wedged graft effectively stabilizes flexion-distraction stage-3 injury in the lower cervical spine: a biomechanical study. Spine. 2009;34:E9–15.
- Abumi K, Kaneda K. Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine. 1997;22:1853–63.
- Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine. 1994;19:2529–39.
- Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine. 1997;22:977–82.
- Pitzen T, Lane C, Goertzen D, Dvorak M, Fisher C, Barbier D, et al. Anterior cervical plate fixation: biomechanical effectiveness as a function of posterior element injury. J Neurosurg. 2003;99:S84–90.
- Wojewnik B, Ghanayem AJ, Tsitsopoulos PP, Voronov LI, Potluri T, Havey RM, et al. Biomechanical evaluation of a low profile, anchored cervical interbody spacer device in the setting of progressive flexion-distraction injury of the cervical spine. Eur Spine J. 2013;22:135–41.