Abstract
Background. Current ultrasound protocols to measure carotid intima-media thickness (CIMT) in trials rather differ. The ideal protocol combines high reproducibility with a high precision in the measurement of the rate of change in CIMT over time and with a precise estimate of a treatment effect. To study these aspects, a post-hoc analysis was performed using data from two randomized double-blind, placebo-controlled trials: one among 872 subjects with familial hypercholesterolemia (FH) and the other among 752 subjects with mixed dyslipidemia (MD), respectively. Participants were randomized to torcetrapib or placebo on top of optimal atorvastatin therapy.
Methods. CIMT information was collected from the left and right carotid artery from two walls (the near and far wall) of three segments (common carotid, bifurcation, and internal carotid artery) at four different angles (right: 90, 120, 150, and 180 degrees on Meijer's carotid arc; left: 270, 240, 210, and 180 degrees, respectively). Based on combinations of these measurements, 60 different protocols were constructed to estimate a CIMT measure per participant (20 protocols for mean common CIMT, 40 protocols for mean maximum CIMT). For each protocol we assessed reproducibility (intra-class correlation coefficient (ICC), mean difference of duplicate base-line scans); 2-year progression rate in the atorvastatin group with its standard error (SE); and treatment effect (difference in rate of change in CIMT between torcetrapib and placebo) with its SE.
Results. Reproducibility: ICC ranged from 0.77 to 0.91 among FH patients and from 0.68 to 0.86 among MD patients. CIMT progression rates ranged from −0.0030 to 0.0020 mm/year in the FH trial and from 0.00084 to 0.01057 mm/year in the MD trial, with SE ranging from 0.00054 to 0.00162 and from 0.00083 to 0.00229, respectively. The difference in CIMT progression rate between treatment arms ranged from −0.00133 to 0.00400 mm/year in the FH trial and from −0.00231 to 0.00486 mm/year in the MD trial. The protocol with the highest reproducibility, highest CIMT progression/precision ratio, and the highest treatment effect/precision ratio were those measuring mean common CIMT with measurements of the near and far wall at multiple angles. When the interest is in the mean maximum CIMT, protocols using multiple segments and angles performed the best.
Conclusion. Our findings support the position that the number and specific combination of segments, angles, and walls interrogated are associated with differences in reproducibility, magnitude, and precision of progression of CIMT over time, and treatment effect. The best protocols were mean common CIMT protocols in which both the near and far walls are measured at multiple angles.
Trial registration: ClinicalTrials.gov identifier: NCT00136981.
Trial registration: ClinicalTrials.gov identifier: NCT00134264.
Key messages
Our findings support the opinion that the number and specific combination of segments, angles, and walls interrogated are associated with differences in reproducibility, magnitude and precision of progression of carotid intima-media thickness (CIMT) over time.
The choice for an ultrasound protocol to mea sure CIMT should depend on a well consi dered balance of differences in reproducibility and magnitude and precision of progression of CIMT over time before the study is carried out.
Not all CIMT measurements are the same; neither do they reflect the same process.
Introduction
Carotid intima-media thickness (CIMT) is a non-invasive marker of atherosclerotic vascular disease that has been studied extensively since 1986 (Citation1). CIMT is widely used in observational and intervention studies to assess determinants of atherosclerosis and its consequences for cardiovascular events (Citation2–23). In addition, change in CIMT over time is currently used as an alternative for cardiovascular events as primary outcome in intervention studies (Citation24–26).
Measurements can be made of the near and/or the far wall along the common carotid artery (CCA), the carotid bifurcation (BIF), and the internal carotid artery (ICA) at different angles of insonation. At present there is quite some diversity in the choice of ultrasound protocols used to measure CIMT. The most commonly used ultrasound protocols allow CIMT measurements to be taken from different combinations of segments (CCA; CCA and BIF; CCA, BIF, and ICA), walls (only far wall; both far and near wall), and angles (single angle, or a combination of angles). Moreover, with these parameters at least two different CIMT outcome measures can be estimated: the mean common CIMT and the mean maximum CIMT. The mean common CIMT is estimated as the mean value of the mean CIMT measurements that are performed over a 10 mm part of the far wall or both the far and near wall of the common carotid artery segment. The mean maximum CIMT is a summary measure that is computed as the mean of the single maximum CIMT measurements that are measured in 6 to 12 standard carotid artery walls: the far wall or both the far and near wall of the two or three distinct carotid artery segments: the common carotid segment, the carotid bifurcation, and the internal carotid artery segment at both the left and right sides.
For the choice of which ultrasound protocol (based on combination of segments, angles, and walls measured) would be most optimal, many issues are important, including the reproducibility of the method; the ability of the method to assess change over time (the CIMT rate of progression); and the ability of the method to show an effect of treatment. Up until now, formal evaluations of differences in methodological aspects between ultrasound protocols are rather limited (Citation27).
We set out to determine, in post-hoc analyses using the RADIANCE 1 and RADIANCE 2 studies, the protocol that could provide the best balance between reproducibility, magnitude of CIMT change over time and its associated precision, and magnitude of effect of intervention on CIMT change over time and its associated precision.
Methods
General
We used data of the RADIANCE 1 (Citation28,Citation29) and RADIANCE 2 (Citation29,Citation30) studies. These studies have been described in detail before. In summary, RADIANCE 1 was a double-blind randomized placebo-controlled multi-center trial in which 850 patients with heterozygous familial hypercholesterolemia (FH) were randomly assigned to receive either atorvastatin monotherapy or atorvastatin combined with 60 mg of torcetrapib for 2 years to study the effect on CIMT progression. RADIANCE 2 was a comparable study, a double-blind, placebo-controlled multi-center trial in which 752 participants with mixed dyslipidemia (MD) were randomly assigned to atorvastatin monotherapy or atorvastatin combined with 60 mg of torcetrapib for 2 years to assess the effect of torcetrapib, a cholesteryl ester transfer protein (CETP) inhibitor, on the progression of atherosclerosis, by measuring the thickening of carotid intima-media.
Carotid ultrasound examinations
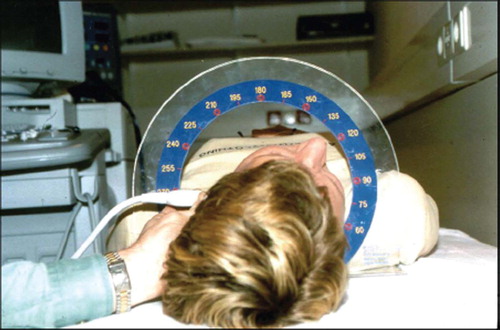
The ultrasound protocol for assessment of the carotid intima-media thickness has been described in detail elsewhere (Citation29). In short, duplicate scans were made at base-line and at each patient's final visit and single scans at visits at 6, 12, and 18 months, to give a maximum of seven scans for each patient. At each visit sonographers acquired and recorded CIMT images of 12 artery wall segments of the near and far walls of the right and left carotid artery for the common, bifurcation, and the internal carotid artery segments. In the trials a time slot of 45 minutes for image acquisition of one participant was recommended. The segments were defined as the common carotid artery (CCA) (from 10 to 20 mm proximal to the tip of the flow divider (TFD)), carotid bifurcation (from the TFD to 10 mm proximal to the TFD), and the proximal 10 mm of the internal carotid artery (ICA). At each segment images were collected at four predefined angles of 30° steps (90° to 180° on the right side and 270° to 180° on the left side) using Meijer's carotid arc (). This resulted in 48 possible measurements per patient. All imaging centers used the same imaging acquisition protocol and equipment (Sequoia 512 scanners equipped with 8L5 transducers; Siemens AG, Munich, Germany). A total of 48 5-second image sequences (video clips) were saved in DICOM format (Digital Imaging in Communications in Medicine; National Electrical Manufacturers Association, Rosslyn, VA, USA). Imaging data were transferred directly from the study sites to the two reading centers (Vascular Imaging Center, University Medical Center, Utrecht, the Netherlands, and Wake Forest University Medical Center, Ultrasound Reading Center, Winston-Salem, NC, USA), where standardized equipment and protocols were used to process stored images. From every image sequence, readers selected one frame in end-diastole for measurement of carotid intima-media thickness. For each image sequence, the reader selected one frame for measurement when the heart is in systole (elctrocardiogram (ECG) tracing is on QRS complex). One-centimeter lengths of leading edge (far wall) and trailing edge (near wall) of media-adventitia and blood-intima boundaries were traced within the region of interest specified by the reader using an automated edge detection program (Artery Measurement System software; Chalmers University, Gothenburg, Sweden (Citation31)). Maximum CIMT was determined from a set of measurements perpendicular to the media-adventitia boundary. Quality assurance protocols have been described elsewhere (Citation29). In short, the sonographers and readers received a uniform training and underwent a uniform predefined certification procedure. Furthermore, quality assurance was continued during the conduct of the trial. Also, two sonographer/reader meetings were scheduled during the study to discuss the issue at hand, to reinforce the important work the sonographers did, and to suggest potential improvements, when appropriate. The quality assurance/quality control (QA/QC) was initiated to attempt to keep the quality of imaging at the highest level.
Assessment of various protocols to measure CIMT
By selecting CIMT information of different combinations of segments, angles, walls, and both carotid arteries, 20 ultrasound protocols were constructed to estimate a mean common CIMT value and 40 ultrasound protocols to estimate a mean maximum CIMT value, resulting in a total of 60 ultrasound protocols (). The protocols that have been used in the analyses of the RADIANCE 1 and RADIANCE 2 studies were protocol 50 for the mean maximum CIMT and protocol 10 for the mean common CIMT.
Table I. The 60 different ultrasound protocols constructed using the study data on segments, walls, and angles measured.
Data analysis
The CIMT estimates of each ultrasound protocol were compared on reproducibility, rate of CIMT progression, and effect of intervention on change of CIMT over time with its associated precision.
Reproducibility was assessed in two ways. Intra-class correlation coefficients (ICC) and the mean difference of the duplicate CIMT scan at base-line with its corresponding standard deviation were calculated for all protocols, and the protocols were ranked by the level of the ICC (the higher, the better) and the standard deviation (SD) of the mean difference (the lower, the better). The ideal and best protocol would have a mean difference of zero with a small variation around this mean difference.
Annual CIMT progression rate in the comparison group (atorvastatin only) was calculated by subtracting the mean CIMT value of the two duplicate scans at base-line from the mean CIMT value of the two duplicate scans at end of study and dividing by 2. In this group the rate of CIMT progression was expected to be slowed down and pointing towards zero, as lipid-lowering trials have shown statins to hold progression (Citation32). Precision of CIMT progression was defined by the standard error (SE). To obtain a parameter that weighs the magnitude of the progression rate and the precision of the measurement, an absolute progression/precision (PP) ratio was constructed by dividing the mean progression rate by its SE and transforming this value into its absolute value. The absolute value was chosen as it is unknown whether atorvastatin treatment would only slow down CIMT progression or would even cause regression (negative rate of progression). The protocols were ranked by this absolute PP ratio from small to large, with the largest value defined as the protocol that achieved the best balance between CIMT progression rate and precision, as ideally one would like to use an ultrasound protocol that shows the highest progression with the highest precision (i.e. smallest SE).
To study the effect of the intervention on CIMT change, differences in CIMT progression and their standard errors were estimated with regression models in which CIMT progression over time was the dependent variable and treatment (atorvastatin with torcetrapib versus atorvastatin alone) was the independent variable. Next an absolute treatment/precision (TP) ratio was calculated by dividing the regression coefficient (represents change in CIMT progression due to treatment with torcetrapib) by its corresponding standard error and transforming this into an absolute value. Next the ultrasound protocols were ranked by this absolute TP ratio from low to high, as ideally one would like to use an ultrasound protocol that shows the highest effect of treatment on CIMT progression (largest regression coefficient) with the highest precision (i.e. smallest SE).
Finally the protocols were ranked by all three parameters for the mean common CIMT protocols, the mean maximum CIMT protocols, and all 60 protocols. A summary score was calculated for each protocol, based on summation of the overall ranks of reproducibility, progression/precision ratio and treatment/precision ratio after categorization of these scores in groups of five and six. Groups of five (for the 20 mean common CIMT protocols and 40 mean maximum CIMT protocols) and six (for the total ranking: 60 protocols) were used instead of the absolute ranks, as it was assumed that differences between the protocols were not large enough to justify a difference of 60 versus 1 between the best and the worst protocol, whereas a difference of 5 or 6 versus 1 between the best and the worst protocol was acceptable.
For the present study only data of the duplicate scans before randomization and the duplicate scans at the end of 24 months of study were used. Participants that had data for all four visits were included in the analyses (RADIANCE 1: n = 748; RADIANCE 2: n = 521). Analyses were performed by the complete-case analysis principle. Imputation of missing data was not done. SPSS statistical software (version 12.0) was used for the analyses.
Results
The study populations of the RADIANCE 1 and RADIANCE 2 studies differed on several baseline characteristics (). Participants of the RADIANCE 1 study (FH patients) were younger, had higher levels of low density lipoprotein (LDL) cholesterol, lower levels of triglycerides, lower waist circumference values, and lower body mass index than participants of the RADIANCE 2 study (MD patients). There were more male participants and less hypertension in the RADIANCE 1 study compared to the RADIANCE 2 study.
Table II. Base-line characteristics of the RADIANCE 1 and RADIANCE 2 study populations. Values presented as mean (standard deviation) or number (percentage).
The findings in patients with familial hypercholesterolemia
Data on both pre-randomization examinations and both end-study examinations were available for 748 out of 850 participants (88%) for the RADIANCE 1 study.
Reproducibility. ICC ranged from 0.774 to 0.908 overall, from 0.803 to 0.908 in the mean common CIMT protocols, and from 0.774 to 0.902 in the mean maximum CIMT protocols (). The highest values of ICC were generally found for mean maximum CIMT and mean common CIMT protocols that included measurements at both walls at multiple angles (≥3 angles). The mean difference in CIMT between the two base-line examinations was close to 0 for almost all ultrasound protocols (). The standard deviation (SD) of the mean difference ranged from 0.0777 to 0.0866 for the mean common CIMT ultrasound protocols and from 0.1215 to 0.2051 for the mean maximum CIMT ultrasound protocols. Mean common CIMT protocols had smaller SD than mean maximum CIMT protocols. Mean common CIMT protocols with measurements of both walls at ≥2 angles had the smallest SD. Mean maximum CIMT protocols with measurements of both walls of all three carotid segments had the smallest SD.
Table III. Reproducibility of CIMT measurements at base-line in the RADIANCE 1 study (n=748), estimated as intra-class correlation coefficients (ICC) and the mean difference in CIMT (mm) between duplicate scans. Protocols were ranked in an order of low to high reproducibility (increasing ICC and decreasing standard deviation of mean difference): the higher the rank, the better the protocol. Ranking ICC for all protocols (reported for CCA the top 4; for MeanMax the top 8, and for all the top 10). Please see for precise information on the angles used in each protocol.
Rate of CIMT progression over time in the atorvastatin group. The rate of CIMT progression in the atorvastatin alone group ranged from −0.00302 to 0.00029 mm/year for the mean common CIMT protocols (). All but one protocol showed negative slopes. The CIMT progression for the mean maximum protocols showed positive and negative directions depending on the angles that were used. The absolute progression/precision ratio (PP ratio) ranged from 0.44 to 3.73 for the mean common CIMT protocols and from 0.06 to 1.50 for the mean maximum CIMT protocols. The highest ratios were obtained with mean common CIMT protocols that included measurements of the near and far wall at multiple angles. In the mean maximum CIMT protocols the highest ratios were found in two-segment protocols that included measurements of the far wall and in three-segment protocols with measurements of the near and far wall.
Table IV. Left side: Annual rate of progression of CIMT (mm), its precision (standard errors), absolute ratio of progression/precision and ranking of the ratio for all 60 ultrasound protocols in the RADIANCE 1 study for the atorvastatin only group (n=364). Right side: Effect of treatment on CIMT rate of progression over time in RADIANCE 1 (n=748). Regression coefficients represent the increase in CIMT per year due to treatment with torcetrapib. Protocols were ranked in an order from low to high: the higher the rank, the better the protocol. Ranking reported for CCA the top 4; for MeanMax the top 8, and for all the top 10. Please see for precise information on the angles used in each protocol.
Effect of treatment effect on CIMT change over time. The effect of torcetrapib as compared to placebo on CIMT progression ranged from 0.00087 to 0.000374 mm/year for the mean common CIMT protocols and from −0.00133 to 0.00400 mm/year for the mean maximum CIMT protocols (). The smallest treatment effects were found in the mean maximum protocols, notably in protocols that included measurements of three segments.
The absolute treatment/precision ratios (TP ratios) ranged from 0.75 to 3.91 for the mean common CIMT protocols and from 0.03 to 2.63 for the mean maximum CIMT protocols. The highest TP ratios were found predominantly in the mean common CIMT protocols. Protocols that included measurements of both walls at multiple angles had higher ratios than protocols that were based on measurements of only the far wall at one angle. When the interest was in mean maximum CIMT protocols, the highest TP ratios were found in two-segment protocols with measurements of the near and far wall.
Overall ranking based on reproducibility, rate of CIMT progression, and effect of treatment on CIMT change over time. Mean common CIMT protocols provided the best balance between high reproducibility, large and precise rates of CIMT progression, and effect of treatment (). The highest mean common CIMT ranking protocol was the one based on measurements from both near and far wall, at angles 120, 150, and 180 of the right carotid artery and angles 180, 210, and 240 of the left carotid artery. Mean common CIMT protocols that measured both walls were ranked higher than single wall protocols. In the mean maximum CIMT protocol, the protocols with highest total rank scores were those that included measurements of the near and far wall. The highest mean maximum CIMT ranking protocol was the one based on measurements from three segments (CCA, BIF, ICA) at near and far wall, at angles 90, 120, and 150 or 120, 150, and 180 of the right carotid artery and angles 180, 210, and 240 or 210, 240, and 270 of the left carotid artery (approach #45, 46, 47, 48). Overall three-segment mean maximum CIMT protocols that included measurements of both walls at multiple angles had the highest total rank scores.
The RADIANCE 2 study findings
Data on both pre-randomization examinations and end-study examinations were available for 521 out of 752 participants (69%) in the RADIANCE 2 study.
Reproducibility. ICC ranged from 0.678 to 0.847 for the mean common CIMT protocols and from 0.684 to 0.861 for the mean maximum CIMT protocols (). The highest values of ICC were found for mean common CIMT protocols that included measurements at multiple angles (≥2 angles) and for mean maximum CIMT protocols that included measurements of both the near and the far wall at ≥2 angles. The mean difference in CIMT between the two base-line examinations was close to 0 for almost all ultrasound protocols (). The standard deviation (SD) of the mean difference ranged from 0.0974 to 0.1572 for the mean common CIMT ultrasound protocols and from 0.1584 to 0.2561 for the mean maximum CIMT ultrasound protocols. Mean common CIMT protocols had smaller SD than mean maximum CIMT protocols. Mean common CIMT protocols with measurements of both walls at ≥2 angles had the smallest SD. Of the mean maximum CIMT protocols, three-segment protocols using measurements of both walls at multiple angles were ranked highest.
Table V. Reproducibility of CIMT measurements at base-line in the RADIANCE 2 study (n=521), estimated as intra-class correlation coefficients (ICC) and the mean difference in CIMT (mm) between duplicate scans and ranking for all protocols. Protocols were ranked in an order of low to high reproducibility (increasing ICC and decreasing standard deviation of mean difference): the higher the rank, the better the protocol. Ranking ICC for all protocols reported for CCA the top 4; for MeanMax the top 8 and for all the top 10. Please see for precise information on the angles used in each protocol.
Rate of CIMT progression over time in the atorvastatin group. The rate of progression of mean common CIMT protocols ranged from 0.00084 to 0.00539 mm/year and of mean maximum CIMT protocols from 0.00398 to 0.01057 mm/year. The progression/precision ratio (PP ratio) ranged from 0.84 to 5.61 for the mean common CIMT protocols and from 1.85 to 5.44 for the mean maximum CIMT protocols (). Overall mean common CIMT protocols that included measurements of both walls were ranked highest. Mean maximum CIMT protocols that included measurements at all three segments of both walls at multiple angles showed the highest ratios between rate of CIMT progression over time and its corresponding precision.
Table VI. Left side: Annual rate of progression of CIMT (mm), its precision (standard errors), absolute ratio of progression/precision and ranking of the ratio for all 60 ultrasound protocols in the RADIANCE 2 study for the atorvastatin only group (n = 268). Right side: Effect of treatment on CIMT rate of progression over time in RADIANCE 2 (n = 521). Regression coefficients represent the increase in CIMT per year due to treatment with torcetrapib. Protocols were ranked in an order from low to high: the higher the rank, the better the protocol. Please see for precise information on the angles used in each protocol. Ranking for all protocols (for CCA top 4; for MeanMax top 8 and for all the top 10).
Treatment effect on CIMT change over time. The effect of torcetrapib as compared to placebo on CIMT progression ranged from −0.00101 to 0.00400 mm/year for the mean common CIMT protocols and from −0.00231 to 0.00486 mm/year for the mean maximum CIMT protocols (). The absolute treatment/precision ratios (TP ratios) ranged from 0.01 to 2.16 for the mean common CIMT protocols and from 0.02 to 1.46 for the mean maximum CIMT protocols. The highest TP ratios were found mainly in the mean common CIMT protocols that used measurements of both walls. Mean maximum protocols that included measurements of only the common carotid and the bifurcation segment showed higher TP ratios than three-segment protocols. Protocols with measurements of the near and far wall had higher ratios in both the mean common and the mean maximum protocols.
Overall ranking based on reproducibility, rate of CIMT progression, and effect of treatment on CIMT change over time. Mean common CIMT protocols provided the best balance between high reproducibility, large and precise rates of CIMT progression, and effect of treatment (). The highest mean common CIMT ranking protocol was the one based on measurements from both near and far wall, at angles 90, 120, and 150 of the right carotid artery and angles 210, 240, and 270 of the left carotid artery (approach #8). Mean common CIMT protocols that measured both walls had higher total rank scores than single-wall protocols. In the mean maximum CIMT protocols, the highest total rank scores were found in protocols that used measurements of the near and far wall. The highest mean maximum CIMT ranking protocol was the one based on measurements from both near and far wall, at angles 120, 150, and 180 of the right carotid artery and angles 180, 210, and 240 of the left carotid artery (approach #49). Mean maximum CIMT protocols that included measurements of all three segments at multiple angles had the highest total rank scores.
Table VII. Overall ranking of the ultrasound protocols based on summation of the transformed rank scores (mean common CIMT and mean maximum CIMT into quintile scores; overall rank scores into sixtile scores) for the RADIANCE 1 and RADIANCE 2 study. Ranking for all protocols (for CCA top 4; for MeanMax top 8, and for all the top 10).
Discussion
Mean common CIMT that was assessed through measurements of both the near and far wall of the common carotid artery segment at multiple (≥2) angles provided the best balance between high reproducibility, large estimates of CIMT progression over time, large change in progression over time induced by the intervention, and its associated precision. With regard to mean maximum CIMT, protocols that included measurements of both near and far wall of all three carotid segments performed best.
Some aspects of this study need to be addressed. Firstly, all CIMT measurements in our study were fixed as regards angle through use of Meijer's carotid arc. This guaranteed that consecutive scans could be performed at approximately the same angle. Our results, however, might differ from CIMT ultrasound protocols that are dedicated to finding the previous image (insight/memory) or those that interrogate the maximum measurements (independent of angles), or interrogate from a single angle that visually measures the best image from which CIMT should be measured. However, there are no data available to indicate how protocols with absence of angle approaches would rank in our tables. In the RADIANCE studies, CIMT measurements were performed independent of whether or not a plaque or a lesion was present. In that sense our approach differed from that of the Mannheim consensus (CIMT measurement in an area free of plaque) (Citation33), yet resembles the approach taken in many other studies on the risk of events and other intervention studies. Also, in our studies the same ultrasound equipment was used in all centers. Having different ultrasound equipment in a randomized trial, one would expect that the variability in the measurements goes up to some extent.
Secondly, reproducibility was assessed by the ICC and the standard deviation of the mean difference. The ICC is a commonly used and well known measure to evaluate reproducibility. It quantifies measurement reliability by comparing the variability of different measurements of the same subject to the total variation across all measurements and all subjects. One characteristic of the ICC is that it depends on the magnitude of the variation between individuals. If the variation between individuals is large, relative to measurement error, the ICC will be high. In contrast, if the variation between individuals is small and CIMT is measured with the same measurement error, the ICC will be small. Multiple-segment protocols could therefore produce higher ICCs than single-segments protocols, based on this difference in between-individuals variation. Therefore, protocols were also ranked according to the standard deviation of the mean difference of the duplicate scan. This measure is a suitable test to assess reproducibility and is less affected by between-individuals variations. In the assessment of reproducibility the mean absolute difference (MAD) of the duplicate base-line scan was also evaluated (results not shown). Ranking of the protocols on the absolute mean difference provided similar results as the ranking based on SD of the mean difference. The correlation between these two parameters was close to 1, indicating that these two parameters assess the same outcome.
Thirdly, protocols were ranked based on the absolute progression/precision ratio in the atorvastatin monotherapy group. Most ideally, one would like to rank protocols on progression/precision in a placebo-group as it is then clear in which direction the CIMT progression rate is assumed to go: progression of CIMT rates over time. However in the group that received atorvastatin, the direction was not known. As previous studies showed that statin treatment produces at most a slowing down of the CIMT progression rate that is close to zero (Citation34,Citation35), the absolute PP ratio was used when ranking on magnitude of progression rate (either in a negative direction or in a positive direction) and precision. Yet, in our study negative progression rates in both the mean common and the mean maximum CIMT protocols were observed. We also ranked the protocols based on direction of CIMT progression, i.e. ranking protocols with negative progression rates and high precision more highly (results not shown); however, this only had a minor effect on the ranking. Finally, we observed the same difficulty of direction of progression in the ranking of treatment effect on progression of CIMT. Although the event trial with atorvastatin and torcetrapib showed increased risk in the torcetrapib arm as compared to atorvastatin monotherapy (Citation36), we decided to rank the ultrasound protocols as if treatment with torcetrapib was to slow down CIMT progression. This was done for two reasons: 1) CIMT trials are designed to show benefit of treatment, and if treatment is expected to cause harm a CIMT trial would not be conducted beforehand; and 2) the event trial showed that torcetrapib therapy resulted in an increased risk of mortality and morbidity of an unknown mechanism, with evidence of an off-target effect of torcetrapib (Citation37). Currently trials with other CETP inhibitors are being conducted, and these will provide information whether this class of drugs yields an effect on CIMT progression. To overcome this difficult problem, we ranked based on the absolute TP ratio, which corresponds only to magnitude of effect with precision, whilst discarding the direction of effect of treatment (positive or negative).
The generalizability of the results of this study may depend on the study populations since reproducibility, progression and its precision, and effect of treatment and its precision may be affected by the level of atherosclerosis. However, the implications on choice of ultrasound protocol seem to be equal for both study populations. For the FH populations the best balance between the three parameters was found in mean common CIMT protocols, with increasing ratios if both walls were measured at more angles. This also applies to the MD populations; yet in the MD population, some mean maximum CIMT protocols also rank favorably.
For decades a lively discussion has been on-going regarding the desirability of performing near-wall CIMT measurements (Citation38). The reluctance is based on the physics of ultrasound indicating that the near-wall CIMT is at best an approximation of the true value, whereas the advocates indicate that the addition of the near-wall measurements increase precision and hence increase precision in risk prediction and evaluation of drug effects. Our study indicated that the best protocols with regard to reproducibility, PP ratio, and TP ratio were all predominantly based on data collected from both the far and the near wall. The results of our study support the view that ultrasound protocols that measure both walls should be preferred above protocols that measure only the far wall.
In our study we used an automated edge detection program. These approaches have been suggested as a very useful approach to reduce considerably variability in the measurement of CIMT. Most of these automated edge detection programs have been applied for reading of the far wall of the common carotid artery, whereas the near wall is not considered, nor are measurements at the bifurcation and in the internal segments. The main potential advantage of automated edge detection programs is that they may reduce variability in CIMT readings as a result of reduction in the differences between readers, and by the elimination of change in reading behavior over time (reader drift). However, the beneficial effect of automated edge detection in reduction of measurement variability depends on the contribution of sonographers and readers on the total variability in the CIMT measurement. A number of studies have indicated that differences between sonographers have a much larger effect on the CIMT measurements than differences between readers (Citation39,Citation40). Furthermore, a formal quantification of the extent of reduction in measurement error using either approach has not been done. In general, when ultrasound images show clear interfaces automated edge detection programs work very well, whereas when the interfaces on the ultrasound images are less clear the automated edge detection program needs to be manually overridden, thereby eliminating the advantages of the use of automated edge detection.
In every study using CIMT measurements, whether a cohort study or a randomized controlled trial, a choice needs to be made based on the costs and the benefits. Benefits relate to high reproducibility, precise measurements, and when appropriate a high progression/precision balance, and thus a high likelihood of success. Costs relate to the time needed to acquire the CIMT information (ultrasound scanning and reading) and the financial expenses related to that process. Acquisition times may vary from 15 minutes for protocols that assess CIMT in one segment and one angle (e.g. protocols #1–4 or #11–14) to 45 minutes for protocols that assess CIMT in all three segments and at multiple angles (e.g. protocols #45–50). Similarly, off-line reading time may vary from 15 minutes for the single-segment, one-angle protocols to 1.5 to 2 hours for the multi-segment, multi-angle protocols. The balance between quality and costs should be evaluated and considered in the decision-making process. We feel that the present analyses provide sufficient information to estimate that balance in an evidence-based way.
To the best of our knowledge published data of this type are limited, most likely since no other study has such a wealth of detailed information on CIMT measurements as was available in the RADIANCE 1 and RADIANCE 2 studies. Data from other studies with similar extensive ultrasound protocols were analyzed and provided information on the best ultrasound protocol for trials in other population groups. In healthy middle-aged subjects, in the OPAL study (Citation27), mean common CIMT ultrasound protocols that included measurements of both the near and far wall at multiple angles (Citation24) performed best on reproducibility and providing a large rate of CIMT progression with a high precision.
In conclusion, our findings support the opinion that the number and specific combination of segments, angles, and walls interrogated are associated with differences in reproducibility, magnitude, and precision of progression of CIMT over time. Given these findings, the choice for an ultrasound protocol should depend on a well considered balance of these parameters before the study is carried out.
Trial registration
RADIANCE 1 ClinicalTrials.gov number: NCT00 136981; RADIANCE 2 ClinicalTrials.gov number: NCT00134264.
Appendix 1
Download PDF (173.2 KB)Acknowledgements
The authors thank Rudy Meijer in Schoorl, the Netherlands, for the design of the image-acquisition protocol, training, and quality control; and P. Barter, T. Roberts, D. Ambrose, A. Chin, W. Davidson, R. Burnside, A. Caffrey, M. Li, A. O'Reilly, Tu T. Nguyen, and T. Thuren. We thank the following staff at CIMT Laboratory Europe: C. van Everdingen, A. Geerts, M. Geurtsen, M. Djuanda, A. Kuin, F. Leus, R. Meijer, D. Mooiweer-Bogaerdt, K. Nijssen, H. Noordzij, L. Romkes, B. Sies, E. Stooker, F. Verhey, B. van der Vlist, L. van der Vlist, E. Wineke, and H. Wisse; and at the CIMT Core Laboratory United States: M. Barr, K. Bettermann, S. Burton, A. Conner-Day, B. Ettenger, J. Griffin, C. Halverson, B. Holley, L. Hoots, J. Fleshman, M. Lauffer, L. Passmore, C. Sharpe, M. Wilder, P. Miller, T. Vitek, and G. Wolgast.
Declaration of interest: Dr Dogan and Dr Duivenvoorden report no conflict of interest. Dr Kastelein reports receiving consulting fees and lecture fees from Pfizer, Astra-Zeneca, Merck, and Schering-Plough and grant support from Pfizer and Astra-Zeneca. Dr Shear was a former employee of Pfizer. Dr Grobbee reports receiving consulting fees, lecture fees, and grant support from Pfizer, Astra-Zeneca, Servier, Organon, Merck, and Unilever. Dr Evans reports receiving honoraria, consulting fees, and grant support for professional input on CIMT issues from Astra-Zeneca, Organon, and Pfizer. Dr Visseren reports receiving research grants from Merck and the Netherlands Organisation for Health Research and Development. Dr Bots reports receiving consulting fees, lecture fees, and grant support from Pfizer, Astra-Zeneca, Servier, Organon, Merck, and Unilever.
No other potential conflict of interest relevant to this article was reported.
References
- Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399–406.
- Prati P, Tosetto A, Vanuzzo D, Bader G, Casaroli M, Canciani L, . Carotid intima media thickness and plaques can predict the occurrence of ischemic cerebrovascular events. Stroke. 2008;39:2470–6.
- Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, Bluemke DA, . Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med. 2008;168:1333–9.
- Rundek T, Arif H, Boden-Albala B, Elkind MS, Paik MC, Sacco RL. Carotid plaque, a subclinical precursor of vascular events: the Northern Manhattan Study. Neurology. 2008;70:1200–7.
- Newman AB, Naydeck BL, Ives DG, Boudreau RM, Sutton-Tyrrell K, O'Leary DH, . Coronary artery calcium, carotid artery wall thickness, and cardiovascular disease outcomes in adults 70 to 99 years old. Am J Cardiol. 2008; 101:186–92.
- Li C, Engström G, Berglund G, Janzon L, Hedblad B. Incidence of ischemic stroke in relation to asymptomatic carotid artery atherosclerosis in subjects with normal blood pressure. A prospective cohort study. Cerebrovasc Dis. 2008; 263):297–303.
- Johnsen SH, Mathiesen EB, Joakimsen O, Stensland E, Wilsgaard T, Løchen ML, . Carotid atherosclerosis is a stronger predictor of myocardial infarction in women than in men: a 6-year follow-up study of 6226 persons: the Tromsø Study. Stroke. 2007;38:2873–80.
- Price JF, Tzoulaki I, Lee AJ, Fowkes FG. Ankle brachial index and intima media thickness predict cardiovascular events similarly and increased prediction when combined. J Clin Epidemiol. 2007;60:1067–75.
- Cao JJ, Arnold AM, Manolio TA, Polak JF, Psaty BM, Hirsch CH, . Association of carotid artery intima-media thickness, plaques, and C-reactive protein with future cardiovascular disease and all-cause mortality: the Cardiovascular Health Study. Circulation. 2007;116:32–8.
- Baldassarre D, Amato M, Pustina L, Castelnuovo S, Sanvito S, Gerosa L, . Measurement of carotid artery intima-media thickness in dyslipidemic patients increases the power of traditional risk factors to predict cardiovascular events. Atherosclerosis. 2007;191:403–8.
- Ali YS, Rembold KE, Weaver B, Wills MB, Tatar S, Ayers CR, . Prediction of major adverse cardiovascular events by age-normalized carotid intimal medial thickness. Atherosclerosis. 2006;187:186–90.
- Lorenz MW, von Kegler S, Steinmetz H, Markus HS, Sitzer M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS). Stroke. 2006;37:87–92.
- Murakami S, Otsuka K, Hotta N, Yamanaka G, Kubo Y, Matsuoka O, . Common carotid intima-media thickness is predictive of all-cause and cardiovascular mortality in elderly community-dwelling people: Longitudinal Investigation for the Longevity and Aging in Hokkaido County (LILAC) study. Biomed Pharmacother. 2005;59 Suppl 1:S49–53.
- Rosvall M, Janzon L, Berglund G, Engström G, Hedblad B. Incident coronary events and case fatality in relation to common carotid intima-media thickness. J Intern Med. 2005; 257:430–7.
- Kitamura A, Iso H, Imano H, Ohira T, Okada T, Sato S, . Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke. 2004;35:2788–94.
- Störk S, van den Beld AW, von Schacky C, Angermann CE, Lamberts SW, Grobbee DE, . Carotid artery plaque burden, stiffness, and mortality risk in elderly men: a prospective, population-based cohort study. Circulation. 2004; 110:344–8.
- Chambless LE, Heiss G, Shahar E, Earp MJ, Toole J. Prediction of ischemic stroke risk in the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2004;160:259–69.
- Chambless LE, Folsom AR, Sharrett AR, Sorlie P, Couper D, Szklo M, . Coronary heart disease risk prediction in the Atherosclerosis Risk in Communities (ARIC) study. J Clin Epidemiol. 2003;56:880–90.
- Iglesias del Sol A, Bots ML, Grobbee DE, Hofman A, Witteman JC. Carotid intima-media thickness at different sites: relation to incident myocardial infarction; The Rotterdam Study. Eur Heart J. 2002;23:934–40.
- Belcaro G, Nicolaides AN, Ramaswami G, Cesarone MR, De Sanctis M, Incandela L, . Carotid and femoral ultrasound morphology screening and cardiovascular events in low risk subjects: a 10-year follow-up study (the CAFES-CAVE study(1)). Atherosclerosis. 2001;156:379–87.
- Parrinello G, Barbagallo CM, Pinto A, Amato P, Cecala MG, Noto D, . Carotid atherosclerosis in hypercholesterolemic patients: relationship with cardiovascular events. Nutr Metab Cardiovasc Dis. 2001;11:96–103.
- O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22.
- Salonen JT, Salonen R. Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb. 1991;11:1245–9.
- Revkin JH, Shear CL, Pouleur HG, Ryder SW, Orloff DG. Biomarkers in the prevention and treatment of atherosclerosis: need, validation, and future. Pharmacol Rev. 2007; 59:40–53.
- Wang JG, Staessen JA, Li Y, Van Bortel LM, Nawrot T, Fagard R, . Carotid intima-media thickness and antihypertensive treatment: a meta-analysis of randomized controlled trials. Stroke. 2006;37:1933–40
- Yokoyama H, Katakami N, Yamasaki Y. Recent advances of intervention to inhibit progression of carotid intima-media thickness in patients with type 2 diabetes mellitus. Stroke. 2006;37:2420–7.
- Dogan S, Plantinga Y, Evans GW, Meijer R, Grobbee DE, Bots ML; OPAL investigators. Ultrasound protocols to measure carotid intima-media thickness: a post-hoc analysis of the OPAL study. Curr Med Res Opin. 2009;25:109–22.
- Kastelein JJ, van Leuven SI, Burgess L, Evans GW, Kuivenhoven JA, Barter PJ, . Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N Engl J Med. 2007;356:1620–30.
- Kastelein JJ, van Leuven SI, Evans GW, Riley WA, Revkin JH, Shear CL, . Designs of RADIANCE 1 and 2: carotid ultrasound studies comparing the effects of torcetrapib/atorvastatin with atorvastatin alone on atherosclerosis. Curr Med Res Opin. 2007;23:885–94.
- Bots ML, Visseren FL, Evans GW, Riley WA, Revkin JH, Tegeler CH, . Torcetrapib and carotid intima-media thickness in mixed dyslipidaemia (RADIANCE 2 study): a randomised, double-blind trial. Lancet. 2007;370:153–60.
- Liang Q, Wendelhag I, Wikstrand J, Gustavsson T. A multiscale dynamic programming procedure for boundary detection in ultrasonic artery images. IEEE Trans Med Imaging. 2000;19:127–42.
- Duivenvoorden R, Nederveen AJ, de Groot E, Kastelein JJ. Atherosclerosis imaging as a benchmark in the development of novel cardiovasular drugs. Curr Opin Lipidol. 2007;18:613–21.
- Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, . Mannheim carotid intima-media thickness consensus (2004–2006). An update on behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis. 2007;23:75–80.
- Crouse JR III, Raichlen JS, Riley WA, Evans GW, Palmer MK, O'Leary DH, . Effect of rosuvastatin on progression of carotid intima-media thickness in low-risk individuals with subclinical atherosclerosis: the METEOR Trial. JAMA. 2007;297:1344–53.
- Salonen R, Nyyssonen K, Porkkala E, Rummukainen J, Belder R, Park JS, . Kuopio Atherosclerosis Prevention Study (KAPS). A population-based primary preventive trial of the effect of LDL lowering on atherosclerotic progression in carotid and femoral arteries. Circulation. 1995;92:1758–64.
- Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, . Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357: 2109–22.
- Vergeer M, Bots ML, van Leuven SI, Basart DC, Sijbrands EJ, Evans GW, . Cholesteryl ester transfer protein inhibitor torcetrapib and off-target toxicity. A pooled analysis of the Rating Atherosclerotic Disease Change by Imaging With a New CETP Inhibitor (RADIANCE) trials. Circulation. 2008;118:2515–22.
- Wikstrand J. Methodological considerations of ultrasound measurement of carotid artery intima-media thickness and lumen diameter. Clin Physiol Funct Imaging. 2007;27:341–5.
- Tang R, Hennig M, Thomasson B, Scherz R, Ravinetto R, Catalini R, . Baseline reproducibility of B-mode ultrasonic measurement of carotid artery intima-media thickness: the European Lacidipine Study on Atherosclerosis (ELSA). J Hypertens. 2000;18:197–201.
- Hulthe J, Wikstrand J, Emanuelsson H, Wiklund O, de Feyter PJ, Wendelhag I. Atherosclerotic changes in the carotid artery bulb as measured by B-mode ultrasound are associated with the extent of coronary atherosclerosis. Stroke. 1997;28:1189–94.