Abstract
Introduction. To examine whether midregional pro-adrenomedullin (MR-proADM) plasma concentrations predict incident cardiovascular outcomes in the general population. Natriuretic peptides (N-terminal pro-brain natriuretic peptide (NT-proBNP), B-type natriuretic peptide (BNP), and midregional pro-atrial natriuretic peptide (MR-proANP)) were analyzed for comparison.
Material and methods. MR-proADM plasma concentrations and those of the natriuretic peptides were determined in 8444 individuals of the FINRISK 1997 cohort. Patients were followed for 14 years (median). Cox regression analyses, discrimination, and reclassification analyses adjusting for Framingham risk factors were performed to evaluate the additional benefit from MR-proADM.
Results. MR-proADM concentrations significantly predicted all-cause death (hazard ratio highest quintile versus lowest 1.18, 95% confidence interval 1.08–1.28), stroke (1.20, 1.05–1.38), major adverse cardiac events (MACE) (1.27, 1.17–1.37), and heart failure (1.67, 1.49–1.87). MR-proADM remained associated with MACE, death, and heart failure even after additional adjustment for NT-proBNP and C-reactive protein. Adding MR-proADM to the Framingham risk factors significantly improved discrimination (P < 0.001 for C-statistics and integrated discrimination improvement) and risk reclassification for heart failure (net reclassification improvement 12.12%, P < 0.001).
Conclusions. In a healthy general population sample of the FINRISK 1997 cohort MR-proADM significantly predicted all-cause death, MACE, and especially heart failure even beyond NT- proBNP. It also improved risk reclassification for heart failure.
Key messages
In the healthy general population sample of the FINRISK 1997 cohort, MR-proADM plasma concentrations compared to other natriuretic peptides significantly predict incident cardiovascular outcomes (all-cause death, MACE, and especially heart failure) even beyond NT-proBNP. It also improved risk reclassification for heart failure.
Introduction
Cardiovascular diseases (CVD) are the leading cause of death in Western and developing countries (Citation1). Thus, primary preventive strategies of CVD have become one of the main goals of public health policy. Classical risk factors such as blood pressure, cholesterol concentration, smoking, and body mass index (BMI) do not fully explain the distribution of risk in the general population (Citation1,Citation2). Thus, novel biomarkers have received growing attention with regard to risk stratification and initiation of individualized therapies (Citation3,Citation4). Markers of inflammation (Citation5,Citation6), hemostasis and blood rheology (Citation7), troponin (Citation8), and cystatin C (Citation9) have been shown to have predictive ability for CVD in community-based cohorts. Biomarkers reflecting vascular function and neurohumoral activity are of main interest. The natriuretic peptides, especially B-type natriuretic peptide (BNP), N-terminal pro-brain natriuretic peptide (NT-proBNP), and midregional pro-atrial natriuretic peptide (MR-proANP) have predictive ability not only in patients with heart failure and manifest CVD, but also in the general population (Citation10–12).
One novel biomarker in the group of vasoactive and neurohumoral peptides is midregional pro-adrenomedullin (MR-proADM), a stable precursor of adrenomedullin (ADM) which is a peptide originally isolated from human pheochromocytoma tissue (Citation13). It has also been identified in various other tissues, e.g. brain, lung, kidney, gastrointestinal tissues, cardiomyocytes, and smooth muscle cells (Citation14). ADM is a 52-amino acid peptide derived from the precursor protein preproADM by post-translational processing which produces MR-proADM, a flanking protein, in equimolar quantities (Citation15). Thus, concentrations of MR-proADM directly reflect ADM concentrations. Since MR-proADM is more stable and has a longer half-life than its precursor ADM, it serves as target for assays which measure MR-proADM plasma concentrations.
ADM is a vasodilator peptide, which also reduces oxidative stress and inhibits endothelial cell apoptosis. It exerts various effects on different organ systems, e.g. induction of hypotension and bronchodilation or enhancement of renal perfusion (Citation16,Citation17). ADM plasma concentrations are increased in myocardial infarction (MI) (Citation18) and correlate with the severity of congestive heart failure (Citation19). Elevated concentrations of MR-proADM were associated with worse outcome in patients with acute dyspnea (Citation20,Citation21). In patients with chronic heart failure MR-proADM was an independent predictor of mortality and provided additional prognostic information to established biomarkers (e.g. NT-proBNP) (Citation22–24). In patients with stable coronary heart disease (CHD) MR-proADM concentrations were predictive for future CHD events and heart failure (Citation25). In the general population elevated MR-proADM plasma concentrations were associated with the Framingham risk factors, CVD, and heart failure (Citation26). In the general population of the Prevention of REnal and Vascular ENd-stage Disease (PREVEND) cohort MR-proADM was associated with the primary end-point (combined cardiovascular mortality and morbidity), especially in younger subjects (Citation27).
To assess the predictive potential of MR-proADM for incident CVD in initially healthy individuals, we performed an analysis of MR-proADM in the 8444 participants of the FINRISK 1997 study representing a random sample of the adult population of five geographical areas of Finland. We compared the predictive value of MR-proADM to the already established natriuretic peptides BNP, NT-proBNP, and MR-proANP for CVD end-points. Furthermore, we examined the additional effect of MR-proADM on CVD risk over and above the classical risk factors, natriuretic peptides and C-reactive protein (CRP).
Material and methods
Study population
The design of the FINRISK 1997 study is described in detail elsewhere (Citation28). Briefly, the population sample which was examined in 1997 included 8444 individuals aged 25 to 64 years from five geographical areas in Finland (North Karelia, Northern Savo, Southwestern Finland, Oulu province, and the region of Helsinki and Vantaa). A sex- and 10-year age group-stratified random sample was drawn for each survey area with 250 individuals in each stratum. In addition, 250 females and 500 males aged 65–74 years were selected in North Karelia and Helsinki-Vantaa regions. Thus, a total of 11,500 individuals were invited to participate; the response rate was 67% (8444). The follow-up rate for participants who continued to live in Finland was 100%. Individuals who had permanently moved abroad (0.5% of the participants prior to 31 December 2010) were lost to follow-up. The survey included a self-administered questionnaire, physical examination and measurements (height, weight, blood pressure), and blood tests. The study was approved by the Ethics Committee of the National Public Health Institute and conducted according to the Helsinki Declaration. All subjects gave a written informed consent.
Determination of risk factors
Blood pressure was measured with the mercury sphygmomanometer. Measurements were made at the right arm in a sitting position after a ≥ 5-min rest. The mean of two measurements was used in the analyses. Hypertension was determined according to the criteria of the American Heart Association as blood pressure ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic or the use of any antihypertensive drug.
Smoking was assessed by a self-administered questionnaire. Depending on the response, classification was performed into three categories: 1) smokers (who had smoked regularly for ≥ 1 year and still smoked or had quit smoking < 6 months ago); 2) former smokers (who used to smoke regularly but had quit ≥ 6 months before the survey); and 3) non-smokers (who had never smoked regularly).
Baseline diabetes was defined using the questionnaire and the register data explained above either as a doctor-diagnosed disease or impaired glucose tolerance, intake of any hypoglycemic drugs, or hospitalizations with diabetes.
Obesity was defined as a body mass index (BMI) ≥ 30 kg/m² according to the World Health Organization definition.
Follow-up and predefined end-points
Follow-up was performed for 14 years with the use of record linkage of the FINRISK data with three data sources: 1) National Hospital Discharge Register; 2) National Causes of Death Register; and 3) National Drug Reimbursement Register. The first two are countrywide, computerized registers covering all hospitalizations and deaths in Finland. The third one includes all drugs prescribed by a doctor. The high validity of these data on coronary heart disease (CHD) and heart failure has been shown previously (Citation29,Citation30).
End-points during the follow-up were CVD including MI, coronary death, hospitalized unstable angina pectoris, any coronary revascularization (percutaneous transluminal coronary angioplasty or coronary bypass surgery), and ischemic stroke (hemorrhagic strokes were excluded from the analysis), incident heart failure, and major adverse cardiac events (MACE) (CVD or heart failure).
Laboratory analysis
Patients were asked to fast 4 h prior to blood drawing and to avoid heavier meals during the day. The median fasting time was 5 (interquartile range 3–7) h. Serum and plasma samples were stored for the analysis of biomarkers at − 70°C and had not been thawed prior to the analysis. All laboratory measurements, except biomarkers, were carried out at the Disease Risk Unit in the National Institute for Health and Welfare, Helsinki. Biomarker concentrations, including MR-proADM, BNP, NT-proBNP, ANP, creatinine, cystatin C, and troponin I were determined in the MORGAM Biomarker Laboratory, University of Mainz, Germany. MR-proADM was measured with the immunoluminometric assay (B.R.A.H.M.S., Kryptor, Hennigsdorf, Germany). Intra-assay and inter-assay coefficients of variation were 2.17% and 2.43%, and the measuring range was 0.24–27.7 nmol/L. MR-proANP was also measured with the immunoluminometric assay (B.R.A.H.M.S., Kryptor). BNP was measured with the chemiluminescent microparticle immunoassay CMIA (Abbott, Architect i2000, Illinois, USA), NT-proBNP was measured with the electrochemiluminescence sandwich immunoassay ECLIA (Roche Diagnostics, Elecsys 2010, Berlin, Germany), cystatin C (mg/L) with the latex immunoassay (Abbott, Architect c8000), creatinine (mg/dL) with kinetic assay (Abbott, Architect c8000), and troponin I (ng/mL) with the chemiluminescent microparticle immunoassay CMIA (Abbott, Architect i2000). BNP, MR-proADM, MR-proANP, and cystatin C were measured from plasma (EDTA); NT-proBNP, creatinine, and troponin from serum.
All intra- and inter-assay coefficients of variation as well as other details of measurements have been documented previously (Citation31).
Statistical analysis
Baseline characteristics are presented as counts and percentages for dichotomous variables, and as median and interquartile range for continuous variables. MR-proADM was analyzed in quintiles: < 0.36, ≥ 0.36–0.48, ≥ 0.48–0.50, ≥ 0.50–0.59, and ≥ 0.59 nmol/L. The natriuretic peptides (NT-proBNP, BNP, MR-proANP) were categorized into quintiles as well. Quintiles for NT-proBNP were: < 17.6, ≥ 17.6–33.9, ≥ 33.9–57.9, ≥ 57.9–101.8, and ≥ 101.8 pg/mL; for BNP: < 6.21, ≥ 6.21–11.32, ≥ 11.32–18.54, ≥ 18.54–32.92, and ≥ 32.92 pg/mL; MR-proANP: < 30.0, ≥ 30.0–38.5, ≥ 38.5–48.8, ≥ 48.8–67.2, and ≥ 67.2 pmol/L. Comparisons over these quintiles were performed with a linear trend test, using a generalized linear model for continuous quintiles. Kaplan–Meier curves for MACE and heart failure were created using MR-proADM quintiles and adjusting for age and sex. To determine the association of MR-proADM with the incident disease outcomes, Cox regression analyses with age as the time-scale were performed with the first quintile as the reference category, adjusting for the variables of the Framingham risk score (log-transformed total cholesterol, log-transformed HDL cholesterol, log-transformed systolic blood pressure, antihypertensive medication, diabetes, current smoking) and the geographic region of Finland (west, east). The validity of the proportional hazards assumptions was checked using the cox.zph procedure in R.
Modern metrics of discrimination and reclassification, including ROC curves, C-statistics, integrated discrimination improvement (IDI), and net reclassification improvement (NRI) with risk categories 0%–5%, 5%–10%, 10%–20%, and > 20% for 10-years risk was used to determine the additional value of MR-proADM concentration over and above the Framingham risk score (Citation32,Citation33). Multiple imputation techniques were used to cope with missing values (Citation31,Citation34). Ten-fold cross-validation was used to control for over-optimism. All statistical analyses were performed with R version 15.1 (R Foundation for Statistical Computing, Vienna, Austria). All tests were two-tailed, and P < 0.05 was considered statistically significant.
Results
Baseline characteristics stratified by MR-proADM quartile
shows the baseline demographics, cardiovascular risk factors, and clinical parameters of cardiovascular disease as categorized by MR-proADM quintile. A total of 7899 subjects (50.3% women, 49.7% men) were included in the analyses after exclusion of pregnant women and subjects with prevalent MACE. The mean age at inclusion was 48 years. The mean baseline concentration of MR-proADM was 0.46 nmol/L. During the follow-up 810 subjects died, including 86 fatal MIs. Incident MACE occurred in 1074 subjects, including 299 ischemic strokes, 770 CVD events, and 505 incident heart failures. Subjects with higher MR-proADM concentrations were older and more likely to be female (P < 0.001). In general, higher MR-proADM levels were found in patients with a worse cardiovascular risk profile. (Subjects were more likely to suffer from hypertension, diabetes, to be current smokers, have higher BMI, higher systolic blood pressure, higher total cholesterol , and lower HDL concentrations; all P < 0.001.) Patients from higher quintiles had an impaired renal function (cystatin C, eGFR MDRD). With increasing MR-proADM quintiles people had a significantly higher risk for all-cause death (23.0% versus 3.9%, P < 0.001), MACE (30.8% versus 4.8%, P < 0.001), CVD (20.7% versus 4.1%, P = 0.0093), incident ischemic stroke (8.9% versus 1.3%, P = 0.002), and especially for incident heart failure (17.6% versus 1.1%, P < 0.001). No statistically significant association was observed for MI (7.8% versus 1.7%, P = 0.16).
Table I. Characteristics of the study population.
Association of baseline MR-proADM quintiles with cardiovascular outcome
presents Kaplan–Meier curves for MACE and heart failure, adjusted for age and sex, showing higher disease-free survival rates for the lowest MR-proADM quintiles. shows the results of Cox regression models with HRs adjusted for Framingham risk factors for various cardiovascular outcomes comparing the highest quintile of baseline MR-proADM, BNP, NT-proBNP, and MR-proANP with the respective lowest quintile. HRs for MR-proADM were significantly increased for all-cause death 1.18 (95% CI 1.08–1.28, P < 0.001), ischemic stroke 1.20 (1.05–1.38, P = 0.0095), MACE 1.27 (1.17–1.37, P < 0.001), and heart failure 1.67 (1.49–1.87, P < 0.001). No association was observed with CHD, MI, and CVD. HRs for NT-proBNP and BNP were significant for all outcomes (CHD, MI, CVD, all-cause death, stroke, MACE, and heart failure) (for NT-proBNP all P < 0.001; for BNP for death and MI P < 0.01; for all other end-points P < 0.001). HRs for MR-proANP were significant for CVD, all-cause death, ischemic stroke, MACE, and heart failure (CVD P < 0.01; all other end-points P < 0.001). After additional adjustment for C-reactive protein and NT-proBNP HRs for MR-proADM became smaller but still remained significant for MACE 1.12 (1.04–1.21, P = 0.0046) and highly significant for all-cause death 1.18 (1.08–1.28, P < 0.001) and heart failure 1.42 (1.26–1.60, P < 0.001) (Supplementary Table I available online at http://informahealthcare.com/doi/abs/10.3109/07853890.2013.874662).
Figure 1. Kaplan–Meier Curves by quintile of midregional pro-adrenomedullin (MR-proADM) for major adverse cardiac events (MACE) and heart failure after adjustment for age and gender. Dotted lines indicate the 95% confidence intervals. C1: Quintile 1, MR-proADM concentration < 0.36 nmol/L; C2: Quintile 2, MR-proADM concentration ≥ 0.36–0.48 nmol/L; C3: Quintile 3, MR-proADM concentration ≥ 0.48–0.50; C4: Quintile 4, MR-proADM concentration ≥ 0.50–0.59; C5: Quintile 5, MR-proADM concentration ≥ 0.59.
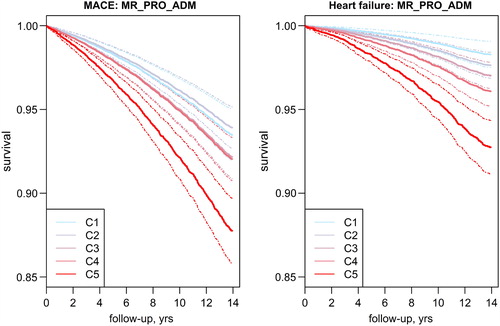
Figure 2. Hazard ratios of different outcomes for baseline midregional pro-adrenomedullin, N-terminal pro-brain natriuretic peptide, B-type natriuretic peptide, and midregional pro-atrial natriuretic peptide. Cox proportional hazards regression models comparing the highest quintile of each biomarker with the lowest quintile have been adjusted for the Framingham risk factors.
Risk discrimination and risk reclassification
MR-proADM significantly improved discrimination for MACE and heart failure (C-statistic and integrated discrimination improvement (IDI) P < 0.001) (). Adding MR-proADM to the Framingham equation significantly improved risk reclassification for heart failure (NRI 12.12%, P < 0.001) (). For subjects at intermediate 10-year risk according to the Framingham risk score (5%–20%) adding MR-proADM resulted in even higher NRIs (clinical NRIs) for heart failure (25%, P < 0.001), all-cause death (10.54%, P < 0.001), MACE (13.91%, P < 0.001), and ischemic stroke (7.35%, P = 0.0476). For NT-proBNP the NRIs were significant for all outcomes, except all-cause death. The clinical NRI was significant for all outcomes. For BNP the NRI was significant for heart failure (10.28%, P = 0.0011), the clinical NRI for all end-points, except for MI. For MR-proANP the NRI was significant for heart failure (8.10%, P = 0.0099) and stroke (7.32%, P = 0.0278). After additional adjustment for NT-proBNP and CRP the NRI for MR-proADM remained significant for heart failure (6.98%, P = 0.0039), and the clinical NRI for heart failure became even stronger (15.53%, P < 0.001) (Supplementary Table II available online at http://informahealthcare.com/doi/abs/10.3109/07853890.2013.874662). The clinical NRI was also significant for MACE (5.61%, P < 0.001).
Table II. C-statistics and integrated discrimination improvement (IDI) for various cardiovascular outcomes due to adding baseline MR-proADM, NT-proBNP, BNP, and MR-proANP to the Framingham risk score.
Table III. Net reclassification improvement (NRI) and clinical NRI for various cardiovascular outcomes due to adding baseline MR-proADM, MR-proADM, NT-proBNP, BNP, and MR-proANP to the standard Framingham risk score.
Discussion
This study examined the predictive ability of baseline MR-proADM concentrations in a population-based setting in subjects without a history of MACE and presents similar analyses for natriuretic peptides for comparison. We observed an association of MR-proADM with MACE, stroke, all-cause death, and especially with heart failure. NT-proBNP was the strongest predictor amongst the natriuretic peptides and was clearly associated with all end-points (including MI and CVD). BNP and MR-proANP were also associated with all end-points (except MR-proANP with MI), although less strongly than NT-proBNP. Interestingly, MR-proADM was predominantly associated with incident heart failure with a HR comparable to that of NT-proBNP. After additional adjustment for NT-proBNP and C-reactive protein the predictive value of MR-proADM remained for all-cause death, MACE, and especially for heart failure. Net reclassification improvement was only significant for heart failure. In subjects with intermediate risk, however, clinical net reclassification was also significantly improved for all-cause death, MACE, stroke, and especially for heart failure.
MR-proADM has emerged as a promising biomarker predicting cardiovascular events in a variety of diseases such as MI, heart failure, and stable CHD. Unlike the natriuretic peptides, however, the predictive value for MR-proADM in the general population has not been established. The community-based Malmö Diet and Cancer Study evaluated amongst other biomarkers the performance of MR-proADM for the prediction of heart failure and atrial fibrillation (Citation35). For coronary events a weak association has been shown with MR-proADM (Citation36). However, differing from our study, no additional analysis after further adjustment for NT-proBNP and/or C-reactive protein was performed. In the PREVEND cohort an association of MR-proADM with the primary end-point (combined cardiovascular mortality and morbidity) was observed (Citation27). No significant risk reclassification was observed in that study.
Interestingly, in the general population of the Gutenberg Health Study it was shown that MR-proADM concentrations correlate with echocardiographic parameters of left-ventricular systolic and diastolic function. Thus, elevated MR-proADM concentrations in the FINRISK population could reflect early changes of the myocardium leading to counter-regulatory up-regulation of ADM and consequently MR-proADM. This might explain the predictive capacity of MR-proADM especially for incident heart failure. For CVD and MI, the predictive value of MR-proADM did not reach statistical significance. For MI we cannot exclude the possibility that this is due to the low number of events (MI n = 277). However, since the number of events was higher for CVD (n = 770) one can assume that this might be due to the fact that in the general population MR-proADM rather accounts for early changes indicating future heart failure than for incident MI. MI usually occurs after an acute plaque rupture or acute thromboembolic event which is presumably not preceded by changes needing counter-regulatory up-regulation of MR-proADM. This is a different process from early structural changes in the heart that occurs long before the first symptoms of heart failure arise (e.g. moderate impairment of systolic function, left-ventricular hypertrophy, early stages of diastolic dysfunction, grade I and II). This might primarily stem from a presumably healthy population and seems to be different in clinical settings. In patients with stable CHD and preserved ejection fraction of the AtheroGene study, biomarkers reflecting cardiovascular stress (e.g. MR-proADM, natriuretic peptides) were more predictive of CHD death and incident heart failure than of the composite of CHD death and MI (Citation25). The particular strength of the present study is the determination of MR-proADM in a large well-characterized cohort of the FINRISK 1997 study with a long follow-up. Additionally, MR-proADM was compared with the established natriuretic peptides NT-proBNP, BNP, MR-proANP and further evaluated after additional adjustment for NT-proBNP and CRP.
Some limitations have to be considered, however. Since all biomarker analyses were performed using samples which had been stored for 14 years, we cannot exclude the possibility that some distortion of the results may have occurred. Furthermore, since MR-proADM is elevated in a variety of diseases and pathophysiological conditions, it is possible that the results were biased by such a condition which had not been recorded at baseline. The identification of incident heart failure was based on registry data and not on echocardiography or other more detailed examinations. Our earlier validation study shows, however, that the specificity of registry-based diagnosis is excellent, although sensitivity is modest. Finally, this study has been performed in the Finnish population. Therefore, the results might not directly apply to other countries or other ethnic groups.
In conclusion we showed that baseline MR-proADM concentrations in the general population of the FINRISK 1997 cohort were significantly associated with incident MACE, stroke, all-cause death, and especially with heart failure. No association was observed with MI or CVD. This was different from the natriuretic peptides NT-proBNP and BNP which were strongly associated with heart failure but with vascular events as well, thus being less specific for heart failure than MR-proADM. Similarly to MR-proADM, MR-proANP showed no significant association with MI, but HRs for heart failure were much lower compared to those of MR-proADM. Most importantly, the association of MR-proADM with heart failure remained significant after additional adjustment for NT-proBNP and CRP; for MR-proANP this was not the case (data not shown). Additionally, MR-proADM significantly improved risk reclassification for heart failure, even after additional adjustment for NT-proBNP and CRP. Thus, MR-proADM might be a promising biomarker for predicting the risk of incident heart failure in the general population beyond classical Framingham risk factors and NT-proBNP.
Supplementary Tables I and II
Download PDF (41.4 KB)Declaration of interest: This work has been sustained by the MORGAM Project's current funding: European Community FP 7 projects ENGAGE CHANCES and BiomarCaRE. V.S. was supported by the Finnish Foundation for Cardiovascular Research. S.B. has received research funding from Abbott, Abbott Diagnostics, Bayer, Boehringer Ingelheim, SIEMENS, and Thermo Fisher. He received honoraria for lectures from Abbott, Abbott Diagnostics, Astra Zeneca, Bayer, Boehringer Ingelheim, Medtronic, Pfizer, Roche, SIEMENS Diagnostics, SIEMENS, Thermo Fisher, and as member of Advisory Boards and for consulting for Boehringer Ingelheim, Bayer, Novartis, Roche, and Thermo Fisher. All other authors did not report any conflict.
References
- Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007;14(Suppl 2):S1–113.
- Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, et al. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106:388–91.
- Koenig W. Update on integrated biomarkers for assessment of long-term risk of cardiovascular complications in initially healthy subjects and patients with manifest atherosclerosis. Ann Med. 2009;41:332–43.
- Romanens M, Ackermann F, Spence JD, Darioli R, Rodondi N, Corti R, et al. Improvement of cardiovascular risk prediction: time to review current knowledge, debates, and fundamentals on how to assess test characteristics. Eur J Cardiovasc Prev Rehabil. 2010;17:18–23.
- Engstrom G, Lind P, Hedblad B, Stavenow L, Janzon L, Lindgarde F. Effects of cholesterol and inflammation-sensitive plasma proteins on incidence of myocardial infarction and stroke in men. Circulation. 2002;105:2632–7.
- Mora S, Rifai N, Buring JE, Ridker PM. Additive value of immunoassay-measured fibrinogen and high-sensitivity C-reactive protein levels for predicting incident cardiovascular events. Circulation. 2006;114:381–7.
- Lowe GD, Sweetnam PM, Yarnell JW, Rumley A, Rumley C, Bainton D, et al. C-reactive protein, fibrin D-dimer, and risk of ischemic heart disease: the Caerphilly and Speedwell studies. Arterioscler Thromb Vasc Biol. 2004;24:1957–62.
- de Lemos JA, Drazner MH, Omland T, Ayers CR, Khera A, Rohatgi A, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304:2503–12.
- Zethelius B, Berglund L, Sundstrom J, Ingelsson E, Basu S, Larsson A, et al. Use of multiple biomarkers to improve the prediction of death from cardiovascular causes. N Engl J Med. 2008;358:2107–16.
- van Hateren KJ, Alkhalaf A, Kleefstra N, Groenier KH, de Jong PE, de Zeeuw D, et al. Comparison of midregional pro-A-type natriuretic peptide and the N-terminal pro-B-type natriuretic peptide for predicting mortality and cardiovascular events. Clin Chem. 2012;58:293–7.
- Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Omland T, et al. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350:655–63.
- McKie PM, Cataliotti A, Sangaralingham SJ, Ichiki T, Cannone V, Bailey KR, et al. Predictive utility of atrial, N-terminal pro-atrial, and N-terminal pro-B-type natriuretic peptides for mortality and cardiovascular events in the general community: a 9-year follow-up study. Mayo Clin Proc. 2011;86:1154–60.
- Kitamura K, Kangawa K, Kawamoto M, Ichiki Y, Nakamura S, Matsuo H, et al. Adrenomedullin: a novel hypotensive peptide isolated from human pheochromocytoma. Biochem Biophys Res Commun. 1993;192:553–60.
- Kitamura K, Kangawa K, Kojima M, Ichiki Y, Matsuo H, Eto T. Complete amino acid sequence of porcine adrenomedullin and cloning of cDNA encoding its precursor. FEBS Lett. 1994;338:306–10.
- Morgenthaler NG, Struck J, Alonso C, Bergmann A. Measurement of midregional proadrenomedullin in plasma with an immunoluminometric assay. Clin Chem. 2005;51:1823–9.
- Kitamura K, Kangawa K, Eto T. Adrenomedullin and PAMP: discovery, structures, and cardiovascular functions. Microsc Res Tech. 2002;57: 3–13.
- Ishiyama Y, Kitamura K, Ichiki Y, Nakamura S, Kida O, Kangawa K, et al. Hemodynamic effects of a novel hypotensive peptide, human adrenomedullin, in rats. Eur J Pharmacol. 1993;241:271–3.
- Kobayashi K, Kitamura K, Hirayama N, Date H, Kashiwagi T, Ikushima I, et al. Increased plasma adrenomedullin in acute myocardial infarction. Am Heart J. 1996;131:676–80.
- Kobayashi K, Kitamura K, Etoh T, Nagatomo Y, Takenaga M, Ishikawa T, et al. Increased plasma adrenomedullin levels in chronic congestive heart failure. Am Heart J. 1996;131:994–8.
- Potocki M, Breidthardt T, Reichlin T, Morgenthaler NG, Bergmann A, Noveanu M, et al. Midregional pro-adrenomedullin in addition to b-type natriuretic peptides in the risk stratification of patients with acute dyspnea: an observational study. Crit Care. 2009;13:R122.
- Christ-Crain M, Morgenthaler NG, Struck J, Harbarth S, Bergmann A, Muller B. Mid-regional pro-adrenomedullin as a prognostic marker in sepsis: an observational study. Crit Care. 2005;9:R816–24.
- Potocki M, Breidthardt T, Reichlin T, Hartwiger S, Morgenthaler NG, Bergmann A, et al. Comparison of midregional pro-atrial natriuretic peptide with N-terminal pro-B-type natriuretic peptide in the diagnosis of heart failure. J Intern Med. 2010;267:119–29.
- Masson S, Latini R, Carbonieri E, Moretti L, Rossi MG, Ciricugno S, et al. The predictive value of stable precursor fragments of vasoactive peptides in patients with chronic heart failure: data from the GISSI-heart failure (GISSI-HF) trial. Eur J Heart Fail. 2010;12:338–47.
- Gegenhuber A, Struck J, Dieplinger B, Poelz W, Pacher R, Morgenthaler NG, et al. Comparative evaluation of B-type natriuretic peptide, mid-regional pro-A-type natriuretic peptide, mid-regional pro-adrenomedullin, and Copeptin to predict 1-year mortality in patients with acute destabilized heart failure. J Card Fail. 2007;13:42–9.
- Wild PS, Schnabel RB, Lubos E, Zeller T, Sinning CR, Keller T, et al. Midregional proadrenomedullin for prediction of cardiovascular events in coronary artery disease: results from the AtheroGene study. Clin Chem. 2012;58:226–36.
- Neumann JT, Tzikas S, Funke-Kaiser A, Wilde S, Appelbaum S, Keller T, et al. Association of MR-proadrenomedullin with cardiovascular risk factors and subclinical cardiovascular disease. Atherosclerosis. 2013;228:451–9.
- Brouwers FP, de Boer RA, van der Harst P, Struck J, de Jong PE, de Zeeuw D, et al. Influence of age on the prognostic value of mid-regional pro-adrenomedullin in the general population. Heart. 2012;98:1348–53.
- Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Mannisto S, Sundvall J, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol. 2010;39:504–18.
- Pajunen P, Koukkunen H, Ketonen M, Jerkkola T, Immonen-Raiha P, Karja-Koskenkari P, et al. The validity of the Finnish Hospital Discharge Register and Causes of Death Register data on coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2005;12:132–7.
- Mahonen M, Jula A, Harald K, Antikainen R, Tuomilehto J, Zeller T, et al. The validity of heart failure diagnoses obtained from administrative registers. Eur J Prev Cardiol. 2013;20:254–9.
- Blankenberg S, Zeller T, Saarela O, Havulinna AS, Kee F, Tunstall-Pedoe H, et al. Contribution of 30 biomarkers to 10-year cardiovascular risk estimation in 2 population cohorts: the MONICA, risk, genetics, archiving, and monograph (MORGAM) biomarker project. Circulation. 2010;121:2388–97.
- Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72; discussion 207–12.
- Cook NR. Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Clin Chem. 2008;54:17–23.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30: 377–99.
- Smith JG, Newton-Cheh C, Almgren P, Struck J, Morgenthaler NG, Bergmann A, et al. Assessment of conventional cardiovascular risk factors and multiple biomarkers for the prediction of incident heart failure and atrial fibrillation. J Am Coll Cardiol. 2010;56:1712–19.
- Melander O, Newton-Cheh C, Almgren P, Hedblad B, Berglund G, Engstrom G, et al. Novel and conventional biomarkers for prediction of incident cardiovascular events in the community. JAMA. 2009;302: 49–57.

