Abstract
Aim: To determine the prevalence of left atrial (LA) enlargement and its relation to left ventricular (LV) diastolic dysfunction among asymptomatic diabetic outpatients attending Muhimbili National Hospital in Dar es Salaam, Tanzania. Methods: Echocardiography was performed in 122 type 2 and 58 type 1 diabetic patients. Diastolic dysfunction was defined as peak transmitral blood velocity to medial mitral annulus velocity (E/E’) ratio ≥ 15. LA volume indexed to body surface area (LAVI) was considered enlarged if ≥ 29 ml/m2. Results: Enlarged LAVI and LV diastolic dysfunction were more common in type 2 than in type 1 diabetic patients (44.3 vs 25.9% and 20.5 vs 3.5%, respectively, both p < 0.05). In multivariate linear regression analysis, larger LAVI was associated with LV diastolic dysfunction independent of significant associations with LV mass index and presence of mitral regurgitation in type 2 diabetic patients, while LV mass index, lower ejection fraction and longer duration of diabetes were the main covariates of larger LAVI in type 1 diabetic patients (all p < 0.05). Conclusion: Enlarged LA is common among asymptomatic Tanzanian diabetic patients, and particularly associated with LV diastolic dysfunction in type 2, and with cardiomyopathy and lower systolic function in type 1 diabetic patients.
Introduction
Although left atrial (LA) enlargement is a common marker of subclinical cardiac target organ damage both in diabetic and hypertensive patients (Citation1), LA size also reflects the severity of left ventricular (LV) diastolic dysfunction independent of other well-known covariates of LA enlargement including hypertension, obesity and age (Citation2–5). In particular, LA volume, which better reflects LV filling pressure over time (Citation6), has been suggested to be a better marker of LV diastolic dysfunction and cardiovascular risk than mitral inflow Doppler indices, which reflect instant LV filling pressures at the time of the examination (Citation3,Citation4,Citation7).
In diabetic patients, LV diastolic dysfunction is common, reported in about 30–60% of cases in studies from Europe and North America (Citation8–11), but data from African populations is scarce. In a recent publication from South Africa, isolated diastolic dysfunction was found as the only echocardiographic pathology in 23% of patients admitted with heart failure (Citation12). However, less is known about the prevalence of LA enlargement and how well it reflects LV diastolic dysfunction in asymptomatic diabetic patients in sub-Saharan Africa. Thus, the aim of this study was to determine the prevalence and covariates of enlarged LA volume among type 1 and type 2 diabetic patients attending Muhimbili National Hospital in Dar es Salaam, Tanzania.
Materials and methods
Patient population
Participants for this study were recruited from diabetic patients who participated in a survey to determine prevalence of microalbuminuria among type 1 and type 2 diabetic patients attending Muhimbili National Hospital in Dar es Salaam, Tanzania in 2003–4 (Citation13). Of the total 244 patients in this previously published survey, 184 patients who were still receiving care and treatment at the diabetic outpatient clinic at the hospital in 2008 were invited to participate in the present study. All 184 patients agreed to participate and signed informed consent. The study received ethical approval from the Muhimbili University of Health's Research and Publications Committee.
Among the 184 patients recruited, LA volume could not be measured in four patients due to poor apical window, and these were excluded from the present analysis.
Clinical assessment and Laboratory tests
A structured questionnaire was used for interview about socio-demographic characteristics, history of cardiovascular risk factors and the duration of diabetes. Height and weight were measured and used to calculate body mass index. Waist circumference was measured at the level of the umbilicus and used as a measure of central obesity. Blood pressure was measured using a mercury sphygmomanometer and appropriate cuff size following the joint European Society of Hypertension and European Society of Cardiology guidelines (Citation14). After a 5-min rest in the sitting position, a set of three readings were done 5 min apart. The average of the last two readings was taken as the patient's clinic blood pressure. Hypertension was defined as blood pressure ≥ 140/90 mmHg or use of antihypertensive medications.
Serum glucose, HbA1c, lipids and creatinine were measured in fasting blood samples. Urinary albumin/creatinine ratio (UACR) was measured in a spot morning urine sample. Abnormal albuminuria was defined as UACR > 30 mg/g (Citation15).
Echocardiography
All echocardiograms were performed by the same licensed cardiologist (PC) who had received special training in echocardiography using a SONOS 7500 Phillips echocardiograph. Patients were examined in left lateral decubitus position using a 3-MHz transducer following a standardized protocol. All images were recorded digitally on Magnetic Optical disks, and interpretation of all digital echocardiograms was done at the Department of Heart Disease, Haukeland University Hospital using a Tomtec (TomTech Imaging Systems GmbH, Unterschleissheim, Germany) workstation for post-processing. All studies were first read by the primary investigator and then proof-read by the senior investigator, a highly experienced reader (EG).
Assessment of cardiac structure
Quantitative echocardiography was performed following the joint European Association of Echocardiography and American Society of Echocardiography guidelines (Citation16). LV mass was calculated using an autopsy validated equation (Citation17) and indexed to height2.7 to obtain LV mass index (LVMI). LV hypertrophy was considered present if LVMI exceeded 49.2 g/m2.7 in men and 46.7 g/m2.7 in women (Citation18). LA volume was measured using biplane Simpson's method at the end of LV systole and indexed to body surface area (LAVI). LAVI was considered enlarged if ≥ 29 ml/m2 (Citation16). Assessment of mitral valve regurgitation was done using colour Doppler imaging and graded 1–4 (Citation19).
Assessment of LV diastolic function
LV filling was recorded at the level of the mitral leaflets tips. The leading edge of the mitral flow pattern was traced to derive peak early (E) and atrial (A) velocities, E/A ratio and E deceleration time. Isovolumic relaxation time was measured from the leading edge of the aortic valve closure spike to the leading edge of the mitral valve opening spike. The medial early diastolic mitral annular velocity (E’) was measured by spectral tissue Doppler imaging in apical four-chamber view. The ratio of E to E’ velocity (E/E’ ratio) was taken as an estimation of LV filling pressure (Citation20) and diastolic dysfunction was defined as E/E’ ≥ 15 (Citation21).
Statistical methods
Data management and statistical analysis was performed using SPSS for Windows version 18.0. Data is presented as mean ± standard deviation for continuous variables and as percentages for categorical variables. Groups of patients were compared using χ2 test, unpaired Student's t-test and general linear model adjusting for age and gender with Sidak's post hoc test as appropriate. Bivariate correlations were assessed by Pearson's correlation coefficients. Uni- and multivariate linear and logistic regression analyses were used to identify covariates of enlarged LAVI in the total study population and separately in groups of patients with type 1 and type 2 diabetes. Results are presented as beta coefficients and significant level for the linear models and as odds ratios (OR) and 95% confidence intervals (CI) for the logistic models. Finally, the ability of LAVI to detect diastolic dysfunction was tested in receiver operating characteristic (ROC) curve analysis of probabilities derived from the multivariate models reporting area under the curve (AUC) and 95% CI. ROC curves were compared using DeLong's test (Citation22). A two-tailed p-value of ≤ 0.05 was considered statistically significant.
Results
Patients’ characteristics
The study population included 58 type 1 and 122 type 2 diabetic patients. Seven patients (3.9%) had LV ejection fraction < 50% (1 type 1 and 6 type 2 diabetic patients). Compared with type 1, type 2 diabetic patients were older (55 ± 9 vs 21 ± 10 years), had longer duration of diabetes (11 ± 6 vs 8 ± 4 years) and were more likely to be obese (37% vs 2%) and have hypertension (82% vs 17%), all p < 0.01. Grade 1 mitral regurgitation was present in 25.6% patients and grade 2 in 1.7% in the total study population, and more common among patients with enlarged LAVI independent of type of diabetes. Severe mitral regurgitation was not found in any patient. All type 1 diabetic patients were on insulin treatment, while among type 2 diabetic patients, 77.9% were on oral hypoglycaemic drugs, 20.5% were on insulin and 1.6% on diet alone.
Prevalence and correlates of larger LAVI
In the total population, enlarged LAVI was present in 38.3% and was more common among type 2 diabetic patients (44.3% vs 25.9%, respectively, p < 0.05). Patients with enlarged LAVI were older when compared with patients with normal LAVI both among type 1 (26.9 vs 18.7 years) and type 2 (56.8 vs 53.1 years) diabetic groups (both p < 0.05). There was no gender difference in patients with and without enlarged LAVI in both type 1 (53% vs 51% women) and type 2 (61% vs 66% women), p > 0.05 for both.
Enlarged LAVI was more common in patients with hypertension and in patients with increased E/E’ ratio reflecting LV diastolic dysfunction, particularly among type 2 diabetic patients (). In comparisons adjusted for sex and age, patients with type 1 diabetes and enlarged LAVI showed a trend towards longer diabetes duration, and had lower estimated GFR (). Among type 2 diabetic patients, those with larger LAVI had significantly higher pulse pressure ().
Table I. Demographic characteristics and laboratory findings in type 1 and type 2 diabetic patients divided into groups with normal and enlarged left atrium volume indexed to body surface area (LAVI).
Figure 1. Prevalence of increased left atrium volume index (LAVI) in different subgroups of patients: (Citation1) normotensive patients (NT) with normal peak early transmitral jet velocity to mitral annulus velocity ratio (E/E’), (Citation2) hypertensive patients (HT) with normal E/E’ and (Citation3) patients with increased E/E’ (presence of left ventricular diastolic dysfunction) according to type of diabetes.
The most important echocardiographic difference between patients with enlarged LAVI and those with normal LAVI was larger LV mass index and higher prevalence of LV hypertrophy both among type 1 and type 2 diabetic patients (). In addition, the E/E’ ratio was significantly higher in patients with type 2 diabetes and enlarged LAVI (). In bivariate correlations, larger LAVI was significantly associated with higher systolic blood pressure, mean blood pressure, serum creatinine, LV mass index as well as higher E/E’ ratio, both in type 1 and type 2 diabetic patients (). Use of anti-diabetic treatment did not correlate with LAVI.
Table II. Echocardiographic findings in type 1 and type 2 diabetic patients divided into groups with normal and increased left atrium volume index (LAVI).
Table III. Correlates of larger left atrium volume index (LAVI) in the total population and in groups of patients with type 1 and type 2 diabetes.
LAVI in relation to LV diastolic dysfunction
In the total population, LV diastolic dysfunction (defined as E/E’ ratio ≥ 15) was present in 15.1% of patients. Diastolic dysfunction was more common in type 2 than in type 1 diabetic patients (20.5% vs 3.5%, p < 0.01). The E/E’ ratio correlated positively with increasing LAVI in univariate analysis, both in type 2 and in type 1 diabetic patients although the correlation coefficient was higher in the type 2 diabetic patients ().
Figure 1. Relationship between left atrium volume index (LAVI) and peak early transmitral jet velocity to mitral annulus velocity ratio (E/E’) in type 1 and type 2 diabetic patients.
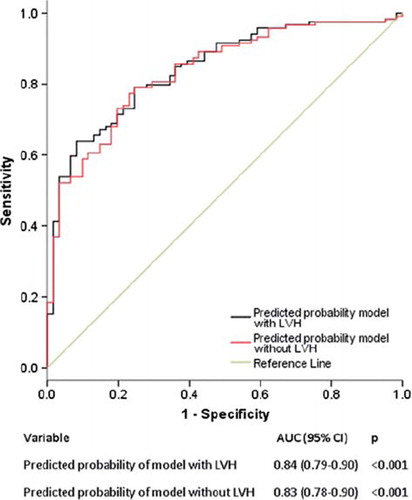
Multivariate linear regression analysis in the type 2 diabetic group demonstrated that larger LAVI was associated with having LV diastolic dysfunction independent of LV mass index and presence of mitral regurgitation, while no significant association was found with LV ejection fraction, age, systolic blood pressure, poorer glycaemic control or presence of obesity (). Using the same model, LV mass index and lower ejection fraction were the main covariates of larger LAVI in type 1 diabetic patients (). Adding duration of diabetes as a covariate in the model revealed an independent association between longer duration of diabetes (β = 0.27, p < 0.05) and larger LAVI among type 1 diabetic patients, irrespective of significant association with LV mass index (β = 0.36) and lower ejection fraction (β = −0.37, both p < 0.01). Converting the multivariate linear model into a multivariate logistic regression model, enlarged LAVI was associated with a 3.3 times higher prevalence of LV diastolic dysfunction (OR = 3.28 [95% CI 1.19–8.99], p = 0.021) in the overall population independent of LV hypertrophy (OR = 2.5 [95% CI 1.15–5.45], p = 0.021), type 2 diabetes (OR = 1.23 [95% CI 0.5–3.05], p = 0.648) and hypertension (OR = 1.2 [95% CI 0.50–2.98], p = 0.670). Plotting the overall probability of this model with and without inclusion of LV hypertrophy among the covariates in a ROC curve demonstrated that the association of larger LAVI with presence of LV diastolic dysfunction was independent of presence of LV hypertrophy ().
Table IV. Independent predictors of left atrium volume index (LAVI) in type 1 and type 2 diabetic patient groups identified in multivariate linear regression analyses.
Figure 1. Enlarged left atrium volume index (LAVI) was associated with left ventricular (LV) diastolic dysfunction independent of presence of LV hypertrophy. Receiver operating characteristic (ROC) curve showing predicted probability of the multivariate logistic regression model with and without LV hypertrophy in the model.
Discussion
To our knowledge, the present study is the first to demonstrate that enlarged LA is a common finding in asymptomatic diabetic patients in sub-Saharan Africa, and particularly associated with presence of LV diastolic dysfunction in type 2 diabetic patients, while LA enlargement more reflects LV systolic dysfunction and diabetic cardiomyopathy development in type 1 diabetic patients. Previous studies in Europe and North America have demonstrated that LV diastolic dysfunction is common in diabetic patients (Citation8–11). Our finding that subclinical LV diastolic dysfunction was common in asymptomatic type 2 diabetic patients, but rare in asymptomatic type 1 diabetic patients (present in 20.5% and 3.5%, respectively), adds to a publication from the Heart of Soweto study in South Africa which found that isolated diastolic dysfunction was the sole echocardiographic abnormality in 23% of Africans admitted with symptomatic heart failure (Citation12). The six-fold higher prevalence of LV diastolic dysfunction among type 2 diabetic patients reflects the higher prevalence of factors predisposing to diastolic dysfunction in this group, like older age and more hypertension, obesity and LV hypertrophy. The lower prevalence of diastolic dysfunction in our study compared with reports from Europe (Citation9–11) and North America (Citation8) probably reflects differences in definitions of diastolic dysfunction used. In fact our definition of diastolic dysfunction of E/E’ ratio ≥ 15 identifies patients who have at least moderate diastolic dysfunction with increased LA pressure (Citation21).
The well-known confounders of enlarged LAVI identified in previous studies, like hypertension, LV hypertrophy and reduced LV ejection fraction were all identified also in the present study population, although the effect of blood pressure diminished when LV mass was added to multivariate analyses, as also reported by others (Citation23). As demonstrated by the results, LAVI was particularly associated with LV diastolic dysfunction in type 2 diabetic patients, but increased progressively with increasing E/E’ ratio in both type 1 and type 2 diabetic patients in concordance with previous findings in the North American population of Olmstead County (Citation3,Citation4). Although higher systolic blood pressure was associated with enlarged LAVI among both type 1 and type 2 diabetic patients in univariate analysis, higher systolic blood pressure did not independently predict LAVI in multivariate analysis. Furthermore, in ROC curve analysis, LAVI was associated with presence of LV diastolic dysfunction independent of presence of LV hypertrophy.
Among type 1 diabetic patients, LAVI did not independently predict LV diastolic dysfunction. The lack of independent association between LAVI and diastolic dysfunction in the type 1 group could be explained by the fact that only 3.5% of patients in this group had diastolic dysfunction according to our definition. Instead, among the type 1 diabetic patients, duration of diabetes and lower systolic function were more predictive of larger LAVI than diastolic dysfunction. These findings are in line with the well known progression from diastolic dysfunction to diabetic cardiomyopathy associated with type 1 diabetes (Citation24). The finding that duration of diabetes predicted enlarged LAVI in type 1 diabetes adds to a previous report demonstrating that longer duration of type 1 diabetes was associated with LV diastolic dysfunction (Citation25).
Of note, obesity was not an independent predictor of larger LAVI in our study, contrary to findings from previous studies in hypertensive populations in Caucasians and African Americans (Citation2,Citation23). However, body mass index and waist circumference both correlated positively with LAVI in univariate analysis in the total population.
Conflicting results have been reported on the impact of poor diabetes control and presence of LV diastolic dysfunction (Citation25–28). In the present study, larger LAVI correlated negatively with HbA1c, indicating that as LAVI increased patients had better glycaemic control. However, overall diabetes control was poor in our study, and did not independently influence presence of LV diastolic dysfunction or LAVI in the multivariate analyses.
Study limitations
There is limited knowledge on LV function in native sub-Saharan African diabetic population. Although this study did not include a healthy control group or deformation analysis, it adds to current knowledge of prevalence and covariates of LAVI as a reflector of presence of LV diastolic dysfunction in asymptomatic sub-Saharan African diabetic patients. The cross-sectional design precludes any claim of causal relationship. There were also a limited number of diabetic patient in this study by design. However, this study gives new information on LV diastolic dysfunction in asymptomatic diabetic patients seen in an outpatient clinic at a tertiary hospital in Tanzania.
From studies in Western societies, it is well known that subclinical coronary artery disease is more common in diabetic patients and associated with systolic dysfunction and heart failure. The present study did not include any systematic testing of presence of coronary artery disease, but none of the patients had known clinical cardiovascular disease or symptoms.
Conclusion
In the present echocardiographic study of asymptomatic diabetic patients receiving outpatient care at the Muhimbili National Hospital in Dar-es-Salaam in Tanzania, enlarged LAVI was more common among type 2 than among type 1 diabetic patients. Larger LAVI particularly reflected presence of LV diastolic dysfunction in type 2 diabetic patients, while in type 1 diabetic patients larger LAVI was associated with lower LV systolic function and diabetes cardiomyopathy. Further studies are needed to determine whether LAVI may be used as a simple predictor of risk for incident symptomatic heart failure in such patients.
Declaration of interests
The authors report no conflict of interest.
References
- Gerdts E, Wachtell K, Omvik P, Otterstad JE, Oikarinen L, Boman K, . Left atrial size and risk of major cardiovascular events during antihypertensive treatment: Losartan intervention for endpoint reduction in hypertension trial. Hypertension. 2007;49:311–316.
- Gerdts E, Oikarinen L, Palmieri V, Otterstad JE, Wachtell K, Boman K, . Correlates of left atrial size in hypertensive patients with left ventricular hypertrophy: The Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) Study. Hypertension. 2002;39:739–743.
- Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left atrial volume as a morphophysiologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002 Dec;90:1284–1289.
- Pritchett AM, Mahoney DW, Jacobsen SJ, Rodeheffer RJ, Karon BL, Redfield MM. Diastolic dysfunction and left atrial volume: A population-based study. J Am Coll Cardiol. 2005;45:87–92.
- Piotrowski G, Banach M, Gerdts E, Mikhailidis DP, Hannam S, Gawor R, . Left atrial size in hypertension and stroke. J Hypertens. 2011;29:1988–1993.
- Moya-Mur JL, Garcia-Martin A, Garcia-Lledo A, Ruiz-Leria S, Jimenez-Nacher JJ, Megias-Sanz A, . Indexed left atrial volume is a more sensitive indicator of filling pressures and left heart function than is anteroposterior left atrial diameter. Echocardiography. 2010;27:1049–1055.
- Cuspidi CNF, Sala, C. Valerio, C. Mancia, G. Association of left atrial enlargement with left ventricular hypertrophy and diastolic dysfunction: A tissue Doppler study in echocardiographic practice. Blood Press. 2012;21:24–30.
- Zabalgoitia M, Ismaeil MF, Anderson L, Maklady FA. Prevalence of diastolic dysfunction in normotensive, asymptomatic patients with well-controlled type 2 diabetes mellitus. Am J Cardiol. 2001;87:320–323.
- Poulsen MK, Henriksen JE, Dahl J, Johansen A, Gerke O, Vach W, . Left ventricular diastolic function in type 2 diabetes mellitus: Prevalence and association with myocardial and vascular disease. Circ Cardiovasc Imaging. 2010; 3:24–31.
- Giorda CB, Cioffi G, de Simone G, Di Lenarda A, Faggiano P, Latini R, . Predictors of early-stage left ventricular dysfunction in type 2 diabetes: Results of DYDA study. Eur J Cardiovasc Prev Rehabil. 2011;18:415–423.
- Raev DC. Which left ventricular function is impaired earlier in the evolution of diabetic cardiomyopathy? An echocardiographic study of young type I diabetic patients.Diabetes Care. 1994;17:633–639.
- Stewart S, Wilkinson D, Hansen C, Vaghela V, Mvungi R, McMurray J, . Predominance of heart failure in the Heart of Soweto Study cohort: Emerging challenges for urban African communities. Circulation. 2008;118:2360–2367.
- Lutale JJ, Thordarson H, Abbas ZG, Vetvik K. Microalbuminuria among Type 1 and Type 2 diabetic patients of African origin in Dar Es Salaam, Tanzania. BMC Nephrol. 2007; 8:2.
- Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, . 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–1187.
- Jensen JS, Clausen P, Borch-Johnsen K, Jensen G, Feldt-Rasmussen B. Detecting microalbuminuria by urinary albumin/creatinine concentration ratio. Nephrol Dial Transplant. 1997;12:6–9.
- Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, . Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7:79–108.
- Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, . Echocardiographic assessment of left ventricular hypertrophy: Comparison to necropsy findings. Am J Cardiol. 1986;57:450–458.
- de Simone G, Izzo R, Chinali M, De Marco M, Casalnuovo G, Rozza F, . Does information on systolic and diastolic function improve prediction of a cardiovascular event by left ventricular hypertrophy in arterial hypertension?Hypertension. 2010;56:99–104.
- Jones EC, Devereux RB, Roman MJ, Liu JE, Fishman D, Lee ET, . Prevalence and correlates of mitral regurgitation in a population-based sample (the Strong Heart Study). Am J Cardiol. 2001;87:298–304.
- Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. Doppler tissue imaging: A noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30:1527–1533.
- Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, . Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–1794.
- DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics. 1988;44:837–845.
- Gottdiener JS, Reda DJ, Williams DW, Materson BJ. Left atrial size in hypertensive men: Influence of obesity, race and age. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. J Am Coll Cardiol. 1997;29: 651–658.
- van Heerebeek L, Hamdani N, Handoko ML, Falcao-Pires I, Musters RJ, Kupreishvili K, . Diastolic stiffness of the failing diabetic heart: Importance of fibrosis, advanced glycation end products, and myocyte resting tension. Circulation. 2008;117:43–51.
- Gul K, Celebi AS, Kacmaz F, Ozcan OC, Ustun I, Berker D, . Tissue Doppler imaging must be performed to detect early left ventricular dysfunction in patients with type 1 diabetes mellitus. Eur J Echocardiogr. 2009;10:841–846.
- Suys BE, Katier N, Rooman RP, Matthys D, Op De Beeck L, Du Caju MV, . Female children and adolescents with type 1 diabetes have more pronounced early echocardiographic signs of diabetic cardiomyopathy. Diabetes Care. 2004;27:1947–1953.
- Sartore G, Piarulli F, Ragazzi E, Burlina S, Chilelli NC, Sarais C, . Subclinical diastolic dysfunction in type 2 diabetic patients with and without carotid atherosclerosis: Relationship with glyco-oxidation, lipid-oxidation and antioxidant status. Int J Cardiol. 2011 Jun 20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21696838
- Fraser GE, Luke R, Thompson S, Smith H, Carter S, Sharpe N. Comparison of echocardiographic variables between type I diabetics and normal controls. Am J Cardiol. 1995;75: 141–145.
