Abstract
Objectives. The goal of our study was to estimate the impact of abnormal night-time blood pressure (BP) on cardiovascular (CV) mortality in hypertensive patients with significant atherosclerosis established in coronary angiography. Method. We enrolled 891 patients, 63.7 ± 9.4 years of age. They were divided into patients with normal daytime BP values, and patients with abnormal daytime BP values. During a follow-up period of 4.7 years in total, all-cause mortality and both CV and non-CV mortality were assessed. Results. In the group with normal daytime BP, a clinic BP value ≥ 140/90 mmHg was observed in 25.7% (n = 161) of patients, and a night-time BP value ≥ 120/70 mmHg was observed in 37.8% (n = 236) of patients. In the group of patients with normal daytime BP in comparison with those with abnormal daytime BP, there was lower CV mortality (5.6% vs 9.8%, p < 0.02). Abnormal daytime BP was associated with a hazard ratio of CV mortality of 1.80 (95% CI 1.08–3.00, p < 0.02), and abnormal night-time BP with a hazard ratio of 1.63 (95% CI 1.03–2.66, p < 0.04). Conclusion. Assessment of both daytime and night-time BP is essential and superior over clinic BP in CV risk evaluation in patients with coronary artery disease confirmed in coronary angiography.
Introduction
High blood pressure (BP) is a key risk factor in the development of coronary atherosclerosis related to cardiovascular (CV) mortality. In August 2011, the National Institute for Health and Clinical Excellence (NICE) published a new edition of guidelines on clinical management of primary hypertension in adults (Citation1). The most significant novelty was the recommendation to use ambulatory BP monitoring (ABPM) to confirm a hypertension diagnosis established with traditional clinic BP measurements. According to these guidelines, only waking-hour measurements should be used for the diagnosis of hypertension. However, limiting ABPM to waking hours only is bound to miss important information about night-time BP values and to underestimate the degree of night-time high BP (Citation1–6). Published in 2007, Guidelines for the Management of Arterial Hypertension proposed a night-time BP threshold for the definition of hypertension with ABPM of 120/70 mmHg (Citation7). Some studies have indicated that high night-time BP is an independent factor in the development of large-artery atherosclerosis. Studies using ultrasonography and magnetic resonance imaging have shown a relationship between high night-time BP values and atherosclerosis (Citation8,Citation9). It is possible that high night-time BP causes significant damage not only to the large-sized arteries but also to the coronary arterial structures, and thereby contributes to a higher incidence of acute CV events. Therefore, the main goal of our study was to estimate the impact of abnormal night-time BP on CV mortality in patients with significant atherosclerosis established by coronary angiography. The secondary goal was to evaluate the prevalence of abnormal night-time BP in this group of patients, for both those with and without hypertension.
Methods
From June 2003 to August 2006, the study recruited 1905 consecutive individuals (28–84 years of age) based on clinical data or the findings of an abnormal stress test, who were referred for diagnostic coronary angiography to our department. The exclusion criteria were significant valvular heart disease or valvular heart disease qualifying the patient for cardiosurgery, congestive heart failure of NYHA class III or IV, renal insufficiency with a creatinine level ≥ 2.0 mg/dl, permanent or persistent atrial fibrillation, and other chronic diseases leading to limited life expectancy. According to the inclusion and exclusion criteria, 1345 subjects were enrolled to the study and from this group 891 subjects with significant atherosclerosis (at least 70% stenosis of at least one coronary artery) were selected. The investigation was performed as a cohort study. All of the subjects gave their written consent for the study after being informed of its nature and purpose. The study protocol was approved by the Ethics Committee of the Medical University of Gdansk. On admission day, before coronary angiography, fasting blood samples were collected in order to measure glucose, creatinine, high-density lipoprotein (HDL)-cholesterol and triglycerides levels. Low-density lipoprotein (LDL)-cholesterol was estimated according to Friedwald's formula. In a period of 2–4 weeks after coronary angiography, patients were invited to come to the outpatient clinic in the morning of a working day (Monday to Friday). During this visit the following data were obtained: (i) two sphygmomanometric BP values (5 min apart) taken in the sitting position, using the appropriate cuff size and performed by trained observers; (ii) measurements of waist and arm circumference to the nearest 0.10 cm taken with steel tape; (iii) two heart rate measurements (radial pulse), i.e. one after each BP measurement; (iv) 24-h ambulatory BP monitoring using an oscillometric device (SpaceLabs 90210, SpaceLabs Inc., Redmond, Washington, USA) with BP readings set at 20-min intervals (06:00–18:00 h) and at 30-min intervals (18:00–06:00 h) using the appropriate cuff size. Participants were sent home with instructions to hold the arm immobile at the time of measurements, to keep a diary of daily activities and to return to the hospital for device removal 24 h later. From the time of the baseline visit to 31 December 2009 (median follow-up 4.7 years), the survival state was ascertained by telephone interview, and by copy of death certificate from district registries and the National Health Service. The primary endpoint was CV mortality and secondary all-cause mortality. The causes of death reported in the certificate were coded according to the International Statistical Classification of Diseases and Related Health Problems, 10th revision version for 2003, and were adjudicated according to National Health Service data (Citation10). CV endpoints and mortality encompassed deaths from acute coronary syndromes, ischemic heart disease, heart failure, cardiac sudden death, cardiac arrhythmias, stroke and peripheral artery disease. In all outcome analyses, the first event within each category was only considered. Ambulatory BP and two clinic BPs were separately averaged. Ambulatory BP values were erased from artifacts and averaged over 24 h; daytime (08:00–22:00 h) and night-time (00:00–06:00 h). Averages were also calculated for the corresponding clinic and 24-h, daytime and night-time heart rate values. Calculations were made in the number (%) of CV or all-cause deaths in subjects with daytime BP < 135/85 mmHg and daytime BP ≥ 135/80 mmHg (according to NICE recommendations). Data from groups of subjects were compared using the t-test for unpaired observations and the χ2 test of proportions. In the study group, we used six separate Cox proportional hazards models to examine clinic, daytime and night-time BP values, and the corresponding the risk of CV and all-cause death. The time duration to CV or all-cause death was determined from the baseline date to the date of death according to the certificate. Covariates in all adjusted multivariate models included gender (male/female), age (continuous), LDL-cholesterol level (continuous), fasting glucose level (continuous), waist circumference (continuous), current smoking status (yes/no) and myocardial infarction history (yes/no). The significance of individual coefficients in the Cox proportional hazards models were determined by the 95% confidence limits for hazards ratios (HRs). A p < 0.05 was taken as the level of statistical significance. Throughout the text the symbol “±” refers to the SD of the mean.
Results
The study population consisted of 891 patients with significant atherosclerosis (mean age 63.7 ± 9.4 years). In the overall study population, median follow-up was 4.7 years (5th–95th percentile interval, 2.6–5.8 years). During 4081 person-years of follow-up, 94 participants died (23.0 per 1000 person-years) of which 61 were due to CV causes (14.9 per 1000 person-years). In the group of patients with normal daytime BP in comparison with those with abnormal daytime BP, there was a lower CV mortality (5.6% vs 9.8%, p < 0.02). shows the prevalence of all-cause and CV mortality with normal and abnormal daytime and night-time BP in the study population. Hazard ratios for clinic BP ≥ 140/90 mmHg, abnormal daytime and night-time BP ≥ 120/70 mmHg appear in . The Kaplan–Meier survival function shows a significantly lower incidence of total mortality in participants with normal daytime BP and night-time BP < 120/70 mmHg in comparison with those with abnormal daytime BP and night-time BP ≥ 120/70 mmHg (p = 0.05), and a lower incidence of CV mortality in participants with normal daytime BP and night-time BP < 120/70 mmHg in comparison with those with abnormal daytime BP and night-time BP ≥ 120/ 70 mmHg (p < 0.02) and those with either abnormal daytime BP or night-time ≥ 120/70 mmHg (p < 0.05) ().
Figure 1. Prevalence of cardiovascular (CV) and all-cause death in subjects with normal daytime blood pressure (BP) and night-time BP < 120/70 mmHg, either abnormal daytime BP or night-time BP ≥ 120/70 mmHg and abnormal daytime BP and night-time BP ≥ 120/70 mmHg.
Figure 2. Hazard ratio (95% confidence intervals, CIs) for cardiovascular (CV) death and all-cause death in subjects with clinic blood pressure (BP) ≥ 140/90 mmHg, abnormal daytime BP and night-time BP ≥ 120/70 mmHg after adjustment for age, gender, smoking, low-density lipoprotein (LDL)-cholesterol level, body mass index (BMI) and diabetes.
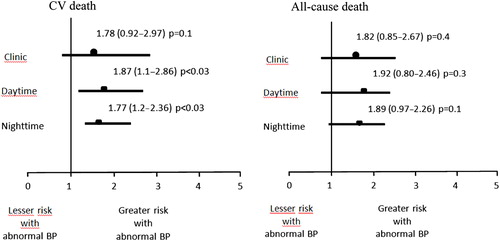
Figure 3. Kaplan–Meier survival curves for (a) cardiovascular (CV) death and (b) all-cause death in subjects with normal daytime blood pressure (BP) and night-time BP < 120/70 mmHg, either abnormal daytime BP or night-time BP ≥ 120/70 mmHg and abnormal daytime BP and night-time BP ≥ 120/70 mmHg.
Mean clinic BP was 138.7 ± 20.7 mmHg for systolic and 77.9 ± 11.5 mmHg for diastolic. Mean 24-h BP was 124.8 ± 14.0 mmHg for systolic and 71.4 ± 8.5 mmHg for diastolic, mean daytime BP was 127.5 ± 13.9 mmHg for systolic and 74.2 ± 8.8 mmHg for diastolic, and mean night-time BP was 120.4 ± 15.9 mmHg for systolic and 66.8 ± 9.1 mmHg for diastolic. The study population was divided into patients with normal daytime BP values (systolic BP < 135 mmHg and diastolic BP < 85 mmHg) and normal night-time BP values (systolic BP < 120 mmHg and diastolic BP < 70 mmHg); abnormal daytime BP values (systolic BP ≥ 135 mmHg and diastolic BP ≥ 85 mmHg) or abnormal night-time BP values (systolic BP ≥ 120 mmHg and diastolic BP ≥ 70 mmHg); abnormal daytime BP values and normal night-time BP values. shows the baseline characteristics of these participants. There were 266 subjects with abnormal daytime BP, which corresponded to 29.8% of the study population. shows mean clinic, 24-h, daytime and night-time BP values in the studied groups. In the group with normal daytime BP, a clinic BP value ≥ 140/90 mmHg was observed in 25.7% (n = 161) of patients and a night-time BP value ≥ 120/70 mmHg in 37.8% (n = 236), but in the group with abnormal daytime BP, a clinic BP value < 140/90 mmHg was observed in 22.5% (n = 60) and a night-time BP value < 120/70 mmHg in 6.8% (n = 18). Among patients with normal daytime BP and abnormal night-time BP 28.8% have normal clinic BP.
Table I. Baseline characteristics of subjects with normal and abnormal daytime blood pressures (BPs).
Table II. Blood pressure (BP) values in subjects with normal and abnormal daytime BPs.
shows pharmacotherapy in the studied groups. In the study population there were 43.6% (n = 389) of patients with normal daytime BP and night-time BP < 120/70 mmHg, 28.5% (n = 254) of patients with either abnormal daytime BP or night-time BP ≥ 120/70 mmHg and 24.8% (n = 248) of patients with abnormal daytime BP and night-time BP ≥ 120/70 mmHg.
Table III. Pharmacotherapy of subjects with normal and abnormal daytime blood pressures (BPs).
Discussion
The key finding of our study is that not only daytime but also night-time BP plays an important role in determining CV risk assessment in patients with stable coronary artery disease (CAD). The uniqueness of our research is ABPM performed in patients with CAD established on the basis of significant atherosclerosis in coronary angiography. It is the first such large study that has proved ABPM superiority over traditional clinic BP measurements in patients with significant CAD.
Our study partly confirmed NICE recommendations concerning added prognostic value of ABPM over clinic BP measurements. According to our findings, a quarter of participants with normal daytime BP (< 135/85 mmHg) had elevated clinic BP (≥ 140/90 mmHg). However, about a quarter of participants with abnormal daytime BP values (≥ 135/85 mmHg) had normal clinic BP values (< 140/90 mmHg), but over one third of subjects had normal daytime BP and elevated night-time BP (≥ 120/70 mmHg). Therefore, in the context of our findings, determining the severity of hypertension on the basis of clinic or ambulatory BP measurements performed during working hours only seems insufficient. In our study, an elevated night-time BP value was related to a higher CV risk in median 4.7 years of follow-up. The first prospective study to demonstrate the important role of night-time BP measurements was the Ohasama study. In this study, each 5% decrease of decline in nocturnal BP was associated with a 20% greater risk of CV mortality (Citation11). In the population of the PAMELA study, night-time BP was even related to a higher prognostic significance over daytime BP (Citation1). In other studies performed in non-CAD populations, night-time BP also had a CV prognostic value (Citation12–14). Furthermore the study concerning nocturnal hypertension have recently confirmed that elevated night-time BP values were related to atherosclerosis risk factors such as uric acid level, creatinine level and dysfunction of renin– angiotensin–aldosterone system and autonomic nervous system (Citation15). These mechanisms are probably responsible for coronary atherosclerosis in patients with nocturnal hypertension.
Our study revealed that elevated clinic BP was not significantly associated with either CV or all-cause mortality. This fact may be connected with hypertension pharmacotherapy that was traditionally given on the basis of clinic BP values and could have reduced baseline CV risk. Previous large studies have provided apparently conflicting data. On the one hand, in the Dublin Outcome study, ambulatory BP measurement in untreated hypertensive patients was superior to clinic in predicting CV mortality during a median follow-up period of 8.4 years. In this study, the prevalence of known CV risk factors other than hypertension was higher among patients who died from CV causes (Citation13). On the other hand, in the PAMELA study, the estimation of CV risk mortality was equally good for ABPM and clinic BP during 11 years of follow-up (Citation1). It seems that the main reason for the discrepancy between PAMELA findings and our own is associated with the studied population. We included only CAD patients with significant coronary atherosclerosis with a high baseline CV risk, but the PAMELA study included patients from the general population (residents of Monza) with a lower baseline CV risk related to the inclusion criteria of the study. In the PAMELA study only about one hundred of the included patients had CV disease (Citation16,Citation17).
In our study, neither clinic nor daytime and night-time BPs were significantly connected to all-cause mortality. CV mortality estimation better than all-cause mortality is related to the study population of CAD treated patients and the relatively short period of follow-up. Further follow-up of the study will probably develop new data.
After taking into consideration both daytime and night-time BPs, our study revealed a higher prevalence of CV and all-cause deaths in patients with abnormal daytime (≥ 135/85 mmHg) and night-time (≥ 120/70 mmHg) BP, than in patients with normal values for both. Analysis of Kaplan–Meier curves revealed lower all-cause mortality in subjects with normal daytime and night-time BP in comparison with those with abnormal values for both. Furthermore and more importantly, there was lower CV mortality in subjects with normal BP levels for both daytime and night-time and normal BP levels for either daytime or night-time than in subjects with abnormal BP values for both daytime and night-time. Our study confirms that optimal control of both daytime and night-time BP values in subjects with established significant CAD is essential in CV mortality prevention. Thus, detecting abnormal daytime and night-time BP values is clinically relevant in a population with established coronary atherosclerosis. A randomized controlled trial is needed to consolidate our findings, which so far is currently not available. Previous studies have confirmed the important role of daytime and night-time BPs in predicting all-cause and CV deaths (Citation18). Analysis of the Belgian Ambulatory Blood Pressure Monitoring database containing 3468 hypertensive patients with no history of CV disease clearly reveals that both daytime and night-time BPs are complementary in predicting all cause and CV mortality (Citation19). Gosse et al. found a strong relationship between arising BP measured by ambulatory device and the occurrence of CV events in a population of previously untreated hypertensive patients (Citation20).
The findings of our study have important clinical relevance. Our findings support NICE recommendations that ABPM is indispensable to the management of hypertension, especially in CAD patients; however, in subjects with significant coronary atherosclerosis, BP monitoring should be performed not only during working hours but also during sleeping hours. Only by monitoring both daytime and night-time BPs can CV risk in these patients be comprehensively assessed. In our opinion, future guidelines should address these issues.
Declaration of interest No conflict of interest for all authors. There are no relationships with industry.
References
- Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: Follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–1783.
- Mancia G, Sega R, Grassi G, Cesana G, Zanchetti A. Defining ambulatory and home blood pressure normality: Further considerations based on data from the PAMELA study. J Hypertens. 2001;19:995–999.
- Fagard R, Staessen J, Thijs L, Amery A. Multiple standardized clinic blood pressures may predict left ventricular mass as well as ambulatory monitoring. A metaanalysis of comparative studies. Am J Hypertens. 1995;8(5 Pt 1):533–540.
- Fan HQ, Li Y, Thijs L, Hansen TW, Boggia J, Kikuya M, et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J Hypertens. 2010;28:2036–2045.
- Li Y, Boggia J, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, et al. Is blood pressure during the night more predictive of cardiovascular outcome than during the day?. Blood Press Monit. 2008;13:145–147.
- Lurbe E, Redon J, Kesani A, Pascual JM, Tacons J, Alvarez V, et al. Increase in nocturnal blood pressure and progression to microalbuminuria in type 1 diabetes. N Engl J Med. 2002;347:797–805.
- Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–1187.
- Verdecchia P. Prognostic value of ambulatory blood pressure: Current evidence and clinical implications. Hypertension. 2000;35:844–851.
- Zanchetti A, Bond MG, Hennig M, Neiss A, Mancia G, Dal Palù C, et al. Risk factors associated with alterations in carotid intima-media thickness in hypertension: Baseline data from the European Lacidipine Study on Atherosclerosis. J Hypertens. 1998;16:949–961.
- WHO. International statistical classification of diseases and related health problems. 10th revision version for 2003. Geneva: WHO; 2003.
- Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: The Ohasama study. J Hypertens. 2002;20:2183–2189.
- Staessen JA, Thijs L, Fagard R, O’Brien ET, Clement D, de Leeuw PW, et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA. 1999;282:539–546.
- Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: The Dublin outcome study. Hypertension. 2005;46:156–161.
- Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M, et al. Predictors of all-cause mortality in clinical ambulatory monitoring: Unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–1241.
- Chatzistamatiou EI, Moustakas GN, Veioglanis S, Papoutsis D, Memo G, Tsioufis C, et al. Nocturnal hypertension: Poor correlation with office blood pressure but strong prognostic factor for target organ damage. Hellenic J Cardiol. 2012;53:263–272.
- Cesana G, De Vito G, Ferrario M, Libretti A, Mancia G, Mocarelli P, et al. Ambulatory blood pressure normalcy: The PAMELA Study. J Hypertens. 1991;9 Suppl:S17–23.
- Mancia G, Sega R, Bravi C, De Vito G, Valagussa F, Cesana G, et al. Ambulatory blood pressure normality: Results from the PAMELA study. J Hypertens. 1995;13(12 Pt 1):1377–1390.
- Sobiczewski W, Wirtwein M, Trybala E, Gruchala M. Severity of coronary atherosclerosis and stroke incidence in 7-year follow-up. J Neurol. 2013. Mar 20. [Epub ahead of print].
- Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51:55–61.
- Gosse P, Cipriano C, Bemurat L, Mas D, Lemétayer P, N’Tela G, et al. Prognostic significance of blood pressure measured on rising. J Hum Hypertens. 2001;15:413–417.

