Abstract
Background and aims. Arterial hypertension doubles the risk of coronary heart disease, heart and kidney failure, and peripheral arterial disease. Less variation in diurnal ambulatory blood pressure monitoring (ABPM) patterns may affect mortality outcome. Therefore, as hypertension occurs in over 95% of older subjects, the prognostic value of dipping status in older hypertensive patients will be assessed. Method. The retrospective study group consisted of 170 hypertensive patients, aged 75–84 years, enrolled in the years 2005 to 2007. Baseline measures included 24-h ABPM. Diurnal index and dipping status was calculated and stratified the group into dippers (40 patients, 23.5%), non-dippers (65 patients, 38.2%) and reverse-dippers (65 patients, 38.2%). Results. During a 5-year observation, after baseline we have observed 69 deaths (40.9%) from the whole group of 170 patients with 23 (35.4%) being non-dippers and 36 (55.4%) reverse-dippers. There were significant differences between the groups divided according to diurnal dipping status in survival time, number of recorded deaths and night mean blood pressure. We have identified and confirmed risk factors for the all-cause mortality: age, mean systolic and diastolic blood pressure, diurnal index and dipping status (dipping, non-dipping or reverse-dipping). Conclusion. Reverse-dippers and non-dippers revealed worse prognosis compared with dippers.
Introduction
Arterial hypertension is the most common cardiovascular disease and represents a major risk factor for further cardiovascular disease (Citation1–3). It is the most significant risk factor of atherosclerosis, causing a serious global medical and socio-economic problem. Although antihypertensive therapy clearly reduces the risk of cardiovascular and renal disease, a significant proportion of hypertensive patients are inadequately treated or not treated at all.
Aging is a universal progressive decline in the functional reserves of an organism initially and later in the actual functions of the body over time. Aging is not a disease, but the risk of disease is affected by aging, often dramatically and fundamentally. It changes the biochemical composition of tissues, physiological capacity decreases, the ability to maintain homeostasis in extreme situations decreases and susceptibility to the disease process increases.
In populations of 75 years and over, hypertension occurs in over 95% of subjects, so the specific issue is hypertension in aging population. Blood pressure (BP) in humans has a normal diurnal variation. With increasing systolic (SBP) and diastolic BP (DBP), there is a continuous curvilinear increase in the risk of cardiovascular diseases (Citation4–6). In epidemiological terms, there is no clear level of BP, which would determine arterial hypertension. Separation of normal BP and hypertension is thus largely arbitrary and changes with new knowledge throughout history. The current definition is based on the results of randomized clinical trials, and hypertension is defined as BP 140/90 mmHg or higher, as it is a limit from which the benefits of treatment of hypertension outweigh its risks.
BP is influenced by many factors, some of which are unpredictable, but many of them are not affected by random effects, and are rhythmically repetitive with different interval (Citation7,Citation8). BP is affected mostly by circadian rhythm, similar to many other biological functions. Under normal circumstances, BP reaches the highest values in the early morning and at night during sleep BP values decrease (Citation7–9). Consistent monitoring and analysis of circadian BP changes is made possible by 24-h (or longer) ambulatory BP monitoring (ABPM). Decrease in mean nocturnal BP by 10–20% compared with the average daily value is a sign of normal physiological diurnal rhythm of BP, and termed “dipping”. If there is lower decrease in average night-time BP values (less than 10%), it is termed “non-dipping”. If the average BP at night rises above the daily average values, instead of a physiological decline, it is termed “reverse-dipping” (Citation9). Therefore, we aimed first to evaluate the prognostic values of ABPM in a specific group of elderly hypertensive patients aged between 75 and 84 years, with the 5-year follow-up of overall mortality. Second, differences in diurnal index and differences between dippers, non-dippers and reverse-dippers, related to overall mortality, as well as other selected endpoints, will be assessed.
Patients and methods
Our study was retrospective evaluation of global mortality of a group of 170 patients aged 75–84 years. All the patients have baseline ABPM measurements during 2005, 2006 and 2007. The observation lasted 5 years. We have confirmed the death or survival in all 170 included patients, using the state evidence of Ministry of Health.
The work was approved by the central ethics committee of the University Hospital and Commenius University in Bratislava.
The most important exclusion criteria were: known secondary cause of hypertension, not enough successful inflation rate during ABPM, serious heart failure (NYHA III, IV), renal failure (glomerular filtration rate less than 0.25 ml/s), malignancy, non-compliant patients and reported severe sleep disturbances according to the patient's diary during ABPM.
Details in the range of basic demographic parameters, personal and medical history, performed biochemical analyses, anthropometric parameters were obtained from patients’ medical records.
Ambulatory BP oscillometric monitoring was performed for 24 h under standard conditions using the CardioSoft Tonoport-V (General Electric, USA) device, with the cuff loaded on the non-dominant arm. Patients recorded their activities and period of sleep during the 24-h monitoring period in their diaries.
Diurnal index was calculated by the formula:
Non-dipping was defined as a decrease in mean nocturnal BP compared with the average daily value of BP by less than 10% (diurnal index in the range 0 to − 10%), reverse-dipping was defined as an increase in mean nocturnal BP compared with the average daily value (diurnal index positive, > 0%).
Biochemical analyses (serum creatinine, fasting glucose) were performed in a hospital laboratory with accredited methods.
Statistical analyses
We have used SPSS for Windows; version 19 (IBM) for the statistical analysis.
We have used an analysis of variance (ANOVA) test for comparison of continuous variables between dippers, non-dippers and reverse-dippers, t-test for comparison of continuous variables between groups of dippers and patients with impaired diurnal sign, and for comparison of groups according to mortality, Pearson chi-square test for comparison of discrete variables between dippers, non-dippers and reverse-dippers, between dippers and patients with impaired diurnal sign, and between groups divided according to mortality.
Results
Patients enrolled for the study included 170 with the average 79.3 ± 2.9 years. There were 136 (80%) women and 34 (20%) men. During the observing period, death was reported in 69 patients (40.6%), full 5-year (1825 days) survival in 101 patients (59.4%) from the whole group. The average length of observing period in the group with reported death was 891 ± 496 days.
Diurnal sign (decrease in mean nocturnal BP by 10% or more) has been preserved only in 40 patients (23.5%) from 170 patients. Reduced or reversed diurnal sign was observed in 130 patients (76.5%), of which “reverse-dipping” was present in half of these (65 patients). The average diurnal index was in the whole group of patients for SBP − 3.53 ± 10.21% and for DBP − 7.25 ± 11.81%. The average BP was 137 ± 16.7/78 ± 9.9 mmHg. Only 54 patients (31.8%) demonstrated well controlled SBP and DBP during ABPM.
History of coronary heart disease (CHD) was also present in all of the patients (100%); myocardial infarction history was present in 31.8% of patients. Other most frequent comorbities were heart failure (50%), atrial fibrillation or atrial flutter (37.6%), and diabetes mellitus (36.5%). Therefore, this group of patients has very high cardiovascular risk. The most commonly used antihypertensive drug group were beta-blockers (77.6%), angiotensin-converting enzyme inhibitors (57.6%) and diuretics (58.2%).
and show a comparison of continuous variables between groups of dippers, non-dippers and reverse-dippers using the ANOVA test () and between groups dippers compared with other patients with impaired diurnal character – together non-dippers and reverse-dipper-combined in single group () using the t-test. The results show that there was significant difference in the periods of survival between the dippers and the rest of the patients (non-dippers and reverse-dippers); in the case of division of the patients into three groups – dippers, non-dippers and reverse-dippers – there was not a significant difference (p = 0.088).
Table I. Comparison of groups according to diurnal sign, continuous variables.
Table II. Comparison of groups according to diurnal sign, continuous variables.
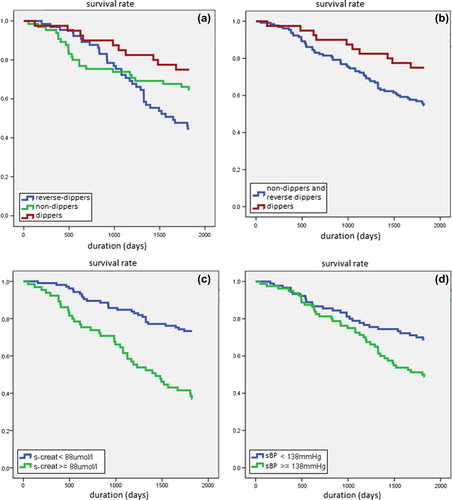
and show a comparison of discrete variables between groups of dippers, non-dippers and reverse-dippers by the chi-square test () and between groups of dippers compared with other patients with impaired diurnal sign () by the chi-square test. also graphically illustrates the results of significant differences. There was in both cases significant difference observed in mortality between the groups of patients: reverse-dippers and non-dippers have a higher mortality rate than dippers. Differences in age and mean BP between groups were not significant.
Table III. Comparison of groups according to diurnal sign, discrete variables.
Table IV. Comparison of groups according to diurnal sign, discrete variables.
and show a comparison of patients divided into groups according to the survival status during the 5-year observing period. Statistical significance was determined by t-test () for continuous variables and Pearson's chi-square test () for discrete variables. Significant differences were observed between the groups in age, mean SBP, mean nocturnal SBP and DBP during ABPM and diurnal index for both SBP and DBP. The most important of the identified significant differences is also shown graphically in and . The survivors have slightly lower age, lower mean SBP, lower mean nocturnal SBP and DBP, and higher diurnal index for both SBP and DBP.
Table V. Comparison of groups according to mortality, continuous variables.
Table VI. Comparison of groups according to mortality, discrete variables.
There were no significant differences in mean DBP during 24-h monitoring between the survivors and death groups.
Using a Cox regression analysis, risk factors were analyzed for mortality: age, gender, mean SBP and DBP, mean day and night SBP and DBP, and diurnal index. We have found that the significant parameters affecting the 5-year mortality were age, mean SBP and DBP, presence of diurnal character, diurnal index, history of myocardial infarction and heart failure, body mass index (BMI) and serum creatinine (; we present only significant values).
Table VII. Cox regression analysis of risk factors for mortality (only significant values mentioned).
For the significant parameters using the receiver operating characteristic (ROC) analysis, we have determined the discriminant, on the basis of which we show the Kaplan–Meier curves for survival ().
Discussion
Retrospective evaluation of 24-h ABPM and overall mortality in elderly hypertensive during a 5-year follow-up was presented. Primarily, the focus was on the diurnal rhythm of BP, expressed either continuously as diurnal index or discretely as the presence of diurnal sign (dipping) or absence of diurnal sign (non-dipping). In some evaluations, reverse-dipping with an increase in BP at night was added.
Mechanisms responsible for abnormal diurnal rhythm are not fully understood. Sympathovagal imbalance (Citation10) and sympathetic hyperactivity at night are likely to play an important role (Citation11–13). The studies conducted so far (Citation14–22) have demonstrated a certain degree of the association of non-dipping and cardiovascular and all-cause mortality. Impaired diurnal rhythm was also strongly associated with multiple cardiovascular risk factors – diabetes mellitus, arterial hypertension, chronic renal insufficiency and ischemic heart disease and with age (Citation23). So far, published studies have included the entire age range of the adult population, not focusing only on specific populations in the elderly (over 75 years), which is at highest risk, as presented in the current study.
In our study, 170 hypertensive patients (mean age 79 ± 2.9 years) were enrolled. The proportion of patients with normal diurnal sign (dippers) was quite low (40 patients, 23.5%), compared with non- dippers (65 patients, 38.2%) and reverse-dippers (65 patients, 38.2%), in comparison with studies published so far (Citation14,Citation22,Citation24). A possible explanation is that these studies investigated a broader and more diverse group of the adult population. In these works, the non-dipping was significantly associated with age (Citation14,Citation15,Citation17,Citation22,Citation24). The possible reason why we have not observed this relationship in our work is probably the patients’ selection, with a specific close group of patients with higher age.
Total mortality for the evaluation of patients’ survival was computed. Overall mortality is, according to some authors, a more appropriate endpoint as e.g. cardiovascular mortality, particularly in retrospective studies, where comorbidities may result in clinical uncertainties and errors in determining the cause of death (Citation25,Citation26). Total mortality may be the most reliable endpoint, especially in polymorbid elderly patients who were monitored in the presented study.
During the 5-year follow-up period, we have reported 69 deaths with an average length of survival in this group 891 ± 496 days. When comparing groups of hypertensive patients surviving with a group of death, we have found significant differences in age and mean SBP (). These differences were also observed by other authors (Citation14,Citation15,Citation17,Citation22,Citation24). Significant differences between these groups were evident for the average nocturnal SBP and DBP, diurnal index for SBP and DBP, and serum creatinine. These relationships have been well described in the literature (Citation14,Citation15,Citation17,Citation22,Citation24).
Between groups divided according to diurnal index into dippers, non-dippers and reverse-dippers, a significant difference was observed in the rate of survival and the number of reported deaths in the group. The absence of normal physiological diurnal index, the dipping of BP at night, was associated with higher mortality. Our observation is consistent with the findings of studies conducted previously (Citation14,Citation15,Citation17,Citation19,Citation21,Citation22,Citation24), albeit they included patients with a lower average age. The novelty of our work is the selection of hypertensive patients within a specific age group. Significant differences were found in share of the dippers, non-dippers and reverse-dippers among surviving patient groups and having recorded death. There were fewer deaths recorded in the group of dippers than non-dippers and reverse-dippers, and fewer deaths in the group of non-dippers than reverse-dippers. From the aspect of mortality, the reverse-dippers group has the worst prognosis.
On the basis of this study, it is possible to better identify the risk groups and risk factors in the most vulnerable group of polymorbid hypertensive patients aged over 75 years by ABPM.
Using Cox regression analysis, we have identified risk factors for total mortality in our group, particularly age, mean SBP and mean DBP, diurnal index, diurnal character (or dipping vs non-dipping), history of myocardial infarction and heart failure, BMI and blood serum creatinine. These risk factors affecting mortality in our group are well known and have been identified by a number of epidemiological studies (Citation5,Citation14,Citation27,Citation28). However, our study focused on patients aged 75–84 years, for which there are considerably fewer published works.
Conclusion
To conclude, in an analysis of ABPM in elderly hypertensive patients, a low proportion of patients with normal diurnal sign, dippers (23.5%), was observed. We found a significant difference between groups divided according to the diurnal index into dippers, non-dippers and reverse-dippers in the rate of survival and the number of reported deaths in the studied group of elderly (over 75 years old) hypertensive patients.
The following risk factors for all-cause mortality identified in this particular elderly hypertensive group included: age, mean SBP and DBP, diurnal index, diurnal sign (dipping or non-dipping), history of myocardial infarction and heart failure, BMI and serum creatinine.
It was confirmed that a disturbed diurnal rhythm (non-dipping and reverse-dipping) is a risk factor for all-cause mortality, even in a specific hypertensive population aged over 75 years. Impaired diurnal sign (non-dipping and reverse-dipping) is associated with several cardiovascular risk factors, which may contribute to the association between non-dipping and overall cardiovascular mortality.
Acknowledgement
This study was elaborated within the grant of European Regional Development Fund – Project FNUSA-ICRC (No.CZ.1.05/1.1.00/02.0123).
Conflict of interest: Authors declare no conflict of interest.
References
- The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension and of the European Society of Cardiology, Guidelines Committee. 2007 Guidelines for the Management of Arterial Hypertension. J Hypertens. 2007;25:1105–1187.
- Kruzliak P, Novák J, Novák M. Vascular endothelial growth factor inhibitor-induced hypertension: From pathophysiology to prevention and treatment based on long-acting nitric oxide donors. Am J Hypertens. 2014;27:3–13.
- Dukát A. Hypertenzia v staršom veku. Cardiol. 2003;12: 9–10.
- Bouhanick B, Bongard V, Amar J, Bousquel S, Chamontin B. Prognostic value of nocturnal blood pressure and reverse-dipping status on the occurrence of cardiovascular events in hypertensive diabetic patients. Diabetes Metab. 2008;34(6 Pt 1):560–567.
- Guidelines Committee. 2003 European Society of Hypertension, European Society of Cardiology guidelines for the management of hypertension. J Hypertens. 2003;21:1011–1053.
- Widimský J et al. Hypertenze. 2. rozšírené a prepracované vydání. Praha. Triton. 2004:590.
- Cicek Y, Durakoglugil ME, Kocaman SA, Cetin M, Erdogan T, Dogan S, et al. Non-dipping pattern in untreated hypertensive patients is related to increased pulse wave velocity independent of raised nocturnal blood pressure. Blood Press. 2012;22:34–38.
- Gonzales Rodriguez E, Hernandez A, Koehler Ballan B, Pechère-Bertschi A. Arterial blood pressure circadian rhythm: Significance and clinical implications. Rev Med Suisse. 2012;8:1709–12, 1714–1715.
- Kario K, Shimada K. Risers and extreme-dippers of nocturnal blood pressure in hypertension: Antihypertensive strategy for nocturnal blood pressure. Clin Exp Hypertens. 2004;26:177–189.
- Malan L, Hamer M, Schlaich MP, Lambert GW, Ziemssen T, Reimann M, et al. Defensive coping facilitates higher blood pressure and early sub-clinical structural vascular disease via alterations in heart rate variability: The SABPA study. Atherosclerosis. 2013;227:391–397.
- Kondo K, Matsubara T, Nakamura J, Hotta N. Characteristic patterns of circadian variation in plasma catecholamine levels, blood pressure and heart rate variability in type 2 diabetic patients. Diabet Med. 2002;19:359–365.
- Kurpesa M, Trzos E, Drozdz J, Bednarkiewicz Z, Krzemińska-Pakuła M. Myocardial ischemia and autonomic activity in dippers and non-dippers with coronary artery disease: Assessment of normotensive and hypertensive patients. Int J Cardiol. 2002;83:133–142.
- Nakano Y, Oshima T, Ozono R, Higashi Y, Sasaki S, Matsumoto T, et al. Non-dipper phenomenon in essential hypertension is related to blunted nocturnal rise and fall of sympatho-vagal nervous activity and progress in retinopathy. Auton Neurosci. 2001;88:181–186.
- Brotman DJ, Davidson MB, Boumitri M, Vidt DG. Impaired diurnal blood pressure variation and all-cause mortality. Am J Hypertens. 2008;21:92–97.
- Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001; 38:852–857.
- Kobrin I, Oigman W, Kumar A, Ventura HO, Messerli FH, Frohlich ED, et al. Diurnal variation of blood pressure in elderly patients with essential hypertension. J Am Geriatr Soc. 1984;32:896–899.
- Lurbe E, Redon J, Pascaul JM, Tacons J, Alvarez V. The spectrum of circadian blood pressure changes in type 1 diabetic patients. J Hypertens. 2001;19:1421–1428.
- Ohkubo T, Imai Y, Tsuji I, Nagai K, Watanabe N, Minami N, et al. Relation between nocturnal decline in blood pressure and mortality. The Ohasama Study. Am J Hypertens. 1997;10:1201–1207.
- Palmas W, Pickering TG, Teresi J, Schwartz JE, Moran A, Weinstock RS, et al. Ambulatory blood pressure monitoring and all-cause mortality in elderly people with diabetes mellitus. Hypertension. 2009;53:120–127.
- Portaluppi F, Montanari L, Massari L, Di Chiara V, Capanna M. Loss of nocturnal decline of blood pressure in hypertension due to chronic renal failure. Am J Hypertens. 1991;4:20–26.
- Suzuki M, Guilleminault C, Otsuka K, Shiomi T. Blood pressure dipping and non-dipping in obstructive sleep apnea syndrome patients. Sleep. 1996;19:382–387.
- Verdechia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M, et al.Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801.
- van Lill L, Malan L, van Rooyen J, Steyn F, Reimann M, Ziemssen T. Baroreceptor sensitivity, cardiovascular responses and ECG left ventricular hypertrophy in men: The SABPA study. Blood Press. 2011;20:355–61.
- Verdechia P, Angeli F, Mazzotta G, Garofoli M, Ramundo E, Gentile G, et al. Day–night dip and early-morning surge in blood pressure in hypertension: Prognostic implications. Hypertension. 2012;60:34–42.
- Gottlieb SS. Dead is dead – Artificial definitions are no substitute. Lancet. 1997;349:662–663.
- Lauer MS, Blackstone EH, Young JB, Topol EG. Cause of death in clinical research: Time for reassessment? J Am Coll Cardiol. 1999;34:618–620.
- World Health Organization–International Society of Hypertension Guidelines for the management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17: 151–183.
- Kannel WB, Gordon T. Evaluation of cardiovascular risk in the elderly: The Framingham study. Bull Acad Med. 1978; 54:573–591.