Abstract
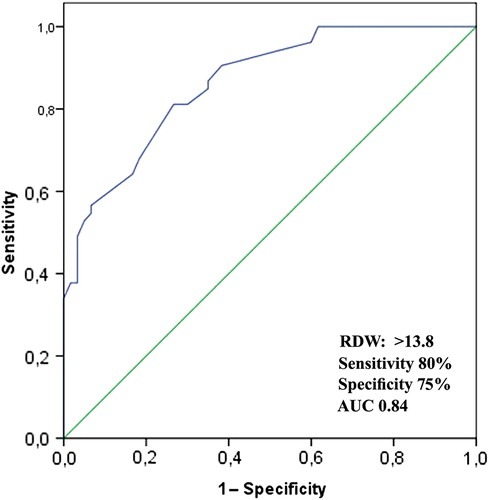
Red cell distribution width (RDW) is independently associated with morbidity and mortality in cardiovascular diseases. RDW is elevated in hypertensive patients compared with normotensives. Based on the nocturnal course, hypertension classified as dipper and non-dipper. Non-dipper hypertension is associated with higher inflammation and worse prognosis. We aimed to investigate whether RDW and high-sensitive C-reactive protein (hsCRP) are elevated in non-dipper hypertensive patients compared with dippers. The study included total 247 essential hypertensive patients. Twenty-four-hour ambulatory blood pressure monitoring (ABPM) was performed for each patient. Thereafter patients were divided into the two groups on the basis of the results of 24-h ABPM: 127 dipper hypertensives and 120 non-dipper hypertensives. Complete blood count and biochemistry were measured by standard methods and hsCRP was assessed by using BN2 model nephelometer. Non-dippers had significantly higher RDW levels than dippers [14.6 (13.8–17.0) vs 13.0 (12.5–13.4), p < 0.001, respectively]. After adjustment for hemoglobin, low-density lipoprotein-cholesterol, sex, age and hs-CRP, mean RDW values were for dipper and non-dippers 13.4 (12.4–13.2) and 14.5 (13.7–16.8), respectively (p < 0.001). RDW was negatively correlated with the percentage decline of systolic and diastolic BP from day to night (r = − 0.392, p < 0.001 and r = − 0.294, p < 0.001, respectively). Serum hsCRP levels were also significantly higher in the non-dippers (p < 0.001) and it was significantly positively correlated with RDW (r = 0.403, p < 0.001). In receiver-operating characteristic curve analysis, the optimal cut-off value of RDW to predict non-dipping pattern was > 13.8%, with 80% sensitivity and 75% specificity. RDW is significantly increased in patients with non-dipper hypertension compared with the dipper hypertension. Inflammatory activity was closely related to RDW in non-dipper hypertensives. RDW, as easy and quick measurable tool, can predict non-dipping pattern in essential hypertension.
Introduction
As a component of the routine blood cell count, red cell distribution width (RDW) is a quantitative measure of variability in the size of circulating erythrocytes and it displays anisocytosis (Citation1). RDW is used not only to differentiate types of anemia but also is a predictor of morbidity and mortality in a variety of settings (Citation2). In many cardiovascular diseases (CVD), RDW has been proposed as a prognostic marker and seems to be related with worse prognosis. The studies investigating RDW in patients with CVD reported that elevated RDW level was associated with adverse outcomes and mortality in patients with stable coronary heart disease (Citation2,Citation3), heart failure (Citation1,Citation4), acute myocardial infarction (Citation5), stroke (Citation6), peripheral artery disease (Citation7) and in patients who underwent primary coronary intervention (Citation8).
RDW is elevated in prehypertensive and hypertensive patients when compared with normotensive subjects (Citation9). It is known that hypertensive individuals can be divided into two groups based on 10% reduction in the nocturnal blood pressure (BP) patterns: dipper and non-dipper hypertensives (Citation10). The latter group carries a higher cardiovascular risk and is connected to greater subclinical target-organ damage compared with dippers (Citation11–13). Hence, early identification of those patients is important, as they are at risk of future adverse cardiovascular events.
Various hematological and inflammatory biomarkers, such as mean platelet volume (MPV) (Citation14), high-sensitive C-reactive protein (hsCRP) (Citation15) and gamma-glutamyl transferase (GGT) (Citation16) have been used in clinical practice to determine non-dipping status in hypertensive patients; however, no study has yet investigated any possible association between circadian BP pattern and RDW. Accordingly, the aim of the present study was to evaluate RDW levels together with the inflammatory response in patients with essential hypertension in terms of circadian BP patterns.
Materials and methods
Study population
The study consisted of 247 consecutive outpatients with primary hypertension who had applied to our clinic. Hypertension was defined as systolic BP (SBP) ≥ 140 mmHg or a diastolic BP (DBP) ≥ 90 mmHg and/or use of the anti-hypertensive drug therapy (Citation17). After diagnosis of hypertension, ambulatory blood pressure monitoring (ABPM) was performed for all patients. Exclusion criteria included secondary hypertension, heart failure, diabetes mellitus, renal or hepatic dysfunction, clinical evidence of cancer, systemic inflammatory disease, hematological system disorder and known coronary artery or cerebrovascular disease. We excluded secondary hypertension by history, physical examination, current laboratory tests (kidney function, potassium and calcium levels, thyroid tests), having resistant hypertension. Most of the study group had been investigated for secondary causes of hypertension previously in our hospital or elsewhere.
The patients’ clinical and demographic characteristics encompassing age, sex, smoking habits and antihypertensive drugs were noted. In addition, serum levels of hsCRP, fasting blood glucose level, creatinine level and fasting serum lipid status including total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL) and triglyceride levels were also recorded. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). The local ethics committee approved the study protocol and informed consent was taken from all patients.
Laboratory tests
All laboratory data were obtained from venous blood samples after 12 h of fasting. Lipid profile, glucose and creatinine were determined by standard methods. Total white blood cell counts, platelet counts, hemoglobin, mean corpuscular volume (MCV) and RDW were calculated using an automated blood cell counter (Siemens, ADVIA 2120i Hematology System, USA). HsCRP levels were assessed by using BN2 model nephelometer (Dade Behring, Cardio Phase hsCRP Assay, Marburg, Germany).
Ambulatory blood pressure monitoring and dipping status
A 24-h ABPM device (Mobilograph, Stolberg, Germany) was applied to each subject. Device was placed around the non-dominant arm and it was worn for 24 h with BP readings every 15-min period in the daytime and every 30-min period at night-time. Daytime and night-time were defined using short, fixed clock intervals, which ranged from 06:00 to 22:00 h and from 22:00 to 06:00 h, respectively. The recordings were analyzed with interactive software. If 20% or more of the measurements could not be taken, those patients were excluded from the study. From the hourly averages of ambulatory BP recordings, daytime, night-time and 24-h averages of SBP, DBP and mean BP were calculated for each patient. Patients with BP decrease of 10% or more during night-time were accepted as dipper hypertensives, whereas patients with BP decreases less than 10% were accepted as non-dipper hypertensives according to the criterion of Verdecchia et al (Citation11).
Statistical analysis
Statistical analysis was performed by using SPSS 15.0 statistical software (SPSS Inc., Chicago, IL, USA). The Kolmogorov–Smirnov test was used to determine whether the continuous variables were normally distributed. Normal distributed variables were given as mean ± SD and non-normally distributed variables were given as medians with interquartile ranges. The chi-square test was used for categorical variables. Mean values of the groups were compared with Student's t-test and Mann–Whitney U test where appropriate. Similarly, Pearson and Spearman correlation coefficients were used to test univariate correlations. Statistical significance was set at p < 0.05.
Results
A total of 247 primary hypertensive patients were enrolled in the study. On the basis of the results of 24-h ABPM, subjects were divided into two groups: 127 dipper patients (mean age; 52 ± 12 years, 63 females and 64 males) and 120 non-dipper patients (mean age; 54 ± 13 years, 66 females and 54 males,). summarizes the baseline demographic and clinical data of two groups.
Table I. Patient characteristics.
Groups were similar with respect to demographic data and antihypertensive drug use. LDL levels of the non-dipper group were found to be higher than the dipper group (126.1 ± 33.9 vs 120.3 ± 35.8, p < 0.05). Hemoglobin levels, white blood cell counts and platelet counts were similar between the groups. Clinical BPs was significantly higher in non-dipper hypertensives than dipper hypertensives (SBP 145.3 ± 11.1 mmHg vs 141.1 ± 9.3 mmHg, DBP 93.8 ± 7.5 mmHg vs 90.3 ± 6.3 mmHg, p < 0.05, respectively). The nocturnal SBP, DBP and mean BPs was also significantly higher in non-dippers compared with dippers ().
Table II. Blood pressure values of dipper and non-dipper groups.
As shown in the , non-dipper patients demonstrated higher levels of RDW compared with dippers [14.6 (13.8–17.0) vs 13.0 (12.5–13.4), p < 0.001, respectively]. After adjustment for hemoglobin, LDL-cholesterol, sex, age and hs-CRP, mean RDW values were for dipper and non-dippers 13.4 (12.4–13.2) and 14.5 (13.7–16.8), respectively (p < 0.001). Moreover, non-dipper patients also had higher hsCRP levels compared with dippers (6.1 ± 2.1 mg/l vs 2.7 ± 1.3 mg/l, p < 0.001, respectively).
Significant positive correlation was observed between RDW and hsCRP levels in non-dipper hypertensive patients (r = 0.403, p < 0.001) ().
Figure 1. The positive correlation between red cell distribution width (RDW) and high-sensitive C-reactive protein (hsCRP).
RDW was negatively correlated with the rate of nocturnal SBP and DBP fall (r =− 0.392, p < 0.001 and r =− 0.294, p < 0.001, respectively) ().
Figure 2. The negative correlation between red cell distribution width (RDW) and nocturnal blood pressure fall. SBP, systolic blood pressure; DBP, diastolic blood pressure.
In hypertensive patients, receiver operating characteristics (ROC) curves explored the relationship between the non-dipping status and RDW. The area under the curve was 0.84 (95% CI 0.80–0.89; p < 0.001). Using a cut-off point of 13.8, the RDW predicted non-dipping status with a sensitivity of 80% and specificity of 75% ().
Discussion
The current data demonstrate that RDW was significantly increased in patients with non-dipper hypertension compared with those of dipper hypertension. Increased RDW levels were found to be strongly related with lack of night-time SBP and DBP falls. RDW > 13.8 measured in hypertensive patients had an 80% sensitivity and 75% specificity in predicting non-dipping pattern.
Hypertension is a well-established and important risk factor for the development of CVD, stroke and renal failure (Citation18). Traditionally, the diagnosis of hypertension is made based on properly measured office BP readings after the clinical assessment (Citation19). Beyond the several BP measurements made in the clinic, 24-h ABPM can provide much information about hypertension, such as the average BP level, BP variability and the diurnal variation (Citation20). In hypertensive individuals, lack of adequate reduction in night-time BP is associated with higher cardiovascular risk and worse prognosis (Citation11,Citation13). Although the underlying causative mechanisms responsible for lack of nocturnal decline in BP have still yet to be completely elucidated, previous studies established that non-dippers are older, obese, and have poorer sleep quality, autonomic dysfunction and high sympathetic activity (Citation21–24). In addition, non-dipper hypertensive patients tend also to have increased inflammatory activity. The association between non-dipper hypertension and inflammation has been reported in various studies conducted on different inflammatory markers, such as hsCRP (Citation14,Citation15), GGT (Citation16) and uric acid (Citation25).
The correlation between RDW and hypertension has been established in many studies. Tanindi et al. (Citation9) found that in patient with prehypertension and hypertension RDW was significantly higher than healthy subjects. Wen (Citation26) found that there was close relationship between RDW levels and carotid artery atherosclerosis in patients with hypertension. In two large community-based cohort studies, researchers reported that increased RDW levels were associated with higher BP levels (Citation3,Citation27). In this study, we tried to determine whether any possible association between circadian BP patterns and RDW levels existed in essential hypertension. Our results suggest that RDW is strongly associated with non-dipping status in essential hypertension. We also found that the percentage decline in BP from day to night was negatively correlated with RDW levels.
Elevated RDW is strongly and independently associated with adverse outcomes in CVD and thus it is proposed as a novel predictor of mortality (Citation1–7). The possible explanation of the relationship between RDW and CVD is the presence of chronic inflammation (Citation28). Chronic inflammation may cause RDW elevation and increased RDW levels might reflect an underlying chronic inflammation, which would result in an increased risk of CVD (Citation1). Indeed, further investigations confirmed this hypothesis. In a study of 3845 adult outpatient subjects, Lippi et al. (Citation29) demonstrated that there was strong, graded and independent association between RDW and hsCRP levels. Lappe et al. (Citation2) found that RDW was associated with mortality (correlating with hsCRP levels) in patients with coronary artery disease. Semba et al. (Citation30) investigated whether serum antioxidants and inflammation predicted RDW values in older women. The patients in higher quartile of RDW were more likely to have a higher interleukin-6 level. Forhecz et al. (Citation31) found that RDW was associated with mortality and inflammation in patients with chronic heart failure. Our results are parallel to those previous studies and we demonstrated that RDW is strongly associated with hsCRP in non-dipper hypertensive patients. Although hsCRP is known to predict non-dipping pattern in hypertensive patients, to our knowledge, our study will be the first to report on a correlation between RDW and hsCRP in patients with hypertension.
In hypertensive patients, early identification of non-dipping pattern is important for protecting patients against deleterious effects of relatively higher night-time BP levels. For this reason, easy, quick and reliable tools may help physicians adjust medical treatment and identify patients who need more close monitoring in order to prevent cardiovascular adverse outcomes. The aforementioned correlations between RDW and inflammation may help understand why this marker is associated with non-dipping status in hypertension. Complete blood count is the most widely available laboratory data in the initial evaluation of hypertensive patients and RDW can thus be easily obtained to identify patients who are prone to night-time non-dipping BP.
Study limitations
The primary limitations of our study were that it had a cross-sectional design and that it represented a single-center experience. Non-dipper hypertensive patients were not followed-up in terms of future adverse cardiovascular events. Although we demonstrated a significant association between elevated RDW and non-dipping pattern, we could not determine the exact mechanism of this association.
Conclusion
The recent study demonstrated that RDW is a useful marker in predicting inadequate reduction in night-time BP in essential hypertension. RDW values are closely related with inflammation in non-dipper hypertensive patients.
Declaration of interest: The authors declared no conflict of interest. The authors alone are responsible for the content and writing of the paper.
References
- Felker GM, Allen LA, Pocock SJ, Shaw LK, McMurray JJ, Pfeffer MA, . Red cell distribution width as a novel prognostic marker in heart failure: Data from the charm program and the duke databank. J Am Coll Cardiol. 2007;50:40–47.
- Lappe JM, Horne BD, Shah SH, May HT, Muhlestein JB, Lappe DL, . Red cell distribution width, c-reactive protein, the complete blood count, and mortality in patients with coronary disease and a normal comparison population. Clin Chim Acta. 2011;412:2094–2099.
- Tonelli M, Sacks F, Arnold M, Moye L, Davis B, Pfeffer M. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation. 2008;117:163–168.
- Zalawadiya SK, Zmily H, Farah J, Daifallah S, Ali O, Ghali JK. Red cell distribution width and mortality in predominantly African-American population with decompensated heart failure. J Cardiac Failure. 2011;17:292–298.
- Dabbah S, Hammerman H, Markiewicz W, Aronson D. Relation between red cell distribution width and clinical outcomes after acute myocardial infarction. Am J Cardiol. 2010;105:312–317.
- Ani C, Ovbiagele B. Elevated red blood cell distribution width predicts mortality in persons with known stroke. J Neurol Sci. 2009;277:103–108.
- Ye Z, Smith C, Kullo IJ. Usefulness of red cell distribution width to predict mortality in patients with peripheral artery disease. Am J Cardiol. 2011;107:1241–1245.
- Karabulut A, Uyarel H, Uzunlar B, Cakmak M. Elevated red cell distribution width level predicts worse postinterventional thrombolysis in myocardial infarction flow reflecting abnormal reperfusion in acute myocardial infarction treated with a primary coronary intervention. Coronary Artery Dis. 2012; 23:68–72.
- Tanindi A, Topal FE, Topal F, Celik B. Red cell distribution width in patients with prehypertension and hypertension. Blood Press. 2012;21:177–178.
- O’Brien E, Sheridan J, O’Malley K. Dippers and non-dippers. Lancet. 1988;2:397.
- Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, . Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801.
- Pickering TG. The clinical significance of diurnal blood pressure variations. Dippers and non-dippers. Circulation. 1990;81:700–702.
- Izzedine H, Launay-Vacher V, Deray G. Abnormal blood pressure circadian rhythm: A target organ damage?Int J Cardiol. 2006;107:343–349.
- Inanc T, Kaya MG, Yarlioglues M, Ardic I, Ozdogru I, Dogan A, . The mean platelet volume in patients with non-dipper hypertension compared to dippers and normotensives. Blood Press. 2010;19:81–85.
- Kaya MG, Yarlioglues M, Gunebakmaz O, Gunturk E, Inanc T, Dogan A, . Platelet activation and inflammatory response in patients with non-dipper hypertension. Atherosclerosis. 2010;209:278–282.
- Ermis N, Yagmur J, Acikgoz N, Cansel M, Cuglan B, Pekdemir H, . Serum gamma-glutamyl transferase (GGT) levels and inflammatory activity in patients with non-dipper hypertension. Clin Exp Hypertens. 2011 Jul 28. [Epub ahead of print].
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., .The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–2572.
- Kannel WB. Blood pressure as a cardiovascular risk factor: Prevention and treatment. JAMA. 1996;275:1571–1576.
- Ogedegbe G, Pickering T. Principles and techniques of blood pressure measurement. Cardiol Clin. 2010;28:571–586.
- Kanbay M, Turkmen K, Ecder T, Covic A. Ambulatory blood pressure monitoring: From old concepts to novel insights. Int Urol Nephrol. 2012;44:173–182.
- de la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M, . Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466–472.
- Mann S, Altman DG, Raftery EB, Bannister R. Circadian variation of blood pressure in autonomic failure. Circulation. 1983;68:477–483.
- Sherwood A, Steffen PR, Blumenthal JA, Kuhn C, Hinderliter AL. Nighttime blood pressure dipping: The role of the sympathetic nervous system. Am J Hypertens. 2002;15:111–118.
- Sherwood A, Routledge FS, Wohlgemuth WK, Hinderliter AL, Kuhn CM, Blumenthal JA. Blood pressure dipping: Ethnicity, sleep quality, and sympathetic nervous system activity. Am J Hypertens. 2011;24:982–988.
- Erden M, Kocaman SA, Poyraz F, Topal S, Sahinarslan A, Boyaci B, . Incremental effects of serum uric acid levels, autonomic dysfunction, and low-grade inflammation on nocturnal blood pressure in untreated hypertensive patients and normotensive individuals. Turk Kardiyoloji Dernegi arsivi: Turk Kardiyoloji Derneginin yayin organidir. 2011;39: 531–539.
- Wen Y. High red blood cell distribution width is closely associated with risk of carotid artery atherosclerosis in patients with hypertension. Exp Clin Cardiol. 2010;15:37–40.
- Perlstein TS, Weuve J, Pfeffer MA, Beckman JA. Red blood cell distribution width and mortality risk in a community-based prospective cohort. Arch Inter Med. 2009;169: 588–594.
- Lappé JM, Horne BD, Shah SH, May HT, Muhlestein JB, Lappé DL, . Red cell distribution width, C-reactive protein, the complete blood count, and mortality in patients with coronary disease and a normal comparison population. Clin Chim Acta. 2011;412:2094–2099 [Epub 2011 Jul 27].
- Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, Guidi GC. Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Arch Pathol Lab Med. 2009;133:628–632.
- Semba RD, Patel KV, Ferrucci L, Sun K, Roy CN, Guralnik JM, . Serum antioxidants and inflammation predict red cell distribution width in older women: The Women's Health and Aging Study I. Clin Nutr. 2010;29:600–604.
- Forhecz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohaszka Z, Janoskuti L. Red cell distribution width in heart failure: Prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am Heart J. 2009;158:659–666.