Abstract
Background. Low serum total cholesterol is frequently associated with worse survival in older people, but mechanisms of this association are poorly understood.
Aims. Characteristics of cholesterol metabolism were related to survival in a random 75 + population sample.
Methods. Serum cholesterol and lathosterol, and sitosterol were measured in random persons (n = 623) of birth cohorts (1904, 1909, and 1914) in 1990, and all persons were followed for 17 years.
Results. Total cholesterol declined in old age, and low cholesterol was associated with poor health and multi-morbidity. Cholesterol below 5.0 mmol/L was associated with accelerated all-cause mortality (age- and gender-adjusted hazard ratio (HR) 1.54; 95% CI 1.21–1.97; P < 0.001) and vascular mortality (HR 2.13 (1.42–3.07); P < 0.001). Lathosterol (indicating cholesterol synthesis) and sitosterol (indicating cholesterol absorption) also decreased with deteriorating health. Low lathosterol, sitosterol, and cholesterol predicted mortality additively and independently of each other. When all three sterols were high (> median) or low, the age- and gender-adjusted survival was 9.9 and 5.6 years (P < 0.001).
Conclusion. Lower synthesis and absorption of cholesterol, and low serum cholesterol level are associated with deteriorating health and indicate impaired survival in old age.
| Abbreviations | ||
| ApoE | = | apolipoprotein E |
| BMI | = | body mass index |
| BP | = | blood pressure |
| CAD | = | coronary heart disease |
| CDR | = | Clinical Dementia Rating |
| CI | = | confidence interval |
| CRP | = | C-reactive protein |
| DHEAS | = | dehydroepiandrosterone sulfate |
| eGFR | = | estimated glomerular filtration rate |
| HDL-C | = | high-density lipoprotein cholesterol |
| LDL-C | = | low-density lipoprotein cholesterol |
| MMSE | = | Mini-Mental State Examination |
| PEF | = | peak expiratory flow |
| PTH | = | parathyroid hormone |
| TC | = | total cholesterol |
| TG | = | triglycerides |
Key messages
Old age, multi-morbidity, cognitive decline, impaired functioning, and need of help are associated with low serum cholesterol, lowered cholesterol synthesis, and to a lesser extent with diminished cholesterol absorption.
Characteristics of attenuated cholesterologenesis are risk indicators in old age.
Introduction
Compared to middle-aged populations, associations of serum total cholesterol (TC) with coronary artery disease (CAD) and mortality have been less consistent in older people. Pooled data from early studies showed that TC was positively correlated with fatal CAD in both men and women and also in older people (age 65–100 years) with decreasing relative but increasing attributable risk (Citation1).
Some later studies have confirmed the prognostic role of elevated TC in older CAD patients (Citation2–8), whilst the relationship between TC and all-cause mortality has not been observed among older persons in several other studies (Citation8–11).
In 1990, the association between low TC and mortality risk was analyzed in 19 studies (Citation12). The U-shaped relationship in men and the flat relation in women for total mortality resulted largely from a positive relation between TC and fatal CAD, and an inverse relation between TC and non-vascular deaths. A U-shaped or J-shaped relationship has also been observed in some later studies (Citation12–16).
Studies focusing on older people have revealed an inverse association between TC and total mortality in the US (Citation13,Citation17,Citation18), European countries (Citation19–22), and Japan (Citation23). This also held true for Medicare recipients followed for 10 years (Citation24,Citation25). Because these results have relevance for cardiovascular prevention among older adults, many investigators have emphasized the need for studies of underlying mechanisms. In epidemiological studies, details of cholesterol metabolism can be studied by measuring serum non-cholesterol sterols, which provide information about cholesterologenesis (Citation26,Citation27). The ratio of cholesterol precursors (e.g. lathosterol) to cholesterol indicates the activity of cholesterol synthesis, and that of plant sterols (e.g. sitosterol) reflects the rate of intestinal cholesterol absorption (Citation28,Citation29).
In the Helsinki Aging Study, a prospective birth cohort study, low total TC appeared to associate with poor health and increased mortality in the 1-year follow-up (Citation30). Now, when almost all participants have died, we report the cholesterol metabolism and clinical characteristics at base-line and their relationships with 17-year prognosis in late life. The purposes of this report is to assess 1) the associations of total cholesterol, lathosterol, and sitosterol with age, cognition, multi-morbidity, and need of care; 2) to reassess these associations 5 years later; and 3) to evaluate the prognostic significance of total cholesterol, lathosterol, and sitosterol for 17-year mortality.
Materials and methods
Base-line examinations
The research protocol for all stages of the Helsinki Aging Study has been approved by the Ethics Committee of the Helsinki University Central Hospital.
The base-line examinations in 1989 have been described in detail earlier (Citation26,Citation27). A random sample of persons born in 1904 (n = 300), 1909 (n = 300), and 1914 (n = 300) was selected from the census register in Helsinki, Finland. The participants alive at entry (n = 795) were mailed a questionnaire including several items about illnesses, medications, functioning, mood, and attitudes towards life. A total of 144 persons refused to answer. At entry, participants (n = 651) were examined clinically by a nurse, general practitioner, neurologist, and cardiologist, and the patient records were collected. In addition to routine anthropometric and cardiovascular measurements (such as pulse rate, blood pressure, and body mass index (BMI)), the clinical examination also included the measurement of the peak expiratory flow (PEF). After collection of all questionnaire and clinical data, the functional status was determined. The examining physician also estimated the global health status using a visual analog scale, and the possible need of further examinations and care. The Mini-Mental State Examination (MMSE) (Citation31) and the Clinical Dementia Rating (CDR) (Citation32) were used for assessment of cognition. Impaired cognition at entry was defined as MMSE < 24 points.
Laboratory examinations
Blood samples for routine laboratory analyses (n = 613), including serum lipids (total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG)), were drawn after an overnight fast. Glomerular filtration rate (eGFR) was estimated with the Cockcroft–Gault formula. Apolipoprotein E genotyping (ApoE alleles) was performed from serum samples by immunoelectrophoresis and isoelectric focusing (Citation33). Base-line C-reactive protein (CRP) was measured with a sensitive enzyme immunoassay (sensitivity 0.3 mg/L; Medix Biochemica, Espoo, Finland) from frozen (−20°C) serum. Leptin concentration was determined by radioimmunoassay (Linco Research, St Charles, MO, USA). Dehydroepiandrosterone sulfate (DHEAS) was measured using a commercial kit (Coat-A-Count DHEA-soy, Diagnostic Products Corporation, Los Angeles, CA, USA).
An immunoradiometric method (AllegroR Intact PTH kit, Nichols Institute, San Juan Capistrano, CA, USA) was used to determine serum parathyroid hormone (PTH).
Non-cholesterol sterols (and cholesterol) were measured with gas liquid chromatography (n = 562). These non-cholesterol sterols include cholesterol precursor lathosterol (reflects cholesterol synthesis), and plant sterol (sitosterol) reflecting cholesterol absorption (Citation28,Citation29). Non-cholesterol sterols are expressed as a ratio to serum cholesterol (μg × 102 per mg of cholesterol) to standardize for variations in their transport protein concentrations.
Follow-up
The participants were re-examined in 1991, 1993 (clinical examination including echocardiography), 1995 (home visits + laboratory), and in 1999 (home visits). The date of death has been collected from the National Population Register up to 31 July 2007. The survival data are 100% complete. The death certificates (n = 346) were collected, and the causes of death were within the first 9 years.
Statistics
All variables were examined for outliers, missing data, and entry errors. Differences in proportions were tested with a chi-square test, and continuous measurements with an analysis of variance. The Kaplan–Meier curves and the Cox survival analyses were used for testing the risks of mortality. Age and gender were used as standard covariates. Other confounders were retained in the model based upon their established association with serum cholesterol levels and mortality rate. The continuous measurements were summarized as means ± SD or 95% confidence intervals (CI) of means. P < 0.05 was considered statistically significant in the univariate analyses.
Results
Serum levels at age of 75, 80, and 85 years; base-line characteristics
The characteristic differences of random persons of three birth cohorts included gender distribution, health indicators, and levels of cardiovascular risk factors (). The number of diseases increased, cognition declined, and need of help increased, but diastolic blood pressure (BP) and BMI decreased with advancing age. There were few smokers among the oldest people.
Table I. Selected base-line characteristics of study population by age.
Determinants of serum cholesterol
The mean base-line TC of the participants (6.31 mmol/L) was higher in women than men in each age group and tended to decrease by advancing age (). Similar differences were also found for HDL-C in women, whereas TG tended to increase with advancing age. The subjects with a history of CAD had lower HDL-C (1.32 mmol/L versus 1.52 mmol/L; P < 0.001), whereas TC (6.35 mmol/L versus 6.30; P = 0.234) and TG (1.54 mmol/L versus 1.40 mmol/L) did not differ significantly.
Table II. Base-line serum total cholesterol, HDL-cholesterol, and triglycerides (mmol/L) (SE) by demography, cognition, need of care, and multi-morbidity.
Variables significantly associated with TC were cognition (CDR class), need of care, and multi-morbidity. TC correlated with MMSE score (r = 0.139; P < 0.01) and global health estimated by the physician (visual analogue scale 0 = poor, 10 excellent; r = 0.184; P < 0.001). Consequently, the results suggested an association between higher TC and better health, cognition, and functioning. This was also illustrated by significant albeit weak correlations between TC and hemoglobin (r = 0.221; P < 0.001), serum albumin (r = 0.091; P = 0.023), serum protein (r = 0.135; P < 0.001), and C-reactive protein (r = −0.093; P = 0.05). TC was also associated with both systolic (r = 0.102; P = 0.05) and diastolic blood pressure (r = 0.120; P = 0.04), but was independent of apolipoprotein E phenotype and BMI (r = 0.043).
Non-cholesterol sterols
Base-line serum sitosterol ratios decreased by age, but this decline was less obvious in serum lathosterol (). Both the lathosterol and sitosterol ratios were low in older persons suffering from poor health, having impaired cognition, and requiring daily care. The lowest values were common in institutionalized patients. Lathosterol was high, but sitosterol was low in subjects with high BMI.
Table III. Mean values of serum lathosterol and sitosterol (μg × 102 × mg of cholesterol, mean (SE)) by gender, age, body mass index, diabetes, cognition, and need of care.
Multi-morbidity (number of diseases) associated closely with low plant sterols but less with lathosterol. Older persons with low lathosterol-to-cholesterol ratios were also characterized by low leptin, low DHEAS, low PEF, lower systolic blood pressure, decreased eGFR, but elevated PTH and CRP (data not shown).
Re-examination at 5 years
None of the participants used statins at base-line or at 5 years, but TC decreased significantly (0.2 mmol/year) during 5 years. This decrease was similar among men and women and in all three birth cohorts. Despite the higher mortality of sick persons with TC and attrition of the study population, significant associations were found between total cholesterol and health status. Again, TC significantly correlated with serum albumin (age- and gender-adjusted r = 0.343; P < 0.001), protein (r = 0.225; P < 0.001), and creatinine (r = 0.236; P = 0.014), and with base-line cholesterol (r = 0.689; P < 0.001). Five-year changes in total cholesterol correlated significantly with those of serum albumin (r = 0.421; P < 0.001), protein (r = 0.375; P < 0.001), and creatinine (r = 0.181; P < 0.01), and with cognitive decline (not shown).
Follow-up; serum cholesterol, lathosterol, and sitosterol as survival predictor; all-cause mortality
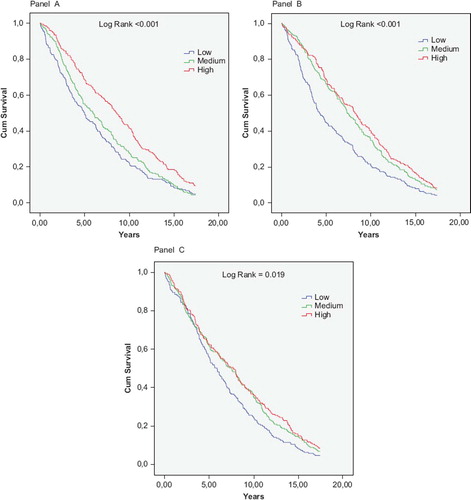
During the 17-year follow-up, 94% of the study participants died. The unadjusted Kaplan–Meier survival curves by tertiles of TC diverged for over 5 years (, Panel A).
Figure 1. Kaplan–Meier curves for 17-year cumulative survival by tertiles of serum total cholesterol (Panel A), lathosterol/cholesterol ratios (Panel B), and sitosterol/cholesterol ratios (Panel C).
Using an arbitrary cut-point (4.99 mmol/L), the median survival of lower and higher TC group was 5.3 and 7.7 years, respectively. The age- and gender-adjusted HR of lower TC was 1.54 (P < 0.001) and remained significant (HR 1.37; P = 0.020) after further controlling for smoking, hypertension, body mass index, history of myocardial infarction, MMSE score, and need of care (). The significance was lost when adjusted for global health and three frailty indicators.
Table IV. Lower cholesterol (< 5 mmol/L), lathosterol/cholesterol (< median), and sitosterol/cholesterol (< median) as predictors of all-cause and vascular mortality.
Excess mortality of participants with low TC tended to be consistent in both genders and each age group, except the youngest women (born in 1914) ().
Figure 2. Low serum total cholesterol (< 5 mmol/L (Panel A)) and low (< median) lathosterol and sitosterol through cholesterol ratios (Panel B) as risk indicators (HR and 95% CI) of all-cause mortality by age and gender. Number of subjects (events/total) in parentheses.
When the participants (n = 572) were grouped according to the median values of serum non-cholesterol sterol/cholesterol ratio, both lower lathosterol (lower synthesis) and sitosterol (lower absorption) associated with mortality risk (, Panels B and C). shows that the predictive value of low lathosterol remained significant and almost unchanged after correction for conventional cardiovascular risk factors, actual health indicators, BMI, cognition, and need of care, which were all powerful mortality predictors in this study population. After multiple adjustments the predictive value of lower sitosterol was insignificant. Because lathosterol and sitosterol were inversely related (r = −0.248; P < 0.001), and reflect reciprocal mechanisms of cholesterologenesis, they were controlled for each other (, Model D). In such analyses, both low synthesis and low absorption rate of cholesterol were significant predictors of all-cause mortality, lathosterol emerging as the most significant indicator.
When the 5-year survivors were followed for 12 years, lower TC (< 5 mmol/L) was associated with excess mortality (age- and gender-adjusted HR 1.67; 95% CI 1.28–2.16); P < 0.001).
Mean base-line TC of the few 17-year survivors (n = 38) was 6.8 (SD 1.7) mmol/L, whereas that of non-survivors was 6.3 (1.2) mmol/L (P = 0.017). The respective means of 5-year values were 6.0 mmol/L and 5.5 mmol/L (P = 0.026).
Vascular mortality
The death certificates were collected for the first 9 years of follow-up. Of the 9-year deaths (n = 346) 180 (57%) were caused by vascular diseases. Low TC (age- and gender-adjusted HR = 2.13; P < 0.001) and lathosterol (HR 1.55) emerged as significant risk indicators (). The predictive values remained virtually unchanged after wide adjustments, whereas the figures for sitosterol were inconsistent.
Among vascular deaths 97 acute myocardial infarctions were classified as immediate cause of death. Neither TC nor non-cholesterol sterols had predictive significance in this subgroup.
Comparison of predictive values
When TC, lathosterol, and sitosterol-to-cholesterol ratios were tested simultaneously as survival covariates, all three parameters (either as continuous or categorized variables) were significant and independent predictors of all-cause mortality (, Model D).
Furthermore, the associations of low serum TC, lathosterol, and sitosterol with mortality risk were graded and additive. When all three sterols were high (> median) or low (< median), the age- and gender-adjusted survival was 9.9 and 5.6 years, respectively (P < 0.001) ().
Discussion
The novel contribution of our study is to demonstrate the interplay between cholesterol synthesis, cholesterol absorption, and serum TC as survival predictors.
The results show that old age is characterized by both decreasing cholesterol synthesis and decreasing cholesterol absorption, and—as a logical consequence—lowered serum TC levels. All these features were associated with deteriorating health, multi-morbidity, frailty, and particularly cognitive impairment, all of which indicate mortality risk at the population level.
A random population sample, comprehensive clinical and laboratory examinations, as well as complete and long follow-up are the major strengths of this study. A further strength is that treatment with cholesterol-lowering drugs does not distort analyses and conclusions of cholesterol and aging-related phenomena. A limitation is that the non-cholesterol sterols were measured at base-line only.
By demonstrating a decrease in serum TC in old age, the results are in accordance with numerous earlier studies (Citation34–41). In our population the decrease in both TC and HDL-C was more profound in the longitudinal than cross-sectional settings due to the clear over-mortality of participants with low TC. Several studies have proposed that the age-associated decrease in TC is attributable to subclinical and clinical diseases and that these relationships should be thoroughly investigated (Citation6,Citation12,Citation17,Citation24,Citation40). In our study a large number of health indicators for older people were registered both at both base-line and during re-examinations. Regardless of which health indicators were selected (subjective or objective health, number of diseases, co-morbidity indexes), the results remained essentially similar and uniformly showed the close connection between low TC and poor health. Although high TC did not predict cardiovascular deaths in this random population including sick people, the result do not oppose the role of TC as a risk factor of CAD in old age. In fact, large meta-analyses, including also older persons, have disclosed the positive association between TC and CAD mortality but not with stroke mortality (Citation42,Citation43). However, other serum lipids than total TC appear to be stronger predictors of CAD in older people (Citation44).
Measurement of non-cholesterol sterols sheds new light on the mechanisms of decreasing cholesterol in old age. An indirect measure of cholesterol synthesis (lathosterol) and that of fractional cholesterol absorption rate (sitosterol) tended to decrease by advancing age and were significantly lower in participants with poor health and impaired cognition. In keeping with earlier observations cholesterol synthesis was high and absorption was low in obesity and diabetes (Citation29), and similar associations were also observed with high leptin concentrations. The association of low sitosterol with higher mortality is also in accordance with the results of 22-year follow-up of men (mean age 60 years) (Citation45). In the LURIC study, in which the non-cholesterol sterols were measured in 1,257 persons (mean age 63 years) and the mean follow-up lasted for 7 years, high absorption and low synthesis of cholesterol were significant mortality indicators (Citation46). However, sitosterol did not emerge as a significant predictor.
It is tempting to speculate that low serum cholesterol in old people is mainly caused by diminished cholesterol synthesis, not adequately compensated by increased cholesterol absorption rate. Unfortunately, the third basic parameter of cholesterol metabolism, the fractional removal rate of serum LDL-C, was not measured due to a lack of methods suitable for large-scale population studies. Nevertheless, the significant decrease in serum TC suggests that a possible reduction of cholesterol removal rate would be insufficient to sustain the balance in a situation of both diminishing synthesis and diminishing absorption due to frailty and/or multiple diseases.
Together with earlier data the following generalization seems to be justified: The older and/or less selected the study population, the closer is the connection between low TC and increased mortality risk.
Human aging is characterized by weakening of growth potential and activation of inflammatory processes (Citation47,Citation48). The present study implies that attenuation of cholesterologenesis is also common in later life. In fact, both low cholesterol synthesis and absorption are strongly related to low BMI, low leptin (reduced subcutaneous tissue), low creatinine, low albumin, and low blood pressure. Low cholesterol synthesis was also associated with low albumin, low DHEAS, low PEF, decreased eGFR, but elevated PTH (vitamin D deficiency) and CRP. Together, they indicate poor nutrition, muscle weakness and sarcopenia, inflammation, and organ failure, all hall-marks of the geriatric syndrome called frailty (Citation49). They are also significant mortality predictors in our study participants (Citation27,Citation50–52).
Although serum TC, lathosterol, and sitosterol were independent survival indicators, the low lathosterol-to-cholesterol ratio appeared to be the ultimate driver in these connections. Our data indicate—even prove—that endogenously lowering cholesterol synthesis and absorption are accelerated by frailty and diseases, and reflect diminishing anabolic processes. Conceivably, low TC is mainly a surrogate marker for decreasing cholesterol synthesis and absorption. Weakening of these basic anabolic and life-sustaining mechanisms is a late-life phenomenon.
It is important to realize that the observed associations reflect endogenously lowered cholesterol—not the results of lipid-lowering treatments, which were not used in our cohort. That low TC due to aging, age-associated diseases, and development of frailty is a mortality predictor does not mean that cholesterol-lowering treatment would be harmful. On the contrary, various analyses have demonstrated that statin treatment is associated with improved survival also in older people (Citation43,Citation53–55). Thus, the active and passive cholesterol-lowering have different clinical consequences.
Declaration of interest: The Lions Organization (Red Feather), the Ragnar Ekberg Foundation, and the Helsinki University Central Hospital are gratefully acknowledged for financial support. All authors have had co-operation with companies dealing with various cholesterol-lowering products.
References
- Manolio TA, Pearson TA, Wenger NK, Barrett-Connor E, Payne GH, Harlan WR. Cholesterol and heart disease in older persons and women. Review of an NHLBI workshop. Ann Epidemiol. 1992;2:161–76.
- Benfante R, Reed D. Is elevated serum cholesterol a risk factor for coronary heart disease in the elderly. JAMA. 1990;263:393–6.
- Tervahauta M, Pekkanen J, Nissinen A. Risk factors of coronary heart disease and total mortality among elderly men with and without preexisting coronary heart disease. Finnish cohorts of the Seven Countries Study. J Am Coll Cardiol. 1995;26:1623–9.
- Frost PH, Davis BR, Burlando AJ, Curb JD, Guthrie GP Jr, Isaacsohn JL, . Serum lipids and incidence of coronary heart disease. Findings from the Systolic Hypertension in the Elderly Program (SHEP). Circulation. 1996;94:2381–8.
- Casiglia E, Mazza A, Tikhonoff V, Scarpa R, Schiavon L, Pessina AC. Total cholesterol and mortality in the elderly. J Intern Med. 2003;254:353–62.
- Corti M-C, Guralnik JM, Salive ME, Harris T, Field TS, Wallace RB, . HDL cholesterol predicts coronary heart disease mortality in older persons. JAMA. 1995;274: 539–44.
- Stemmermann GN, Chyou PH, Kagan A, Nomura AM, Yano K. Serum cholesterol and mortality among Japanese-American men. The Honolulu (Hawaii) Heart Program. Arch Intern Med. 1991;151:969–72.
- Chyou PH, Eaker ED. Serum cholesterol concentrations and all-cause mortality in older people. Age Ageing. 2000;29: 69–74.
- Kronmal RA, Cain KC, Ye Z, Omenn GS. Total serum cholesterol levels and mortality risk as a function of age. A report based on the Framingham data. Arch Intern Med. 1993;153:1065–73.
- Krumholz HM, Seeman RE, Merrill SS, Mendes de Leon CF, Vaccarino V, Silverman DI, . Lack of association between cholesterol and coronary heart disease mortality in persons older than 70 years. JAMA. 1994;272:1335–9.
- Psaty BM, Anderson M, Kronmal RA, Tracy RP, Orchard T, Fried LP, . Association between lipid levels and the risks of incident myocardial infarction, stroke, and total mortality: The Cardiovascular Health Study. J Am Geriatr Soc. 2004;10:1639–47.
- Jacobs D, Blackburn H, Higgins M, Reed D, Iso H, McMillan G, . Report of the Conference on Low Blood Cholesterol: Mortality Associations. Circulation. 1992;86: 1046–60.
- Iribarren C, Sharp D, Burchfiel CM, Sun P, Dwyer JH. Association of serum total cholesterol with coronary disease and all-cause mortality: Multivariate correction for bias due to measurement error. Am J Epidemiol. 1996; 143:463–71.
- Menotti A, Kromhout D, Nissinen A, Giampaoli S, Seccareccia F, Feskens E, . Short-term all-cause mortality and its determinants in elderly male populations in Finland, The Netherlands, and Italy: the FINE Study. Finland, Italy, Netherlands Elderly Study. Prev Med. 1996;25:319–26.
- Curb JD, Abbott RD, Rodriquez BL, Masaki K, Popper J, Chen R, . Prospective association between low and high total and low-density lipoprotein cholesterol and coronary heart disease in elderly men. disease in elderly men. J Am Geriatr Soc. 2004;52:1975–80.
- White AD, Hames CG, Tyroler HA. Serum cholesterol and 20-year mortality in black and white men and women aged 65 and older in the Evans County Heart Study. Ann Epidemiol. 1992;2:85–91.
- Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD. Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: A cohort study. Lancet. 2001;358:351–5.
- Reuben DB, Ix JH, Greendale GA, Seeman TE. The predictive value of combined hypoalbuminemia and hypocholesterolemia in high functioning community-dwelling older persons: MacArthur Studies of Successful Aging. J Am Geriatr Soc. 1999;47:402–6.
- Forette B, Tortrat D, Wolmark Y. Cholesterol as risk factor for mortality in elderly women. Lancet. 1989;8643:868–70.
- Weverling-Rijnsburger AWE, Blauw GJ, Lagaay AM, Knook DL, Meinders AE, Westendorp RG. Total cholesterol and risk of mortality in the oldest old. Lancet. 1997;350: 1119–23.
- Brescianini S, Maggi S, Farchi G, Mariotti S, Di Carlo A, Baldereschi M, . Low total cholesterol and increased risk of dying: Are low levels clinical warning signs in the elderly? Results from the Italian Longitudinal Study on Aging. J Am Geriatr Soc. 2003;51:991–6.
- Onder G, Landi F, Volpato S, Fellin R, Carbonin P, Gambassi G, . Serum cholesterol levels and in-hospital mortality in the elderly. Am J Med. 2003;115:265–71.
- Abbott RD, Ueshima H, Hozawa A, Okamura T, Kadowaki T, Miura K, . Risk factor effects and total mortality in older Japanese men in Japan and Hawaii. Ann Epidemiol. 2008;18:913–8.
- Schupf N, Costa R, Luchsinger J. Relationship between plasma lipids and all-cause mortality in nondemented elderly. J Am Geriatric Soc. 2005, 53:219–26.
- Akerblom JL, Costa R, Luchsinger JA, Manly JJ, Tang MX, Lee JH, . Relation to all-cause mortality in Caucasian, African-American and Hispanic elders. Age Ageing. 2008;37:207–13.
- Lindroos M, Kupari M, Heikkilä J, Tilvis R. Prevalance of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol. 1993;21:1220–5.
- Tilvis RS, Kähönen-Väre MH, Jolkkonen J, Valvanne J, Pitkala KH, Strandberg TE. Predictors of cognitive decline and mortality of aged people over a 10-year period. J Gerontol A Biol Sci Med Sci. 2004;59:268–74.
- Miettinen TA, Tilvis RS, Kesaniemi YA. Serum plant sterols and cholesterol precursors reflect cholesterol absorption and synthesis in volunteers of a randomly selected male population. Am J Epidemiol. 1990;131:20–31.
- Strandberg TE, Salomaa VV, Vanhanen H, Miettinen TA. Associations of fasting blood glucose with cholesterol absorption and synthesis in nondiabetic middle-aged men. Diabetes. 1996;45:755–61.
- Strandberg TE, Valvanne J, Erkinjuntti T, Sorva A, Tilvis RS. Serum lipids, health, and one-year mortality in randomized age cohorts of 75, 80, and 85 years: the Helsinki Aging Study. Nutr Metab Cardiovasc Dis. 1992;2:101–5.
- Folstein MF, Folstein SE. Mini-Mental State. A practical method for grading the cognitive state of patients for the clinician. J Psychiat Res. 1975;12:189–98.
- Hughes CP, Berg L, Danziger WL, Coben LA, Martin R. A new clinical scale for staging of dementia. Br J Psychiatr. 1982;140:566–72.
- Ehnholm C, Lukka M, Kuusi T, Nikkilä E, Utermann G. Apolipoprotein E polymorphism in the Finnish population: gene frequencies and relation to lipoprotein concentrations. J Lipid Res. 1986;27:227–35.
- Frishman WH, Ooi WL, Derman MP, Eder HA, Gidez LI, Ben-Zeev D, . Serum lipids and lipoproteins in advanced age. Intraindividual changes. Ann Epidemiol. 1992;2:43–50.
- Ferrara A, Barrett-Connor E, Shan J. Total, LDL, and HDL cholesterol decrease with age in older men and women. The Rancho Bernardo Study 1984–1994. Circulation. 1997;96: 37–43.
- Weijenberg MP, Feskens EJ, Kromhout D. Age-related changes in total and high-density-lipoprotein cholesterol in elderly Dutch men. Am J Public Health. 1996;86:798–803.
- Abbott RD, Sharp DS, Burchfiel CM, Curb JD, Rodriguez BL, Hakim AA, . Cross-sectional and longitudinal changes in total and high-density-lipoprotein cholesterol levels over a 20-year period in elderly men: the Honolulu Heart Program. Ann Epidemiol. 1997;7:417–24.
- Kuzuya M, Ando F, Iguchi A, Shimokata H. Changes in serum lipid levels during a 10 year period in a large Japanese population. A cross-sectional and longitudinal study. Atherosclerosis. 2002;163:313–20.
- Kuzuya M, Ando F, Iguchi A, Shimokata H. Age-specific change of prevalence of metabolic syndrome: longitudinal observation of large Japanese cohort. Atherosclerosis. 2007;191:305–12.
- Abbott RD, Curb JD, Rodriguez BL, Masaki KH, Yano K, Schatz IJ, . Age-related changes in risk factor effects on the incidence of coronary heart disease. Ann Epidemiol. 2002;12:173–81.
- Roades DA, Welty TK, Wang W, Yeh F, Devereux RB, Fabsitz RR, . Aging and the prevalence of cardiovascular risk factors in older American Indians: The strong heart study. J Am Geriatr Soc. 2007;55:87–94.
- Anum EA, Adera T. Hypercholesterolemia and coronary heart disease in the elderly: a meta-analysis. Ann Epidemiol. 2004;14:705–21.
- Prospective Studies Collaboration; Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, . Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007; 370:1829–39.
- Clarke R, Emberson JR, Parish S, Palmer A, Shipley M, Linksted P, . Cholesterol fractions and apolipoproteins as risk factors for heart disease mortality in older men. Arch Intern Med. 2007;167:1373–8.
- Strandberg TE, Gylling H, Tilvis RS, Miettinen TA. Serum plant and other noncholesterol sterols, cholesterol metabolism and 22-year mortality among middle-aged men. Atherosclerosis. 2010;210:282–7.
- Silbernagel G, Fauler G, Hoffmann MM, Lütjohann D, Winkelmann BR, Boehm BO, . The associations of cholesterol metabolism and plasma plant sterols with all-cause and cardiovascular mortality. J Lipid Res. 2010;51: 2384–93.
- Papaconstantinou J. Insulin/IGF-1 and ROS signaling pathway cross-talk in aging and longevity determination. Mol Cell Endocrinol. 2009;299:89–100.
- Cluett C, Melzer D. Human genetic variations: Beacons on the pathways to successful ageing. Mech Ageing Dev. 2009; 130:553–63.
- Abellan van Kan G, Rolland Y, Bergman H, Morley JE, Kritchevsky SB, Vellas B. The I.A.N.A Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12:29–37.
- Strandberg TE, Tilvis RS. C-reactive protein, cardiovascular risk factors and mortality in a prospective study in the elderly. Arterioscler Thromb Vasc Biol. 2000;20:1057–60.
- Kähönen MH, Tilvis RS, Jolkkonen J, Pitkälä K, Härkönen M. Predictors and clinical significance of declining plasma dehydroepiandrosterone sulfate in old age. Aging (Milano). 2000;12:308–14.
- Björkman MP, Sorva AJ, Tilvis RS. Elevated serum parathyroid hormone predicts impaired survival prognosis in a general aged population. Eur J Endocrinol. 2008;158:749–53.
- Aronow WS. Management of hyperlipidemia with statins in older adults. Clin Interv Aging. 2006;1:433–8.
- Gränsbo K, Melander O, Wallentin L, Lindbäck J, Stenestrand U, Carlsson J, . Cardiovascular and cancer mortality in very elderly post-myocardial infarction patients receiving statin treatment. J Am Coll Cardiol. 2010;55: 1362–9.
- Glynn RJ, Koenig W, Norgestgaard BG, Shepherd J, Ridker PM. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann Intern Med. 2010;152:488–96.