Abstract
Objectives: This study aimed to determine the prevalence of hypertension from repeated blood pressure (BP) measurements, and examine the association between hypertension and obesity, as well as other related risk factors, in a Chinese pediatric population. Methods: A total of 6692 children, aged 3–18 years, were recruited in 2010. Anthropometric measurements and BP were measured using a mercury sphygmomanometer. Those with an elevated BP were screened a second or third time at 2-week intervals. “Hypertension” was defined as elevated BP on all three occasions. A self-administered questionnaire was completed. Results: The prevalence of an elevated BP was 18.2%, 5.1% and 3.1% on the first, second and third visits, respectively. The odds ratios (ORs) and 95% confidence intervals (CIs) for an elevated BP among obese children were 7.07 (5.94–8.42), 17.23 (12.63–23.52) and 20.63 (13.69–31.09), and among those with a paternal history of hypertension were 1.26 (0.98–1.61), 1.35 (0.90–2.02) and 1.80 (1.15–2.81) on each consecutive visit. Conclusions: Repeated measurements are required to confirm the diagnosis of hypertension in children and that obesity and paternal hypertension are strongly associated with pediatric hypertension.
Introduction
Hypertension (HTN) is one of the leading causes of burden of disease worldwide (Citation1). Strategies for the prevention and control of HTN mainly target adults over the long-term (Citation2). Blood pressure (BP), however, tends to track from childhood into adulthood (Citation3). Thus, recognizing the development of HTN at an earlier age may provide physicians with an opportunity to reduce its risk factors early on (Citation4). The promotion of such a strategy, however, requires more evidence-based support that links BP with its associated risk factors in different children populations, particularly in developing countries, where obesity has become an epidemic (Citation5).
Owing to a large variability in repeated BP measurements obtained on a single visit, the diagnosis of HTN in adults is typically based on repeated BP measurements over several visits (Citation6). Similar to adults, it was recently recommended that elevated BP in children should be determined from at least three separate visits (Citation7). Of the studies that have assessed the prevalence of elevated BP in children from more than one visit (Citation8–10), only two population-based studies determined the prevalence of elevated BP based on measurements from three separated occasions. They report that the prevalence of elevated BP was more than halved on the third versus the first visit (Citation9,Citation11). To our knowledge, data on the prevalence of HTN based on BP readings from at least three separate occasions in the Chinese pediatric population is scant. Therefore, the prevalence and risk factors of sustained HTN in the pediatric population are largely unknown.
In the present study, we estimated the prevalence of HTN among 3–18-year-old children and adolescents in Beijing, China based on readings obtained from three separate visits. Furthermore, we assessed the association between HTN and excess body weight, sleep duration, familial history of HTN, parental educational levels and other characteristics of both children and their parents.
Methods
Study population
A total of 6692 consecutive subjects, aged 3–18 years, were enrolled from two urban districts and two rural districts of Beijing, China in 2010 using a stratified cluster sampling technique. In the four districts, nine kindergartens, seven primary schools and five secondary schools at middle level were selected, and at least 400 gender-balanced volunteers in each age group were recruited randomly from the sampling sites above. The study was approved by the ethical research committee of the Capital Institute of Pediatrics. Informed consent was obtained from all subjects and their guardians.
BP measurement and HTN screening procedure
BP was measured according to a standard protocol by trained examiners using a mercury sphygmomanometer in the sitting position (Citation12). After a resting period of at least 15 min, BP was measured on the right upper arm at the level of the heart. The cuff size was determined based on the size of the subject's arm, and covered at least two-thirds of the upper arm. BP was measured three times every visit, and each measurement was separated by at least a 1–2-min interval, during which the right arm was elevated for 5–6 s. If a difference of more than 4 mmHg was obtained between two adjacent BP readings during the same visit, then an additional measurement was obtained. Korotkoff phase 1 (K1) and 4 (K4) sounds were used to define systolic BP (SBP) and diastolic BP (DBP), respectively. Heart rate was recorded in beats/min.
Children with an elevated BP during the first visit were required to return 2 weeks later for a second visit. Similarly, children with an elevated BP during the second visit were required to return 2 weeks later for a third visit. BP measurements obtained from the second and third visits were performed by the same examiners and with the same devices as in the first visit.
Anthropometric measurements
Anthropometric measurements were obtained in a quiet and temperature-controlled room by a team of trained clinical research officers at the initial visit. Standing height (without shoes) was measured twice to the nearest 0.1 cm using a standard stadiometer. Weight (with light clothing) was measured to the nearest 0.1 kg (Citation13). Body mass index (BMI) was calculated as weight divided by the height squared (kg/m2).
Questionnaire
Information on potential risk factors was collected using a self-administered questionnaire, which was completed by both the children and their parents. The questionnaire included questions on puberty status, physical activity, salt intake, sleep habits, familial history of HTN and parental educational levels.
Puberty status was estimated by whether they have menarche for girls and whether they have spermatorrhoea for boys. Insufficient amount of sleep was defined according to the rules and regulations of school health work in China (Citation14,Citation15) as < 10 h/day for children aged 3–7 years, < 9 h/day for those aged 8–11 years and < 8 h/day for those aged 12–18 years. Parental educational levels were ranked according to the following categories: primary (lower than primary school), secondary (primary school to middle school) and tertiary educational level (equal to or above university). Parents were considered to have HTN if they have been diagnosed as HTN by doctors from upper second-class hospital or have been told by a physician or health professional that they have elevated BP and have to take antihypertensive drug regularly to control BP.
Definitions and standards
Elevated BP was defined according to Chinese reference data (Citation16), which is generally considered the best available reference for the Chinese pediatric population. Elevated BP was defined as SBP or DBP in the ≥ 95th sex- and age-specific percentile. “Hypertension” was defined as elevated BP on all three occasions.
Overweight and obesity in school-aged children were defined according to BMI cut-offs for Chinese children and adolescents (Citation17). The US 2000 CDC Growth Chart (CDC2000) was used to clarify the weight status for children aged 3–6 years (Citation18). Specifically, BMI in the < 85th, between the ≥ 85th and < 95th, and in the ≥ 95th percentiles was classified as normal weight, overweight and obese, respectively. Based on the Chinese national survey of students’ physical quality data, we also calculated BMI percentiles (i.e. < 5th, 5th–24th, 25th–49th, 50th–74th, 75th–84th, 85th–94th and ≥ 95th).
Statistical analysis
A covariance analysis adjusted for gender, age and puberty status was used to assess the differences in mean BP and chi-square test was used to compare the prevalence, respectively. Adjusted for gender, age, puberty status and heart rate, a binary-logistic regression model was used to assess the associations between HTN and various characteristics. A composite bar-diagram was used to describe the relationship between BMI and BP. All analyses were conducted in SPSS version 18.0. A p < 0.05 was considered statistically significant.
Results
A total of 6692 (49.7% male) children, aged 3–18 years, participated in the study. Participant characteristics are presented in .
Table I. Characteristics of participants by gender.
The prevalence of elevated BP was 18.2% on the first visit. Among those children with elevated BP on the first visit, 71.2% returned for a second visit (866 of 1217). The reasons for not returning for a second visit included school absenteeism, conflicts with school activities/responsibilities, moved to another city, went to seek medical advice or did not want to participate. There were no systematic differences between the children with elevated BP that were re-screened and those that were not. The prevalence of an elevated BP among children at the second visit was 37.4% (324 of 866). The estimated prevalence of elevated BP following two visits was calculated as follows: the number of children with an elevated BP on the second visit (n = 324) was divided by the total number of children (n = 6341) who had a normal BP at the first visit (n = 5475) plus those that underwent BP measurements on a second visit (n = 866). Using this method, the estimated prevalence of elevated BP following two visits was 5.1% (324 of 6341). Similarly, of the children with an elevated BP on the second visit, 89% had participated in a third visit (287 of 324), and the estimated prevalence of elevated BP following three visits was 3.1% (197 of 6304) ().
The level of SBP, DBP and the prevalence of elevated BP, at three separate visits, are a little higher in urban than that in rural, presented in .
Table II. Mean blood pressure and prevalence at three separate visits by district.
Gender-specific SBP, DBP and the prevalence of elevated BP, at three separate visits, are presented in . There were no significant differences in BP between boys and girls. The prevalence of elevated SBP, elevated DBP and HTN was slightly higher in boys than girls on the first and second visits (p < 0.05). However, there were no significant differences between genders on the third visit. Among the children with elevated BP, 36.7%, 45.7% and 50.3% of them had isolated elevated SBP on the first, second and third visits, respectively, and 38.8%, 17.9% and 14.2% of them had isolated elevated DBP on the three successive visits.
Table III. Mean blood pressure and prevalence at three separate visits by gender.
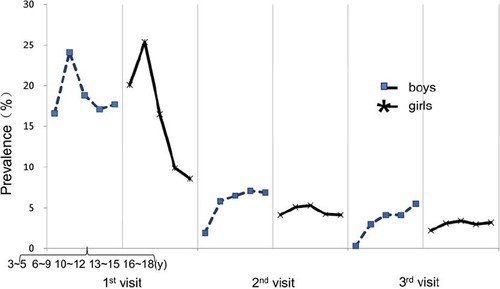
The prevalence of elevated BP was age dependent (). There were 668, 902, 628, 632 and 497 boys, and 637, 899, 673, 646 and 510 girls in 3∼, 6∼, 10∼, 13∼ and 16∼18 age groups participating in the first visit; 616, 832, 612, 594 and 476 boys, and 566, 837, 656, 645 and 507 girls in the five age groups participating in the second visit; and 608, 828, 612, 585 and 474 boys, and 557, 836, 654, 644 and 506 girls in the five age groups participating in the third visit.
The gender-, age-, puberty status- and heart rate-adjusted associations between HTN and selected characteristics of the children and their parents are presented in .
Table IV. Risk factors associated with hypertension in children at three visits.
The prevalence of elevated BP in children on each separate visit and according to BMI percentile categories is presented in . The prevalence of elevated BP increased with increasing BMI percentile categories (based on Chinese national survey of students’ physical quality data (Citation17)).
Discussion
The prevalence of HTN, based on three separate visits with triplicate BP measurements at each visit, among 6692 Chinese children, aged 3–18 years, was 3.1%. It was also found that the prevalence of HTN was age dependent. On the second and third visit, most children with an elevated BP also had an isolated elevated SBP. The prevalence of elevated BP was six-fold lower on the third versus the first visit. In general, HTN in children was associated with overweight and obesity, sleep duration and parental history of HTN, but not with parental educational level, which was self-reported or reported by their parents.
The advantages of the present study are the large sample size and the population-based study design, which ensure that the results are representative of the general population. However, the screening design has some disadvantages that need to be discussed. First, BP was not re-assessed in children with a normal BP on the initial visit, and consequently, this may lead to an underestimation in the prevalence of HTN, especially if certain children had a low BP at that initial visit, but in actuality had a high BP (including masked HTN). One study has shown that, in adults, BP may decrease over subsequent visits in both individuals with high and normal initial BP (Citation19). The perfect design would be to evaluate and diagnose HTN through ambulatory BP monitoring, but this is difficult and is not practical in a population-based survey. However, only a few studies with small sample sizes have explored the effects of masked HTN in youth (Citation20).
Previous studies have also demonstrated a substantial decrease in BP in children when measurements were repeated on separate occasions. In 2007, a Swiss study (Citation21) on 5207 children reported that 11.4% had elevated BP at the initial screening visit, while only 2.2% had persistent elevated BP based on repeated measurements taken on a separate occasion. In an Italian study, 8.8% of 5207 children in the sixth grade were found to have elevated BP, and only 4.2% were still hypertensive when their BP was re-measured some days later (Citation8). Historically, in the USA, the reported prevalence of pediatric HTN has varied greatly depending, in part, on the way in which HTN is defined and number of occasion that BP is measured. In a BP survey of 10 641 children conducted in Dallas in 1979 (Citation22), the prevalence of elevated BP was reported to be 8.9% on the first visit. On the third visit some days later, only 1.2% had systolic HTN and 0.4% had diastolic HTN. Among 2460 adolescents in Houston (Citation11), the prevalence of elevated BP was 16.8%, 11.1% and 9.5% on the first, second and third visits, respectively, in 2002. In another study conducted in 2004 on teenagers in Houston, it was found that the prevalence was 19.4%, 9.5% and 4.5% with each successive visit. Compared with the findings of these studies, the prevalence of elevated BP among school-age children in China is a little higher than that of the children in Switzerland and USA.
In the present study, of the children with elevated BP, 36.7%, 45.7% and 50.3% had an isolated elevated SBP, and 38.8%, 17.9% and 14.2% had an isolated elevated DBP on the first, second and third visits, respectively. In Europe, however, of the children that had an elevated BP, the majority also had an isolated elevated SBP (84%, 84% and 81% on the first, second and third visits, respectively), whereas a few children had an elevated DBP (Citation21). The BP references in USA (Citation7) and Europe (Citation23) use Korotkoff phase 5 sounds to evaluate DBP, whereas the BP reference standards for Chinese children and adolescents (Citation16) use K4. This may explain the differences found in the prevalence of elevated DBP between Europe and China.
The results from the current study also suggest that classifying weight status by normal weight, overweight and obese is somewhat limited. Such an arbitrary classification neglects to capture the continuous relationship between weight status and BP, especially in children. Specifically, it was found that the pre-valence of elevated BP increased with successive increases in BMI percentiles, even within the presumably normal range of BMI. These trends were observed at all three visits. As already known, BMI percentiles and the definition of elevated BP account for normal, gender-specific, age-related increases in BMI and BP, and this trend might reflect a relationship that is independent of normal physical maturation.
The ORs (95% CIs) for elevated BP or HTN were fairly high among overweight and obesity children. This finding suggests that obesity is an independent risk factor of HTN. Almost all of the other similar studies have suggested a similar conclusion. Thus, weight management should be considered a primary therapeutic goal for obesity-related HTN.
HTN is a familial aggregation complex disease, and the association between children and their parental history of HTN has been previously suggested. Familial history is an important variable in the development of prevention strategies and public health practices for metabolic disorders (Citation24). The gender of the parents may also influence the association between parental HTN and HTN in offspring. The current study presented that paternal history of HTN was an independent risk factor of HTN in children, which has been proven consistently, as in one longitudinal study on children with HTN in Australia (Citation25). Additional studies in this field also found that parental or maternal history of HTN may play a more important role in the incidence of HTN in their offspring (Citation26,Citation27). While in the present study there were only 34, 13 and nine children whose mother had HTN, and only 13, six and three children whose both parents had HTN in the first, second and third visits, respectively. The sample of children with parental or maternal history was too small and may lead to low statistical power of test, which may further confuse the analysis and appropriate conclusions. Furthermore, the parents were not old enough to reach the high-risk age for HTN, therefore, many normotensive parents at present may develop HTN in the future. All the above might impair the associations between parental HTN and elevated BP in the offspring.
Conclusion
The prevalence of HTN after three separate visits is 3.1% – only one sixth of that on the first screening in Chinese pediatric population, and repeated measurements are necessary to confirm the diagnosis of HTN in children and adolescents. The current study shows overweight and obesity are risk factors of HTN in children and adolescents and those with paternal HTN are a high-risk population. Healthcare providers should be strong advocates helping to prevent obesity in adolescents and children.
Acknowledgements
The authors wish to thank the participants, as well as the staff from Beijing Centers for Disease Control and Prevention and Beijing Maternal and Child Health Care Hospital.
Conflicts of interest
None.
Sources of funding
This study was supported by grants to M.J. from the Beijing Medical Development Fund (grant 2007-1024), Beijing Health System Leading Talent Fund (grant 2009-1-08), Beijing Training Project for the Leading Talent in S & T (grant 2011LJ07), and a grant to M.L.H. from the Beijing Municipal Health Bureau Youth Fund (grant 2009-23).
References
- Lawes CM, Vander HS, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part 1: Estimates of blood pressure levels. J Hypertens. 2006;24:413–422.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289:2560–2572.
- Labarthe DR. Prevention of cardiovascular risk factors in the first place. Prev Med. 1999;29:S72–S78.
- Fuentes RM, Notkola IL, Shemeikka S, Tuomilehto J, Nissinen A. Tracking of systolic blood pressure during childhood: A 15-year follow-up population-based family study in eastern Finland. J Hypertens. 2002;20:195–202.
- Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: A summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–2013;e144.
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, . Recommendations for blood pressure measurement in humans and experimental animals. Part 1: Blood pressure measurement in humans: A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697–716.
- The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576.
- Genovesi S, Giussani M, Pieruzzi F, Vigorita F, Arcovio C, Cavuto S, . Results of blood pressure screening in a population of school-aged children in the province of Milan: Role of overweight. J Hypertens. 2005;23:493–497.
- Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113:475–482.
- Leung LC, Sung RY, So HK, Wong SN, Lee KW, Lee KP, . Prevalence and risk factors for hypertension in Hong Kong Chinese adolescents: Waist circumference predicts hypertension, exercise decreases risk. Arch Dis Child. 2011; 96:804–809.
- Sorof JM, Poffenbarger T, Franco K, Bernard L, Portman RJ. Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. J Pediatr. 2002;140:660–666.
- Lawes CM, Vander HS, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part 1: Estimates of blood pressure levels. J Hypertens. 2006;24:413–422.
- Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452.
- Chinese State Bureau of Technical Supervision & Ministry of Health P.R. China. Health standard of daily learning time for primary school students.
- Chinese State Bureau of Technical Supervision & Ministry of Health P.R. China. Health standard of daily learning time for secondary school students.
- Mi J, Wang TY, Meng LH, Zhu GJ, Han SM, Zhong Y, . Development of blood pressure reference standards for Chinese children and adolescents. Chin J Evid Based Pediatr. 2010;5:4–14.
- Group of China Obesity Task Force. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Chin J Epidemiol. 2004; 25:97–102.
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–1243.
- Bovet P, Gervasoni JP, Ross AG, Mkamba M, Mtasiwa DM, Lengeler C, . Assessing the prevalence of hypertension in populations: Are we doing it right? J Hypertens. 2003;21: 509–517.
- Lurbe E, Torro I, Alvarez V, Nawrot T, Paya R, Redon J, . Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45:493–498.
- Chiolero A, Cachat F, Burnier M, Paccaud F, Bovet P. Prevalence of hypertension in schoolchildren based on repeated measurements and association with overweight. J Hypertens. 2007;25:2209–2217.
- Fixler DE, Laird WP, Fitzgerald V, Stead S, Adams R. Hypertension screening in schools: Results of the Dallas study. Pediatrics. 1979;63:32–36.
- Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, . Management of high blood pressure in children and adolescents: Recommendations of the European Society of Hypertension. J Hypertens. 2009;27:1719–1742.
- Wada K, Tamakoshi K, Yatsuya H, Otsuka R, Murata C, Zhang H, . Association between parental histories of hypertension, diabetes and dyslipidemia and the clustering of these disorders in offspring. Prev Med. 2006;42:358–363.
- Burke V, Gracey MP, Beilin LJ, Milligan RA. Family history as a predictor of blood pressure in a longitudinal study of Australian children. J Hypertens. 1998;16:269–276.
- Fuentes RM, Notkola IL, Shemeikka S, Tuomilehto J, Nissinen A. Familial aggregation of blood pressure: A population-based family study in eastern Finland. J Hum Hypertens. 2000;14:441–445.
- DeStefano AL, Gavras H, Heard-Costa N, Bursztyn M, Manolis A, Farrer LA, . Maternal component in the familial aggregation of hypertension. Clin Genet. 2001;60:13–21.