Abstract
Hypertension is the most prevalent, treatable cause of cardiovascular (CV) disease. Patients with hypertension and one or more comorbidities increasingly form a significant part of the primary care practitioner's caseload. The emphasis on intensive blood pressure (BP) lowering has softened, encouraging any degree of BP lowering, since any fall in BP is beneficial for reducing CV risk. Consistency of BP control during long-term therapy (i.e. low visit-to-visit variability) and decreasing BP variability over 24-h may be as, if not more, important than degree of BP lowering per se. Fluctuations in BP between visits as well as within a 24-h period have been associated with increased CV risk. Ambulatory BP monitoring (ABPM) is a crucial element of the clinician's armamentarium not only for assessing the “true” BP load and fluctuations under real-life conditions but for identification of various abnormal BP patterns that may require attention, including white- coat hypertension, masked hypertension, non-dipping and the morning BP surge. ABPM provides accurate assessment of treatment effectiveness over 24-h and may lead to better tailoring of therapy. This article reviews the benefits of ABPM and discusses the importance of selecting long-acting antihypertensive agents for optimizing BP control.
Introduction
Hypertension is one of the strongest prognostic markers for cardiovascular (CV) disease (Citation1). Moreover, hypertension is extremely prevalent, estimated to affect up to 15–20% of adults, increasing to 30–40% in the elderly. Most primary-care physicians will already be caring for many patients with hypertension, including those with complicating comorbidities, and this will increase dramatically in the near future with the ageing population. Hence, tackling hypertension effectively is imperative. In addition to increasing the likelihood of coronary heart disease by threefold, hypertension is the most prevalent, important and modifiable risk factor for stroke – more than half of the global burden of stroke is attributable to high blood pressure (BP) (Citation2,Citation3). Thus, the costs to society and health service providers of poorly managed hypertension are substantial (Citation4).
The landscape of hypertension treatment is changing. BP variability has assumed increasing importance in the diagnosis and management of hypertension (Citation5), as indicated by the increasing use of ambulatory BP monitoring (ABPM). Measuring BP over 24-h has not only resulted in more accurate diagnosis of hypertension but has also changed how antihypertensive effectiveness is defined (Citation6). Antihypertensive agents that provide durable, consistent lowering across the 24-h dosing period and particularly drugs that are able to “smooth out” undesirable BP fluctuations, are now favoured (Citation7,Citation8). In addition, consistency and durability of BP control over the long-term has emerged as a major contributor to CV disease reduction by antihypertensive therapy (Citation9). The purpose of this review is to present the latest evidence regarding BP targets, the effects of BP variability on CV risk, and the aims of good BP control by therapy during follow-up. The advantages offered by employing ABPM in everyday practice are discussed within the context of optimizing BP management.
ABPM benefits and BP targets
Originally considered an investigational tool when introduced, ABPM is now increasingly employed in clinical practice, as it is widely recognized that ABPM provides more reliable BP measurements and gives better prediction of organ damage and the risks of CV complications compared with clinic BP measurement (Citation10–12). ABPM is able to provide more information on the full and “true” 24-h BP load than clinic BP measurement alone, since at least 50 measurements are carried out under ambulatory (i.e. “real-life”) conditions. This has been recognized in the most recent update to the UK's National Institute for Health and Clinical Excellence (NICE) treatment guidelines that recommend the use of ABPM to confirm a diagnosis of hypertension after measurement of clinic BP (Citation13). Unfortunately, the guidelines did not include a recommendation to measure BP over a full 24-h period that would provide valuable information on BP variability and night-time BP.
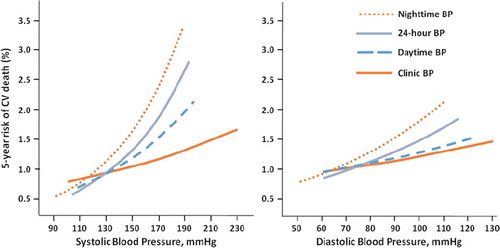
In treated hypertensive patients, higher mean 24-h BP by ABPM predicts CV events independently of clinic BP or other CV risk factors (Citation10) and has been shown to be superior to clinic BP measures in predicting CV mortality, especially when night-time values are considered () (Citation11).
Figure 1. The relative predictive power of different blood pressure measurements for 5-year risk of cardiovascular death (Citation11). Reproduced with permission from Dolan et al. (Citation11).
The use of ABPM may improve the accuracy of diagnosis of hypertension, identify patterns of episodic hypertension (such as white-coat hypertension) and facilitate more appropriate treatment targeting (Citation12). Nonetheless, while there is clear guidance for BP targets based upon clinic BP measurement, there are as yet no evidence-based targets for ABPM alone. Guidelines from the European Society of Hypertension (ESH) and European Society of Cardiology (ESC) offer BP thresholds for the definition of hypertension using different types of measurement (), which may be regarded as approximate threshold values (Citation1). These values are based upon population studies and meta-analyses, and ABPM thresholds are usually several mmHg lower than clinic BP measurement, e.g. clinic BP of 140/90 mmHg corresponds to an average 24-h BP value of 125–130/80 mmHg () (Citation1,Citation14–16). In a recent population-based study, the diagnostic threshold and target clinic BP was slightly lower than clinic values by 10/5 mmHg for 24-h BP and by 6/3 mmHg for daytime measurements (Citation17).
Table I. Approximate blood pressure threshold values for definition of hypertension with different types of measurement: guidelines of the European Society of Hypertension and European Society of Cardiology (Citation1).
ABPM provides detailed information over a 24-h period, including circadian fluctuations and differences between daytime and night-time BP (). ABPM, but not clinic BP, can identify patients with masked hypertension, who may have a poor CV prognosis despite apparently well-controlled BP in the clinic (Citation18,Citation19). Moreover, ABPM can differentiate between true resistant hypertension and white-coat effect in patients with uncontrolled resistant hypertension (Citation20). Thus, in the case of white-coat effect, ABPM may prevent premature switching or stepping-up of therapy, and in masked hypertension help to assess the true BP load on the CV system.
Figure 2. Twenty-four-hour ambulatory blood pressure measurement showing a typical dip in night-time blood pressure and a rise in early morning blood pressure (Citation53). Reproduced with permission from Kario et al. (Citation53).
Another advantage to ABPM is that it allows the collection of additional information over a 24-h period, such as heart rate (Citation21,Citation22). The average heart rate at day and night, and heart rate variability (e.g. standard deviation of average 24-h, daytime or night-time heart rate) can be easily collected by ABPM. Repeatedly it has been shown that elevated heart rate has pathophysiological and prognostic implications. Furthermore, it has been shown that ambulatory heart rate adds prognostic information beyond that of other ABPM predictors (Citation21). Heart rate measures during sleep, and in particular the absence of dipping of heart rate to sleep levels, were independently associated with all-cause mortality (Citation21).
Increasing recognition of the value of ABPM has led to a surge in the number of devices available. An accurate device is fundamental to all BP measurements and choice of equipment should be based on independent validation from national and international societies (Citation23–25) rather than manufacturer claims. In addition to device accuracy, other factors to consider include choice of software and ease of use, presentation and analysis of data, as well as financial considerations (Citation23,Citation26).
Identifying white-coat and masked hypertension
White-coat hypertension is defined as an elevated clinic BP reading (≥ 140/90 mmHg) while daytime or 24-h BP readings are within their normal ranges (< 135/85 mmHg or < 130/80 mmHg, respectively) () (Citation1). It is present in around 15% of the general population and accounts for around one-third of patients in whom hypertension is diagnosed (Citation1). White-coat hypertension is more common in women, the elderly and patients with mild hypertension (Citation27). The prognostic significance of white-coat hypertension has been reported in different studies and remains equivocal. Whilst CV risk was not significantly different between patients with white-coat hypertension and normotensive subjects in a recent meta-analysis (Citation28), it cannot be assumed to be a benign condition (Citation29). In elderly patients, for example, white-coat hypertension has been associated with cardiac abnormalities, namely left ventricular hypertrophy, closer to those seen in patients with sustained hypertension than in normotensive subjects (Citation30).
Table II. Classifications of hypertension that may be differentially diagnosed with ambulatory blood pressure monitoring (ABPM) versus clinic blood pressure (BP) measurement.
Diagnosing masked hypertension is much more challenging than white-coat hypertension, because it would be impractical to use ABPM on every patient with apparently normal clinic BP. Declining organ function in the presence of apparently well-controlled BP by clinic assessment should prompt further evaluation by out-of-clinic measurement (Citation31), and masked hypertension should also be considered more likely in untreated patients with normal clinic BP and CV risk factors such as kidney disease or diabetes (Citation19).
White-coat hypertension should be distinguished from the “white-coat effect”, which is observed in many hypertensive patients, whereby the clinic BP is disproportionately greater than the average daytime ABPM but their ambulatory BP averages are in a hypertensive range. Patients diagnosed with severe hypertension by clinic BP may in fact only have mild hypertension on ABPM due to a marked white-coat effect (Citation32). When patients from a large European disease registry who had recorded resistant hypertension were monitored by ABPM, only 62.5% were classified as having true resistant hypertension – the remaining 37.5% had white- coat effect and controlled hypertension (Citation20).
Conversely, patients with masked hypertension have a normal clinic BP (< 140/90 mmHg) and elevated daytime or 24-h BP readings (≥ 130–135/ 85 mmHg or ≥ 125–130/80 mmHg, respectively) () (Citation1). The prevalence of masked hypertension varies according to the studied population but is approximately 15% (Citation33). Unlike white-coat hypertension, the CV risks associated with masked hypertension have been reported more consistently to be increased (Citation28,Citation34–36) and masked hypertension has been associated with increased risk of CV disease (Citation37). In an observational, non-interventional study of more than 4000 treated hypertensive patients, half were controlled according to clinic BP measurements but nearly two-thirds revealed masked hypertension (R.E. Schmieder et al., unpublished data), indicating lack of effective antihypertensive therapy in a substantial proportion of patients.
Identifying variability in 24-h BP
Several specific patterns of BP variability with negative prognostic implications for CV risk have been widely reported. ABPM provides a powerful tool for establishing and analysing BP variability, which is increased in patients with hypertension and associated with target organ damage and CV risk (Citation6,Citation38).
Non-dipping and extreme dipping
The normal circadian rhythm of BP includes a nocturnal decrease of 10–20% compared with daytime values () (Citation39). Elevated nocturnal BP has been shown to be better associated with CV target organ damage and outcomes compared with a non-dipping BP pattern (Citation40). Non-dipping status refers to a specific pattern, whereby normal falls in BP during sleep are attenuated (nocturnal BP fall < 10%). Various other permutations have been described including extreme dipping (nocturnal BP fall > 20%), dipping (“normal” falls in nocturnal BP) and reverse dipping (night-time elevated BP) (Citation41). Only ABPM allows evaluation of dipping status, particularly non-dipping, which has been reported as being a negative prognostic indicator for CV outcomes (Citation41–43). Hypertensive patients who are non-dippers have been found to have higher left ventricular mass, a marker of poorer CV prognosis (Citation44), and the systolic component of non-dipping has been identified as being a key determinant of target organ damage in untreated hypertensive patients (Citation45). Likewise, in a Japanese study, non-dipping and extreme dipping are associated with an increased risk of cerebrovascular damage (Citation46).
The characteristic “non-dipping” profile of night-time BP in patients with true resistant hypertension may, in part, be a consequence of inadequate 24-h BP control by some antihypertensive agents (Citation47). The presence of obstructive sleep apnoea may also result in a marked increase in BP and heart rate as a result of increased sympathetic tone and vasoconstriction, thus contributing to a non-dipping pattern and CV consequences (Citation48). The close association between obstructive sleep apnoea and hypertension has important implications for CV prevention and treatment. Continuous positive airway pressure (CPAP) comprises the most common treatment procedure for patients with obstructive sleep apnoea, leading to marked reductions in sympathetic activity and blunting of BP surges during sleep (Citation48).
Night-time BP (especially systolic) is identified as the most significant predictor of CV event-free survival compared with the predictive value of daytime values; however, the underlying pathogenesis of this relationship is not a simple one and is poorly understood (Citation49,Citation50). In a large study of ABPM monitoring in patients with untreated hypertension or temporarily off-medication, night-time BP was demonstrated to be the most important predictor of CV mortality () (Citation11). In another study examining blunted heart rate dip during sleep in a cohort of 3957 patients, the absence of heart rate slowing (non-dipping) during sleep was also independently associated with all-cause mortality (Citation21).
Morning BP surge
It is widely accepted that CV events occur most frequently in the morning but attempts to relate the normal waking rise in BP () to the risk of CV events have been frustrated somewhat by varying definitions and inconsistent design and findings between studies. There is a premise that exaggerated upward changes in BP are indicative of an increased CV risk, as shown by a recent meta- analysis (Citation51). However, in one study the morning surge in BP was associated with decreased mortality in non-dipping hypertensive patients, most of whom were on treatment (Citation52). This is interesting as it suggests that non-dipping falsifies the determination of morning surge and the relation between CV risk and morning surge is lost. In another study in elderly hypertensive patients, a higher morning BP surge was associated with stroke risk independently of nocturnal dipping status and “extreme dippers” had a higher incidence of stroke during morning hours (Citation53,Citation54). It is possible, therefore, that the magnitude of the differential between night-time and morning BP is a critical determining factor; this is supported by a study that found an increased risk of stroke in those individuals from a younger, mixed population of patients who had a large night-time fall in BP or a large morning surge (Citation55).
Optimizing 24-h BP control
Rather than a blanket approach that classifies all hypertensive patients as equal according to their BP, today's thinking encourages us to view each patient as an individual, and to approach their management according to their specific CV risk factors (Citation1,Citation56). We know that even relatively modest reductions in BP can have a significantly beneficial impact on CV risk regardless of baseline BP or whether the patient has pre-existing CV disease (Citation57). We also know that BP targets are seldom achieved in practice or even in clinical trials, especially in high-risk patients. Furthermore, consistency of BP control emerged as a key determinant of reducing CV risk by BP lowering medication (Citation9). In addition, BP variability within 24-h is emerging as another key determinant of CV risk, independently of “absolute” BP values.
It is becoming clear that clinic measurement of BP is inadequate for diagnosing and monitoring hypertension during therapy. ABPM over 24-h is rapidly becoming the gold standard for evaluating and managing patients with hypertension, specifically for assessing BP variability and the prognostic value of BP at different times of the day or night, i.e. beyond obtaining just overall 24-h BP values (Citation35,Citation58). Therefore, pragmatically there are some principles of treatment we should adopt in daily clinical practice.
Sustained, consistent antihypertensive effectiveness is widely accepted as being important for good BP control, since 24-h BP is much more closely correlated with CV outcomes than clinic readings (Citation59). However, average measures may miss intermittent BP surges that are damaging to end organs, and may under- or over-estimate treatment efficacy. In particular, BP control that lasts throughout the early morning hours is desirable to address the risks associated with a morning BP surge (Citation60). It has been suggested to administer at least one antihypertensive medication at night-time, rather than the usual timing of administration in the morning, thus addressing the need for improved BP control throughout the night-time and early morning waking hours. In a prospective study of the Spanish hypertensive population, patients taking medication at bedtime showed lower mean sleep-time BP and a reduced prevalence of non-dipping compared with patients taking medication upon awakening. Furthermore, evening administration was associated with a higher prevalence of controlled ambulatory BP and a significantly lower risk of total CV disease events (Citation38). An alternative approach may be to use antihypertensive agents with BP lowering effects that last for at least 24-h and to administer short-acting agents on top of these at bedtime. This approach may be particularly suited to non-dipping patients.
Morning surge and loss of night-time BP fall are both mediated partly by the renin–angiotensin– aldosterone system, supporting agents that effectively target this pathway as a rational treatment choice in all patients with hypertension. Newer ARBs also provide sustained BP control over 24-h, covering the vulnerable early morning hours and last 4–6 h of the dosing period. There are many benefits of agents with once-daily administration, including improved adherence; however, not all once-daily drugs provide consistent BP control throughout the dosing interval. Agents that have a trough:peak plasma ratio ≥ 50 are more effective at controlling 24-h BP while maintaining natural circadian patterns (Citation61). An intrinsically long-acting pharmacological effect rather than an effect solely dependent on formulation is crucial for true 24-h consistent BP control (Citation59).
Recently, an added advantage has been suggested for long-acting antihypertensive agents that have a slower “off rate” (the speed at which efficacy is lost after doses are missed); for these agents, a clinically relevant loss of effectiveness (correlated to an increased CV risk) only occurs with very poor adherence (approximately half of all doses are missed/not taken as prescribed) (Citation62). This means that in the “real world” where patients are not perfect and sometimes forget to take their medication, prescribing an intrinsically long-acting agent can go some way towards mitigating against this eventuality. We should look for effective 24-h BP control for all our hypertensive patients.
Summary and conclusions
Increasingly, 24-h BP has emerged as an important predictor of CV risk and various patterns of BP variability are now recognized as risk factors (Citation63). Notably, BP instability and damaging excesses can persist even when mean systolic BP is apparently well-controlled (Citation7). Certain patterns predict increased CV risk more reliably than others, especially masked hypertension and night-time elevated BP, although white-coat hypertension and morning surge are by no means benign (Citation30,Citation34,Citation40,Citation49,Citation51). ABPM over 24-h is a better predictor of CV events and mortality than clinic readings (Citation10,Citation11). ABPM also improves the accuracy of diagnosis by identifying intermittent symptoms such as white-coat hypertension and therefore enables more appropriate targeting of treatment (Citation12). ABPM can differentiate between sustained and white-coat hypertension in untreated patients, and between resistant and white-coat hypertension in patients on treatment (Citation20), as well as between controlled and uncontrolled hypertension, preventing premature treatment switching. ABPM is being used more often now to evaluate the true effectiveness of antihypertensive treatment over 24-h; sustained, consistent BP control is necessary for optimal effectiveness.
Since good 24-h BP control is important, especially in high-risk patients who are more likely to have a non-dipping status (Citation64), the ability of an antihypertensive agent to “smooth out” undesirable excessive BP variability throughout a 24-h period is becoming a key driver of treatment selection (Citation65). Differences can exist even within a single drug class; for instance, long-acting ARBs are more effective at smoothing 24-h BP than their shorter- acting counterparts (Citation8). Treatments that reduce early morning surge and night-time elevated BP are especially important; agents that target the renin–angiotensin–aldosterone system and which have a long intrinsic duration of action would be a rational treatment choice either alone or as part of a multi-drug regimen.
Acknowledgements
Takeda Pharmaceuticals Europe Ltd has provided an educational grant to support the production of this manuscript, including provision of editorial support by Virgo HEALTH. Takeda Pharmaceuticals Europe Ltd had no control over the article's content at any stage.
Conflicts of interest and source of funding: Professor Schmieder received grants, consultancy and lecture fees from Takeda. Marina Lehmann and Stephanie Schmidt have no conflicts of interest.
References
- Mancia G, De BG, Dominiczak A, Cifkova R, Fagard R, Germano G, . 2007 ESH-ESC Practice guidelines for the management of arterial hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens 2007;25:1751–1762.
- Mancia G, Grassi G. Management of essential hypertension. Br Med Bull 2010;94:189–199.
- Saini M, Shuaib A. Blood pressure lowering and stroke. Expert Rev Neurother 2010;10:225–241.
- Paramore LC, Halpern MT, Lapuerta P, Hurley JS, Frost FJ, Fairchild DG, . Impact of poorly controlled hypertension on healthcare resource utilization and cost. Am J Manag Care 2001;7:389–398.
- Oparil S. Hypertension in2010: New challenges in blood pressure goals and assessment.Nat Rev Cardiol.2011;8: 73–75.
- Parati G, Faini A, Valentini M. Blood pressure variability: Its measurement and significance in hypertension. Curr Hypertens Rep 2006;8:199–204.
- Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet 2010;375:938–948.
- Mancia G, Parati G. Importance of smooth and sustained blood pressure control in preventing cardiovascular morbidity and mortality. Blood Press Suppl 2001;10(Suppl 3):26–32.
- Mancia G, Schumacher H, Redon J, Verdecchia P, Schmieder R, Jennings G, . Blood pressure targets recommended by guidelines and incidence of cardiovascular and renal events in the Ongoing Telmisartan Alone and in Combination With Ramipril Global Endpoint Trial (ONTARGET). Circulation 2011;124:1727–1736.
- Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, . Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med 2003;348:2407–2415.
- Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, . Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: The Dublin outcome study. Hypertension 2005;46:156–161.
- Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FD, Deeks JJ, . Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: Systematic review. BMJ 2011;342:d3621.
- National Institute for Health and Clinical Excellence. Hypertension: The clinical management of primary hypertension in adults. 2011 [cited 2011 Jan 10]; Available from: http://www.nice.org.uk/nicemedia/live/13561/56007/56007.pdf
- Ohkubo T, Imai Y, Tsuji I, Nagai K, Ito S, Satoh H, . Reference values for 24-hour ambulatory blood pressure monitoring based on a prognostic criterion: The Ohasama Study. Hypertension 1998;32:255–259.
- Staessen JA, Fagard RH, Lijnen PJ, Thijs L, Van HR, Amery AK. Mean and range of the ambulatory pressure in normotensive subjects from a meta-analysis of 23 studies. Am J Cardiol 1991;67:723–727.
- Mancia G, Sega R, Bravi C, De VG, Valagussa F, Cesana G, . Ambulatory blood pressure normality: Results from the PAMELA study. J Hypertens 1995;13(12 Pt 1):1377–1390.
- Head GA, Mihailidou AS, Duggan KA, Beilin LJ, Berry N, Brown MA, . Definition of ambulatory blood pressure targets for diagnosis and treatment of hypertension in relation to clinic blood pressure: Prospective cohort study. BMJ 2010;340:c1104.
- Bobrie G, Clerson P, Menard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: A systematic review. J Hypertens 2008;26:1715–1725.
- Papadopoulos DP, Makris TK. Masked hypertension definition, impact, outcomes: A critical review. J Clin Hypertens (Greenwich) 2007;9:956–963.
- de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, . Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension 2011;57:898–902.
- Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Blunted heart rate dip during sleep and all-cause mortality. Arch Intern Med 2007;167:2116–2121.
- Parati G, Bilo G. Should 24-h ambulatory blood pressure monitoring be done in every patient with diabetes?Diabetes Care 2009;32 Suppl 2:S298–S304.
- O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, . European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 2003;21:821–848.
- O’Brien E, Atkins N, Stergiou G, Karpettas N, Parati G, Asmar R, . European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit 2010;15:23–38.
- O’Brien E, Coats A, Owens P, Petrie J, Padfield PL, Littler WA, . Use and interpretation of ambulatory blood pressure monitoring: Recommendations of the British hypertension society. BMJ 2000;320:1128–1134.
- O’Brien E. Twenty-four-hour ambulatory blood pressure measurement in clinical practice and research: A critical review of a technique in need of implementation. J Intern Med 2011;269:478–495.
- Chrysant SG. Treatment of white-coat hypertension. Curr Hypertens Rep 2000;2:412–417.
- Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: An updated meta analysis. Am J Hypertens 2011;24:52–58.
- Dawes MG, Bartlett G, Coats AJ, Juszczak E. Comparing the effects of white-coat hypertension and sustained hypertension on mortality in a UK primary care setting. Ann Fam Med 2008;6:390–396.
- Puchades R, Ruiz-Nodar JM, Blanco F, Rodriguez F, Gabriel R, Suarez C. White-coat hypertension in the elderly. Echocardiographic analysis. A substudy of the EPICARDIAN project. Rev Esp Cardiol 2010;63:1377–1381.
- Messerli FH, Cotiga D. Masked hypertension and white- coat hypertension: Therapeutic navigation between scylla and charybdis. J Am Coll Cardiol 2005;46:516–517.
- Kim SG. Clinical implications of ambulatory and home blood pressure monitoring. Korean Circ J 2010;40:423–431.
- Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006;47:846–853.
- Ogedegbe G, Agyemang C, Ravenell JE. Masked hypertension: Evidence of the need to treat. Curr Hypertens Rep 2010;12:349–355.
- Stolarz-Skrzypek K, Thijs L, Richart T, Li Y, Hansen TW, Boggia J, . Blood pressure variability in relation to outcome in the International Database of Ambulatory blood pressure in relation to Cardiovascular Outcome. Hypertens Res 2010;33:757–766.
- Bjorklund K, Lind L, Zethelius B, Andren B, Lithell H. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation 2003;107:1297–1302.
- Kabutoya T, Ishikawa J, Hoshide S, Eguchi K, Ishikawa S, Shimada K, . Determinants of negative white-coat effect in treated hypertensive patients: The Jichi Morning Hypertension Research (J-MORE) study. Am J Hypertens 2009;22:35–40.
- Hermida RC, Ayala DE, Mojon A, Fernandez JR. Influence of circadian time of hypertension treatment on cardiovascular risk: Results of the MAPEC study. Chronobiol Int 2010;27: 1629–1651.
- Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benemio G, Boldrini F, . Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation 1990;81:528–536.
- Tsioufis C, Andrikou I, Thomopoulos C, Syrseloudis D, Stergiou G, Stefanadis C. Increased nighttime blood pressure or nondipping profile for prediction of cardiovascular outcomes. J Hum Hypertens 2011;25:281–293.
- Ivanovic BA, Tadic MV, Celic VP. To dip or not to dip? The unique relationship between different blood pressure patterns and cardiac function and structure. J Hum Hypertens 2011 Sep 8. doi:10.1038/jhh.2011.83
- Cuspidi C, Sala C, Valerio C, Negri F, Mancia G. Nocturnal blood pressure in untreated essential hypertensives. Blood Press 2011;20:335–341.
- Omboni S, Parati G, Palatini P, Vanasia A, Muiesan ML, Cuspidi C, . Reproducibility and clinical value of nocturnal hypotension: Prospective evidence from the SAMPLE study. Study on Ambulatory Monitoring of Pressure and Lisinopril Evaluation. J Hypertens 1998;16: 733–738.
- Kim BK, Lim YH, Lee HT, Lee JU, Kim KS, Kim SG, . Non-dipper pattern is a determinant of the inappropriateness of left ventricular mass in essential hypertensive patients. Korean Circ J 2011;41:191–197.
- Syrseloudis D, Tsioufis C, Aragiannis D, Soulis D, Stefanadi E, Spanos A, . The dominant role of the systolic component of nondipping status on target-organ damage in never-treated hypertensives. Am J Hypertens 2011;24: 292–298.
- Kario K, Matsuo T, Kobayashi H, Imiya M, Matsuo M, Shimada K. Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension 1996;27:130–135.
- Syrseloudis D, Andrikou I, Andrikou E, Dimitriadis K, Stefanadis C. Ambulatory blood pressure monitoring in resistant hypertension. Int J Hypertens 2011;2011:285612.
- Wolf J, Hering D, Narkiewicz K. Non-dipping pattern of hypertension and obstructive sleep apnea syndrome. Hypertens Res 2010;33:867–871.
- Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension 2011;57:3–10.
- Hermida RC, Ayala DE, Mojon A, Fernandez JR. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol 2011;58:1165–1173.
- Li Y, Thijs L, Hansen TW, Kikuya M, Boggia J, Richart T, . Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension 2010;55:1040–1048.
- Israel S, Israel A, Ben-Dov IZ, Bursztyn M. The morning blood pressure surge and all-cause mortality in patients referred for ambulatory blood pressure monitoring. Am J Hypertens 2011;24:796–801.
- Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, . Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: A prospective study. Circulation 2003;107: 1401–1406.
- Kario K, Yano Y, Matsuo T, Hoshide S, Eguchi K, Shimada K. Additional impact of morning haemostatic risk factors and morning blood pressure surge on stroke risk in older Japanese hypertensive patients. Eur Heart J 2011;32: 574–580.
- Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, . Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: The Ohasama study. Hypertension 2006;47:149–154.
- Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, . Reappraisal of European guidelines on hypertension management: A European Society of Hypertension Task Force document. J Hypertens 2009;27:2121–2158.
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665.
- Iqbal P, Stevenson L. Cardiovascular outcomes in patients with normal and abnormal 24-hour ambulatory blood pressure monitoring. Int J Hypertens 2010;2011:786912.
- Elliott HL. 24-Hour blood pressure control: Its relevance to cardiovascular outcomes and the importance of long-acting antihypertensive drugs. J Hum Hypertens 2004;18:539–543.
- White WB. Importance of blood pressure control over a 24-hour period. J Manag Care Pharm 2007;13(8 Suppl B): 34–39.
- Neutel JM. The importance of 24-h blood pressure control. Blood Press Monit 2001;6:9–16.
- Lowy A, Munk VC, Ong SH, Burnier M, Vrijens B, Tousset EP, . Effects on blood pressure and cardiovascular risk of variations in patients’ adherence to prescribed antihypertensive drugs: Role of duration of drug action. Int J Clin Pract 2011;65:41–53.
- Oparil S, Kjeldsen SE, Narkiewicz K, Hedner T. Blood pressure variability: Emerging role in risk assessment and therapeutics. Blood Press 2010;19:209–211.
- Schmieder RE, Ruilope LM. Blood pressure control in patients with comorbidities. J Clin Hypertens (Greenwich) 2008;10:624–631.
- Parati G, Schumacher H, Bilo G, Mancia G. Evaluating 24-h antihypertensive efficacy by the smoothness index: A meta-analysis of an ambulatory blood pressure monitoring database. J Hypertens 2010;28:2177–2183.
