Abstract
Cardiac biomarker troponin can be elevated in patients without a primary cardiac diagnosis and may have prognostic value. We conducted a systematic review to estimate the prevalence and prognostic significance of elevated troponin levels in patients admitted to hospital without a primary cardiac diagnosis. Literature search was done using MEDLINE (1946 to November 2012), EMBASE (1974 to Week 45, 2012), and Cochrane Central Register of Controlled Trials (November 2012). Two independent investigators reviewed full-text studies for final inclusion. We included studies of patients admitted without a primary cardiac diagnosis. Eligible studies compared adverse outcomes in patients with normal versus elevated troponin levels. Twenty-seven studies were included in the meta-analysis. Elevated troponin was associated with increased in-hospital and 30-day mortality (25 studies, 7255 patients, OR 3.88, 95% CI 2.90–5.19, P < 0.0001). Elevated troponin was also associated with increased risk of long-term mortality at 6 months (9 studies, 5368 patients, OR 4.21, 95% CI 1.84–9.64, P < 0.00001). Troponin is an independent predictor of short-term mortality with a pooled adjusted OR of 2.36, 95% CI 1.47–3.76, P < 0.0003. In conclusion, elevated troponin in non-cardiac patients is independently associated with increased mortality.
Key words::
Key messages
Troponin elevation is common in acutely hospitalized patients without a primary cardiac diagnosis.
Troponin elevation is associated with a statistically significant increase in short-term and long-term mortality.
Introduction
Myocardial infarction represents a major health problem that has not only clinical but also social, psychological, and economic implications. Troponin is a measurement of myocardial injury and a diagnostic marker for acute coronary syndrome (Citation1). It is frequently measured in patients not presenting with a cardiac problem, in order to rule out myocardial infarction (Citation2–4). The clinical implication and prognostic value of elevated troponin in the absence of a primary cardiac diagnosis is not well understood.
Cardiac troponins have been studied as prognostic markers in acute coronary syndrome (ACS) patients (Citation3). Elevated troponins are significantly associated with an increase in all-cause mortality (Citation5–7). Peak troponin levels are also an independent predictor of major adverse cardiac events (MACE) and heart failure at follow-up (Citation8).
Cardiac biomarkers can be elevated without a diagnosis of ACS and may also have prognostic value. An elevated troponin level itself does not provide information about the underlying mechanism for troponin release and requires interpretation in the clinical context of each patient. The prevalence and prognostic significance of elevated troponin levels in the absence of ACS need to be further studied.
We did a comprehensive systematic review and meta-analysis to address the following questions: What is the prevalence of troponin elevation in patients admitted without a primary cardiac diagnosis, and is there an association between troponin elevation and adverse outcomes in these patients?
Methods
Study eligibility
We included all studies with non-cardiac patients with the following inclusion criteria: Patients that were 18 years or older; acutely admitted to hospital without a primary cardiac diagnosis; patients with either troponin T or troponin I measured; comparison of elevated and normal troponin for at least one adverse outcome including mortality, readmission to hospital, and MACE (major adverse cardiac outcomes). We defined admission with a primary cardiac diagnosis a priori as admission for acute coronary syndrome, post-cardiac arrest, congestive heart failure, arrhythmias, cardiomyopathy, pericarditis, and valvular heart disease including those due to infective endocarditis. We excluded studies with the primary population having end-stage renal disease due to potential troponin elevation secondary to decreased renal clearance.
Study identification
To identify relevant literature, the systematic literature searches were conducted in MEDLINE (1946 to November 2012), EMBASE (1974 to Week 45, 2012), and Cochrane Central Register of Controlled Trials (November 2012) by a clinical librarian with experience in conducting electronic literature searches. No language restrictions were applied.
A sensitive search strategy (Supplementary Appendix 1, to be found online at http://informahealthcare.com/doi/abs/10.3109/07853890.2014.959558) was based on combination of subject headings and keywords using alternative spellings and word endings. Optimized search filters and text words were used to refine search results to randomized controlled trials and prognostic and observational studies published on the topic. The search strategies were altered for each database to include specific terms, field names, and search filters. In addition, the bibliographies of relevant retrieved individual studies and selected reviews were hand-searched for relevant citations, and ‘clinicaltrials.gov’ (of NLM) was also searched to identify unpublished trials.
Study selection
We screened the title and abstract of each study identified by the above search strategy. We retrieved the full-text article for any study identified as potentially fulfilling eligibility criteria based on title and abstract.
Two reviewers independently assessed all full-text studies for final inclusion. We used a standardized inclusion/exclusion form to review each study (Supplementary Appendix 2, to be found online at http://informahealthcare.com/doi/abs/10.3109/07853890.2014.959558). Disagreements in inclusion and exclusion were resolved by discussion between the two reviewers, and any further disagreement was resolved by a third reviewer.
Data collection and quality assessment
One review author extracted the data, and a second author independently checked the data. We abstracted the following data for all included studies: type of study, study period, primary patient population or reason for admission, primary outcome, number of total patients, type of troponin measured (fourth-generation troponin T, high-sensitivity troponin T, or troponin I), troponin threshold, timing of troponin measured, and length of follow-up. We also abstracted number of patients in normal versus elevated troponin study arms, number of deaths, readmissions, or MACE if reported. If the number of patients in normal versus elevated troponin or the number of deaths in each arm was not reported, we contacted the corresponding authors to request the data.
We abstracted the following data for quality assessment and assessing risk of bias in individual studies: type of study, whether eligibility criteria were clear, completeness and method of follow-up, blinding of outcome assessors, and factors adjusted for in multivariate analysis if performed.
Statistical analysis
We used kappa (κ) statistic to quantify inter-observer agreement for study eligibility. Eight studies that met eligibility criteria did not report n/N and are not included in the univariate meta-analysis. We calculated unadjusted odds ratios (OR) for each individual study using n/N and used random effects model to estimate the pooled ORs (Citation9). We assessed heterogeneity across study results using an I2 value. We used the GRADE approach (Citation10) to characterize the risk of bias for each of the outcomes. We assessed risk of bias across studies by evaluating a funnel plot. We also did subgroup analysis for studies with specific patient populations to compare pooled ORs for short-term mortality. Eight studies reported multivariate analysis with adjusted ORs.
Results
Our initial search strategy retrieved 3639 articles. After initial screening, we selected 142 abstracts for full text review. We selected 27 studies (Citation11–37) for final inclusion in the systematic review (). Eight studies reported multivariate analysis with adjusted ORs (Citation13,Citation18,Citation23,Citation25,Citation27,Citation28,Citation34,Citation35). Inter-observer agreement for study inclusion was excellent with κ = 0.96.
Characteristics of studies included
The 27 studies included in the meta-analysis enrolled 7921 patients, with the study sample size ranging from 40 to 4433. presents a summary of the characteristics of the included studies. The majority of studies were prospective (17 studies), and the remaining were retrospective. Ten studies included patients with critical illness or patients admitted to an intensive care unit (ICU). Seven studies included patients with pulmonary embolism (PE), five with sepsis or an acute infection requiring hospitalization, three with chronic obstructive lung disease (COPD) exacerbation, one with diabetic ketoacidosis (DKA), and one with hypertensive emergency. Seventeen studies investigated troponin I, eight studies evaluated troponin T, and two studies evaluated high-sensitivity troponin T. The duration of follow-up varied from 28 days to 4 years, or until discharge for in-hospital mortality.
Table I. Characteristics of studies included in systematic review.
Quality of included studies
presents a summary of the quality assessment for all included studies. All studies had a clear question, with the majority of studies evaluating troponin as the primary variable for assessing adverse outcomes. All studies had clear inclusion and exclusion criteria. Most studies looked at in-hospital mortality as the primary outcome and therefore had complete follow-up. There was good follow-up for most studies looking at post-discharge outcomes. Four studies did not explicitly state whether follow-up was complete or not. The overall quality of evidence was moderate ().
Table II. Study quality characteristics.
Table III. Summary of findings of meta-analysis.
Prevalence of elevated troponin
Troponin elevation is common (3585/7921, 45%) in acutely hospitalized patients even in the absence of ACS or a primary cardiac diagnosis. The troponin assays and therefore the threshold for definition of elevated troponin varied among centres and studies. Prevalence of elevated troponin is similar both in troponin T (1641/3677, 45%) and troponin I (1373/3052, 45%) studies, but higher in the two studies with elevated high-sensitivity troponin T (385/625, 62%).
Mortality and elevated troponin
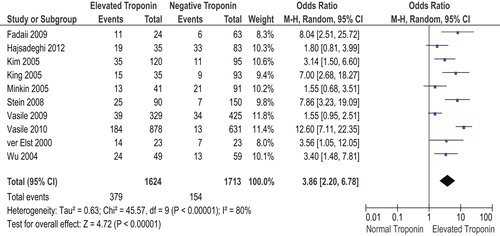
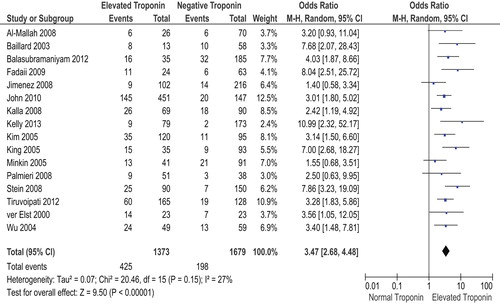
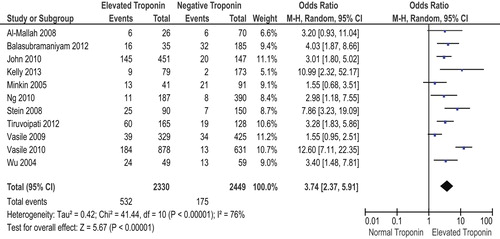
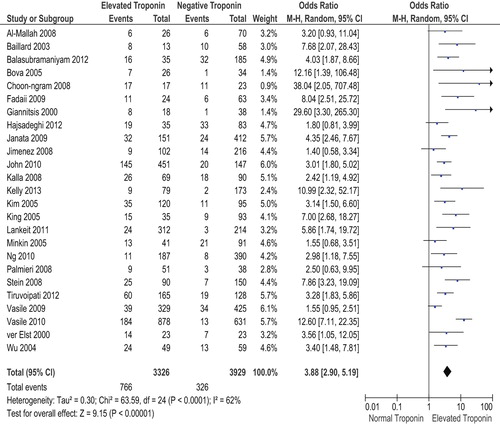
We performed a meta-analysis of 25 studies with n/N reported to calculate unadjusted OR for short-term mortality (in-hospital or ≤ 30 days) for elevated troponin in non-cardiac inpatients (). The 25 studies enrolled a total of 7255 patients with 1092 deaths. For all included studies, the point estimate for the risk of mortality associated with an elevated troponin was greater than unity. The meta-analysis of the 25 studies showed that an increased troponin in non-cardiac medicine inpatients is a predictor of short-term mortality with an OR of 3.88 and 95% CI of 2.90–5.19, P < 0.0001. There was moderate heterogeneity with an I2 of 62%.
Figure 2. Forest plot of short-term (in-hospital and ≤ 30 days) mortality in elevated troponin versus normal troponin groups.
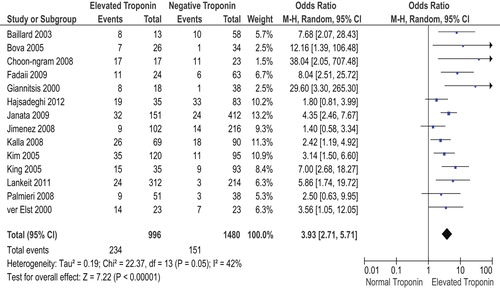
We pooled the results of nine studies to calculate an unadjusted OR for long-term mortality (≥ 6 months) and elevated troponin in non-cardiac inpatients (, ). The nine studies enrolled a total of 5368 patients. There were 1611 deaths during follow-up. An increased troponin level in non-cardiac medicine patients was a predictor of long-term mortality with an OR of 4.21 and 95% CI of 1.84–9.64, P < 0.00001. There was significant heterogeneity in these results with an I2 of 96%.
Figure 3. Forest plot of long-term (≥ 6 months) mortality in elevated troponin versus normal troponin groups.
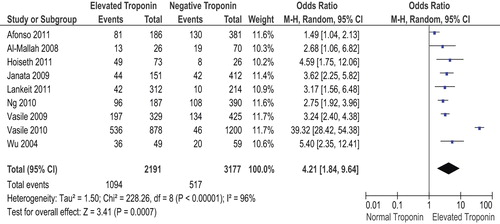
Eight studies also reported adjusted ORs based on multivariate analysis. We pooled the adjusted ORs (), and an increased troponin in non-cardiac medicine inpatients was an independent predictor of short-term mortality with an adjusted pooled OR of 2.36 and 95% CI of 1.47–3.76, P < 0.0003).
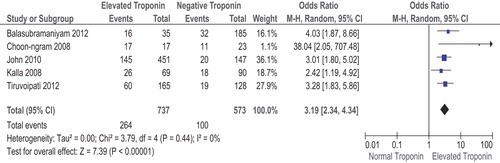
Subgroup analysis
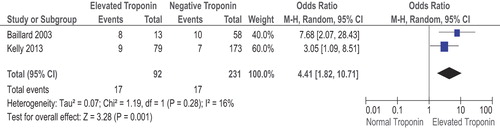
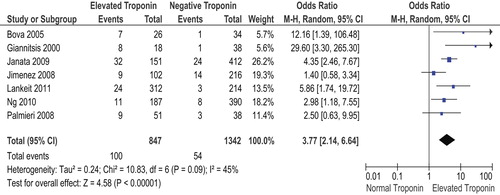
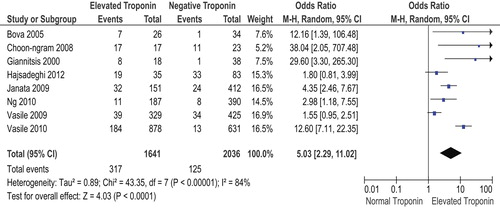
report meta-analysis of studies separated based on reason for admission. We performed a subgroup analysis to test whether this was a source of heterogeneity. Studies were grouped according to reason for admission (critical illness/ICU, sepsis, COPD, and PE), and I2 was lower in sepsis, COPD, and PE, respectively (I2 0%, 16%, and 45%). All subgroups showed same association between elevated troponin and increased mortality. Subgroup analysis based on troponin I versus troponin T did not explain the source of heterogeneity ( and ).
Our meta-analysis includes both retrospective and prospective studies. Retrospective analysis of patients with a non-cardiac discharge diagnosis may differ from patients admitted with a preliminary diagnosis and followed prospectively after troponin measurement. However, the same association between elevated troponin and increased short-term mortality is seen for both study designs ( and ).
Discussion
Our meta-analysis indicates that there is a high prevalence of elevated troponin in non-cardiac hospitalized patients. Furthermore, troponin elevation is associated with an increase in 30-day and 6-month mortality. Most studies did not have a significant difference in baseline cardiac risk factors or underlying cardiac disease in elevated versus normal troponin groups, which can potentially be a confounding factor. Therefore, we pooled the adjusted ORs of eight studies that did multivariate analysis. Troponin elevation is an independent predictor of increased mortality. The association between troponin elevation and mortality is significant for all patient populations studied, regardless of underlying diagnosis.
Strengths and limitations
Our systematic review has several strengths. We carried out a comprehensive literature search without any language restrictions, and the included studies were from diverse geographic regions. Study eligibility was assessed by two independent reviewers with good agreement. Our meta-analysis had substantial statistical power, with a large total population and high incidence of outcomes. There was a consistent significant association between troponin elevation and mortality.
There are some limitations to our systematic review. There is heterogeneity in the studies included, but all studies demonstrated the same overall trend towards an increased risk of mortality. The likely source of heterogeneity is the diverse patient population. The studies used different troponin assays with varying cut-offs to define troponin elevation. The timing of the studies also influenced the troponin assay and reference values used, but again the same trend towards increased mortality is observed regardless of assay. This meta-analysis is limited by the quality of the underlying evidence and study designs. All included studies are observational, and therefore association does not imply causation.
Implications and future research
Detectable and elevated troponin may represent a spectrum from myocardial injury to ischemia leading to necrosis. With the introduction of high-sensitivity assays for markers of myocardial injury, detectable and elevated troponin levels in the absence of myocardial necrosis become more common. This has led to a recent update in the definition of myocardial infarction by the Joint ESC/ACCF/AHA/WHF Task Force (Citation38). Our systematic review had a limited number of studies evaluating prognosis of elevated high-sensitivity troponin levels in patients without a primary cardiac diagnosis. Further studies are needed to evaluate the association between elevated high-sensitivity troponin and adverse outcomes in non-cardiac patients. High-sensitivity assays, which are becoming more commonly used in clinical practice challenge how we interpret detectable and elevated troponin levels. High-sensitivity assays may increase diagnostic accuracy with increased sensitivity for myocardial ischemia (Citation39,Citation40) and better predict recurrent myocardial infarction and death (Citation41). However, high-sensitivity assays come with a trade-off of decreased specificity for the diagnosis of myocardial infarction (Citation42).
Troponin elevation especially with high-sensitivity assays may allow us to detect more patients with non-ACS-mediated myocardial ischemia and may identify previously unrecognized underlying coronary artery disease (CAD). Troponin elevation is a measurement of myocardial injury but does not define cause of that injury and therefore should be interpreted based on clinical presentation and pre-test probability of CAD. There is no clear consensus in the literature on an approach and management of these patients. There are currently no guidelines on whether these patients warrant further cardiac investigations (Citation43).
Our systematic review shows that troponin elevation is common in the absence of myocardial infarction, and is associated with a poor prognosis. Further research should focus on developing therapeutic interventions in this population at high risk of adverse outcomes.
Conclusion
Troponin elevation is common in acutely hospitalized patients without a primary cardiac diagnosis and is associated with a statistically significant increase in short-term and long-term mortality.
Supplementary Appendix 2
Download PDF (53.4 KB)Acknowledgements
We would like to thank the following authors for providing further information regarding their study: Mareike Lankeit, MD, from University of Göttingen, Germany; and Austin Ng, MBBS, from University of Sydney, Australia.
Declaration of interest: There was no financial and material support by any organization for this study and there were no potential conflicts of interests for any of the authors. Dr Ahmed had full access to all of the data in the study and takes responsibility for integrity of the data and the accuracy of the data analysis.
References
- Babuin L, Jaffe AS. Troponin: the biomarker of choice for the detection of cardiac injury. CMAJ. 2005;173:1191–202.
- Thygesen K, Alpert JS, White HD. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–95.
- Kehl DW, Iqbal N, Fard A, Kipper BA, De La Parra Landa A, Maisel AS. Biomarkers in acute myocardial injury. Transl Res. 2012;159:252–64.
- White HD. Pathobiology of troponin elevations: do elevations occur with myocardial ischemia as well as necrosis? J Am Coll Cardiol. 2011;57:2406–8.
- De Lemos JA, Drazner MH, Omland T, Ayers CR, Khera A, Rohatgi A, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA. 2010;304:2503–12.
- Weber M, Bazzino O, Navarro Estrada JL, de Miguel R, Salzberg S, Fuselli JJ, et al. Improved diagnostic and prognostic performance of a new high-sensitive troponin T assay in patients with acute coronary syndrome. Am Heart J. 2011;162:81–8.
- Ohman E, Armstrong PW, Christenson RH, Granger CB, Katus HA, Hamm CW, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO II Investigators. N Engl J Med. 1996;335:1333–41.
- Hasaan AK, Bergheanu SC, Hasan-Ali H, Liem SS, van der Laarse A, Wolterbeek R, et al. Usefulness of peak troponin-T to predict infarct size and long-term outcome in patients with first acute myocardial infarction after primary percutaneous coronary intervention. Am J Cardiol. 2009;103:779–84.
- DerSimonian R, Liard N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
- Afonso L, Bandaru H, Rathod A, Badheka A, Ali Kizibash M, Zmily H, et al. Prevalence, determinants, and clinical significance of cardiac troponin-I elevation in individuals admitted for a hypertensive emergency. J Clin Hypertens (Greenwich). 2011;13:551–6.
- Al-Mallah M, Zuberi O, Arida M, Kim H. Positive troponin in diabetic ketoacidosis without evident acute coronary predicts adverse cardiac events. Clin Cardiol. 2008;31:67–71.
- Baillard C, Boussarsar M, Fosse JP, Girou E, Le Toummelin P, Cracco C, et al. Cardiac troponin I in patients with severe exacerbation of chronic obstructive pulmonary disease. Intensive Care Med. 2003; 29:584–9.
- Balasubramaniyam N, Aronow W, Lai H, Palaniswamy C, Lorenzo A, Khera S, et al. Prevalence of increased cardiac troponin I levels in hospitalized patients with pneumonia and in-hospital mortality in patients with increased versus normal cardiac troponin I levels. Open Journal of Cardiology. 2012;3:1.
- Bova C, Crocco F, Ricchio R, Serafini O, Greco F, Noto A. Importance of troponin T for the risk stratification of normotensive patients with pulmonary embolism. A prospective, cohort study with a three-month follow-up. Haematologica. 2005;90423–4.
- Choon-ngram T, Partpisanu P. Serum cardiac troponin-T as a prognostic marker in septic shock. J Med Assoc Thai. 2008;91:1818–21.
- Fadaii A, Sohrabpour H. Serum troponin levels, APACHE II score and mortality rate for non-cardiac reasons in RCU patients. Tanaffos. 2009;8:29–34.
- Giannitsis E, Muller-Bardorff M, Kurowski V, Weidtmann B, Wiegand U, Kampmann M, et al. Independent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolism. Circulation. 2000;102:211–17.
- Hajsadeghi S, Gholami S, Gohardehi G, Moghadam NS, Sabet AS, Kerman SRJ, et al. Association between troponin T and ICU mortality, a changing trend. Cardiovasc J Afr. 2012;23:186–90.
- Hioseth AD, Neukamm A, Karlsson BD, Omland T, Brekke PH, Soyseth V. Elevated high-sensitivity cardiac troponin T is associated with increased mortality after acute exacerbation of chronic obstructive pulmonary disease. Thorax. 2011;66:775–81.
- Janata KM, Leitner JM, Holzer-Richling N, Janata A, Laggner AN, Jilma B. Troponin T predicts in-hospital mortality in patients with pulmonary embolism. Eur Respir J. 2009;34:1357–63.
- Jimenez D, Diaz G, Molina J. Marti D, Del Rey J, Garcia-Rull S, et al. Troponin I and risk stratification of patients with acute nonmassive pulmonary embolism. Eur Respir J. 2008;31:847–53.
- John J, Woodward DB, Wang Y, Yan AB, Fischer D, Kinasewitz GT, et al. Troponin-I as a prognosticator of mortality in severe sepsis patients. J Crit Care. 2010;25:270–5.
- Kalla C, Raveh D, Algur N, Rudensky B, Yinnon AM. Incidence and significance of a positive troponin test in bacteremic patients without acute coronary syndrome. Am J Med. 2008;121:909–15.
- Kelly AM, Kim S. Is elevated troponin associated with in-hospital mortality in emergency department patients admitted with chronic obstructive pulmonary disease? Eur J Emerg Med. 2013;20:54–7.
- Kim HJ, Ham HS, Cho YJ, Kim HC, Lee JD. Usefulness of cardiac troponin I as a prognostic marker in non-cardiac critically ill patients. Tuberculosis and Respiratory Diseases. 2005;59:53–61. [In Korean].
- King DA, Codish S, Novack V, Barski L, Almog Y. The role of cardiac troponin I as a prognosticator in critically ill medical patients: a prospective observational cohort study. Crit Care. 2005;9:390–5.
- Lankeit M, Jimenez D, Kostrubiec M, Dellas C, Hasenfuss G, Pruszcyk P, et al. Predictive value of the high-sensitivity troponin T assay and the simplified pulmonary severity index in hemodynamically stable patients with acute pulmonary embolism: a prospective validation study. Circulation. 2011;124:2716–24.
- Minkin R, Cotiga D, Noack S, Dobrescu A, Homel P, Shapiro JM. Use of admission troponin in critically ill medical patients. J Intensive Care Med. 2005;20:334–8.
- Ng A, Chow V, Yong A, Chung T, Kritharides L. Elevated troponin T predicts both short and long-term mortality after pulmonary embolism. Heart, Lung and Circulation. 2010;19S:S216.
- Palmieri V, Gallotta G, Rendina D, De Bonis S, Russo V, Postiglione A, et al. Troponin I and right ventricular dysfunction for risk assessment in patients with nonmassive pulmonary embolism in the emergency department in combination with clinically based risk score. Intern Emerg Med. 2008;3:131–8.
- Stein R, Gupta B, Agarwal S, Golub J, Bhutani D, Rosman A, et al. Prognostic implications of normal (< 0.10ng/ml) and borderline (0.10 to 1.49ng/ml) troponin elevation levels in critically ill patients without acute coronary syndrome. Am J Cardiol. 2008;102:509–12.
- Tiruvoipati R, Sultana N, Lewis D. Cardiac troponin I does not independently predict mortality in critically ill patients with severe sepsis. Emerg Med Australas. 2012;24:151–8.
- Vasile VC, Babuin L, Rio Perez JA, Alegria JR, Wong Kee Song LM, Chai HS, et al. Long-term prognostic significance of elevated cardiac troponin levels in critically ill patients with acute gastrointestinal bleeding. Crit Care Med. 2009;37:140–7.
- Vasile VC, Chai HS, Khambatta S, Afessa B, Jaffe AS. Significance of elevated cardiac troponin T levels in critically ill patients with acute respiratory disease. Am J Med. 2010;123:1049–58.
- Ver Elst KM, Spapen HD, Nguyen DC, Garbar C, Huyghens LP, Gorus FK. Cardiac troponins I and T are biological markers of left ventricular dysfunction in septic shock. Clin Chem. 2000;46:650–7.
- Wu TT, Yuan A, Chen CY, Chen WJ, Luh KT, Kuo SH, et al. Cardiac troponin I levels are a risk factor for mortality and multiple organ failure in non-cardiac critically ill patients and have an additive effect to the APACHE II score in outcome prediction. Shock. 2004;22: 95–101.
- Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60:1581–98.
- Keller T, Zeller T, Peetz D, Tzikas S, Roth A, Czyz E, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med. 2009;361:868–77.
- Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361:858–67.
- Mills NL, Churchhouse AM, Lee KK, Anand A, Gamble D, Shah AS, et al. Implementation of a sensitive troponin I assay and risk of recurrent myocardial infarction and death in patients with suspected acute coronary syndrome. JAMA. 2011;305:1201–6.
- Daniels LB. Making sense of high sensitivity assays and their role in clinical care. Curr Cardiol Rep. 2014;16:471.
- Newby LK, Jesse RL, Babb JD, Christenson RH, De Fer TM, Diamond GA, et al. ACCF 2012 expert consensus document on practical clinical consideration in the interpretation of troponin elevations: a report of the American College of Cardiology Foundation task force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2012;60:2427–63.