Abstract
Aim. To date, accurate reports about the prevalence of high normal blood pressure (BP) and hypertension among Chinese adolescents have been rare. We examine the sex-specific and age-specific prevalence of high normal BP and hypertension, and the associated risk factors among multi-ethnic Chinese adolescents from a large and representative sample. Methods. 29,997 adolescents aged 8–18 years old received blood pressure measurement on one clinical visit. Results. The overall prevalence was 4.15% for hypertension (4.73% for boys and 3.62% for girls) and 29.85% for high normal BP (33.40% for boys and 26.65% for girls). The odds ratios (ORs) increased with age, but the absolute changes of ORs were significantly different between boys and girls. Compared with that of the Han counterparts, the risk of high normal BP was 1.960-fold, 1.283-fold and 1.618-fold for Yi boys, Mongolian boys and Yi girls, respectively, whereas the OR was 0.440 for Tibetan boys, 0.492 for Tibetan girls and 0.794 for Korean girls. Compared with those of normal weight, overweight and obese adolescents had significantly increased risk of high normal BP (OR = 3.377 for obese boys and OR = 2.009 for overweight boys; OR = 2.865 for obese girls and OR = 1.738 for overweight girls). Rural adolescents had a higher risk of hypertension than those living in urban areas. Conclusion. The prevalence of high normal BP and hypertension was high in Chinese adolescents. Age, ethnicity, obesity, overweight, abnormal waist circumference, family history of cardiovascular diseases and dwelling at rural districts were significantly associated with pediatric high normal BP or hypertension.
Introduction
Cardiovascular diseases and cerebrovascular diseases have become the leading cause of mortality in both developed counties and developing countries. Hypertension has been identified as the major risk factor of cardiovascular diseases and cerebrovascular diseases leading to myocardial infarction, stroke, renal dysfunction and heart failure (Citation1–3). Many studies show that the prevalence of hypertension in children and adolescents increases worldwide (Citation4–7). It has been shown that childhood blood pressure is associated with blood pressure in later life, and elevated blood pressure in childhood increases the risk for the development of hypertension during adolescence (Citation4). Hypertension may begin in childhood or adolescence and then develop into adulthood (Citation5,Citation6). Hypertension in childhood is now commonly known to be an early risk factor for cardiovascular morbidity and mortality (Citation7). As blood pressure levels are typically retained throughout life, children with hypertension or high normal blood pressure (BP) are more likely to become hypertensive adults (Citation7).
Given that blood pressure can be influenced by age, gender and height for children and adolescents, the fourth report on the diagnosis, evaluation and treatment of high blood pressure in adolescents introduced a diagnostic standard about hypertension and high normal BP in children and adolescents according to their age, gender and height in 2004 (Citation8). Based on the specific blood pressure standard (the fourth report), the majority of studies reported prevalence rates of hypertension ranging from 1% to 5% among adolescents in abroad (Citation9). Some studies reported the varied prevalence rates of hypertension and high normal BP in other counties () (Citation10–18). In China, there were several studies having reported the prevalence of hypertension and high normal BP in children and adolescents (Citation19–21), but all these studies were conducted in only a province of China with a small sample size, which did not represent the general Chinese adolescent population. To date, accurate reports about the prevalence of high normal BP and hypertension among Chinese adolescents have been rare. Furthermore, as China is a multi-ethnic country and most minorities have their specific lifestyle, some studies have ever found that racial difference can influence the prevalence of high normal BP and hypertension (Citation22,Citation23). However, no information on the racial difference in prevalence of high normal BP and hypertension has been reported among Chinese multi-ethnic adolescents. Therefore, it will be important from the perspective of clinical and public health significance to investigate the prevalence of high normal BP and hypertension in a representative population sample of general Chinese multi-ethnic adolescents. This will facilitate the early detection and early management of pediatric high normal BP and hypertension.
Table I. Prevalence of high normal blood pressure and hypertension (%).
In this study, we examined the sex-specific, age-specific and race-specific prevalence of pediatric high normal BP and hypertension, and the associated risk factors among multi-ethnic Chinese adolescents aged 8–18 years old from a large and representative sample with their blood pressure measurement based on one clinical visit.
Materials and methods
Sample and participants
This study is based on data from a large-scale population survey on Chinese physiological constants and health conditions in a representative sample of general Chinese population from 2007 to 2011. It was supported by the Basic Performance Key Project by the Ministry of Science and Technology of the People's Republic of China, and has been approved by the review board of the Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences annually. In brief, this survey was carried out in six provinces of China, including Sichuan province, Heilongjiang province, Hunan province, Inner Mongolia autonomous region, Yunnan province and Ningxia Hui autonomous region. The three-stage cluster sampling method was used to select eligible subjects in each province. Firstly, two or three cities were sampled based on their economical status and ethnic inhabitations of minorities, and then several communities and villages were randomly selected in every city. In these selected communities and villages, all eligible people who were not suffering from severe chronic diseases and had not run a high fever in the past 15 days were considered our survey subjects.
Blood pressure measurement
Strict quality control standards of blood pressure measurement were carried out. Trained physicians performed blood pressure measurement following standard guidelines. Standard operating methods were used to measure blood pressure according to the fourth report on the diagnosis, evaluation, and treatment of high blood pressure in adolescents (Citation8) and Chinese guidelines for hypertension prevention and treatment (Citation24). Subjects were asked to avoid drinking coffee, tea or eating other stimulant food and drugs before the measurement. Blood pressure was measured in the morning after subjects had rested for 5 min in the seating position, with her or his back supported, feet on the floor and right arm supported with cubit fossa at heart level. The appropriate cuff was chosen based on their arm circumference. Blood pressure was measured based on one clinical visit. Two measurements were separated with a 5-min interval and the average of two measurements was used in the analysis.
Definition of high normal BP and hypertension
According to the fourth report (Citation8), hypertension was defined as average SBP and/or DBP levels ≥ 95th percentile for gender, age and height. High normal BP was defined as average SBP or DBP levels ≥ 90th percentile and < 95th percentile. Furthermore, as with adults, adolescents with SBP level ≥ 120 mmHg and/or DBP level ≥ 80 mmHg were also considered high normal BP. Percentiles of height were defined according to tables of reports of the physical fitness and health research of Chinese school students (Citation25).
Definitions of characteristics
We collected data including demographic characteristics (age, gender, educational level, ethnicity and residence), smoking, high-salt diets, body mass index (BMI), waist circumference (WC) and family history of cardiovascular diseases. Educational level was categorized into three groups: primary school, junior middle school and senior middle school. Ethnicities was grouped into Han, Yi, Miao, Mongolia, Tibetan, Hui, Tujia, Korean, Manchu, Yao, Dai, Qiang, et al. Residence included urban district and rural district on the basis of the habitation environment and gross domestic product level. Smokers were categorized into non-smoker and smoker according to their current smoking conditions. High-salt diets were self-reported. Family history of cardiovascular diseases meant that parents of subjects have suffered from some cardiovascular diseases.
BMI was defined as weight (kg) divided by squared height (m2). Weight and height was measured to the nearest 0.1 kg and 0.1 cm with the subjects wearing light undergarments and no shoes according to standard procedure (Citation26). According to the BMI reference norm for screening overweight and obesity in Chinese adolescents (Citation26), general obesity was defined as BMI ≥ 95th percentile, overweight was defined as BMI < 95th percentile and ≥ 85th percentile. WC was measured to the nearest 0.1 cm while subjects were in the standing position. According to a standard definition of child obesity worldwide (Citation27), abnormal WC is defined as WC ≥ 90th percentile.
Statistical analysis
The database was constructed with EPI3.02 software by two data managers and was corrected to guarantee the accuracy and integration of the data. Statistical analysis was conducted with SAS9.2 software (SAS institute Inc, Cary, NC, USA). Two-tailed p < 0.05 was defined as statistically significant. Continuous data were presented with mean and standard deviation (SD), and categorical data with number and percentage. Ordinal data were compared with Wilcoxon sum rank test. Logistic regression model was used to explore the association between demographic characteristics and high normal BP. Odds ratios (ORs) and 95% confidence intervals (CI) were used to reflect the risk of high normal BP.
Results
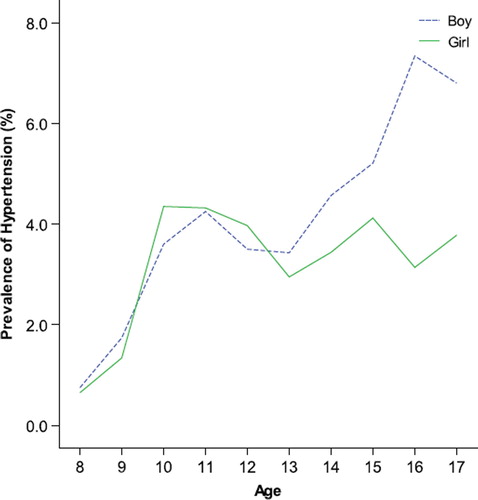
Among 29,997 subjects, 14,193 boys and 15,804 girls aged 8–18 years old took part in this study. The mean age was 13.7 ± 2.3 years old for boys and 13.9 ± 2.3 years old for girls. Of all them, 1244 subjects and 8953 subjects were hypertensive and prehypertensive, respectively, and the overall prevalence rates of hypertension and high normal BP were 4.15% and 29.85%, respectively. The prevalence rates of hypertension and high normal BP were significantly higher in boys than in girls (4.73% vs 3.62% for hypertension, and 33.40% vs 26.65% for high normal BP, p < 0.0001). showed the prevalence rates of hypertension in boys vs girls with increasing age. It could be found that the prevalence rates of hypertension were similar between the two genders before 13 years old but gradually different with aging after 13 years old.
presented the prevalence of hypertension and high normal BP by characteristics. With aging, the prevalence rates of hypertension and high normal BP increased gradually, from 0.7% and 8.4% at 8 years old to 5.1% and 37.1% at 17 years old. Significant difference of high normal BP and hypertension was found among the different educational levels. The prevalence of hypertension and high normal BP was significantly different among multi-ethnic adolescents. Yi subjects had the highest prevalence rates of hypertension (9.4%) and high normal BP (40.8%), whereas Tibetan subjects had the lowest prevalence rates of hypertension (1.5%) and high normal BP (19.7%). Compared with adolescents with normal weight, those who were obese and overweight had higher prevalence rates of hypertension (11.6% and 6.0%) and high normal BP (47.0% and 40.2%). Subjects with WC ≥ 90th had higher prevalence rate of hypertension (8.7%) and high normal BP (43.0%) than those with smaller WC. Adolescents whose parents have suffered from cardiovascular diseases had higher prevalence rate of hypertension (9.5%) and high normal BP (33.5%) than those without family history of cardiovascular diseases. No significant difference was found in the prevalence between subjects with or without a high-salt diet. Rural adolescents had higher prevalence rate of high normal BP (31.3%) than ones dwelling at urban districts (26.9%). Smokers had higher prevalence rates of hypertension and high normal BP than non-smokers (p < 0.0001).
Table II. Prevalence conditions of hypertension and high normal blood pressure (n(%)).
In view of the significant difference between the two genders, risk factors were explored among boys and girls, respectively. showed the ORs and their 95% CIs of risk factors for high normal BP or hypertension. Increasing trends of ORs with aging were found among both genders. However, the absolute changes of ORs were significantly different between boys and girls: before 13 years old, similar changing trend of ORs were showed in two genders, but after 13 years old, ORs increased more for boys than for girls. Compared with their 8-year-old counterparts, 17-year-old boys had a 13.063-fold risk of high normal BP or hypertension but 17-year-old girls had only a 8.700-fold risk. In two logistic models, educational level was closely associated with high normal BP: higher educational level could reduce the prevalence risk compared with primary students. Compared with Hans, Yi and Mongolian boys had a 1.960-fold (1.665–2.307) and 1.283-fold (1.070–1.539) risk of high normal BP or hypertension respectively, and Yi girls had a 1.618-fold (1.387–1.887) risk. Tibetan subjects had just less than half the risk (OR = 0.440, 95% CI 0.342–0.565 for boys, and OR = 0.492, 95% CI 0.391–0.621 for girls) of high normal BP or hypertension compared with Han counterparts. Korean girls had lower risk than Han girls (OR = 0.794, 95% CI 0.659–0.958).
Table III. Risk factors associated with high normal blood pressure or hypertension from multi-logistic regression model.
Overweight and obesity increased prevalence risk greatly in comparison with those with normal weight irrespective of gender. Boys and girls with WC ≥ 90th had a similar increased risk (OR = 1.242, 95% CI 1.063–1.452 for boys and OR = 1.212, 95% CI 1.061–1.384 for girls). Among boys, those with family history of cardiovascular diseases had increased prevalence risk of high normal BP or hypertension (OR = 1.336, 95% CI 1.008–1.772). Rural subjects had an increased risk in comparison to those dwelling at urban areas (OR = 1.154, 95% CI 1.065–1.250 for boys, and OR = 1.210, 95% CI 1.119–1.309 for girls). We did not observe any significant association between smoking and high normal BP or hypertension for both genders (OR = 0.899, 95% CI 0.785–1.029 for boys, and OR = 0.690, 95% CI 0.384–1.239 for girls).
Discussion
This is the first study to comprehensively investigate the prevalence of high normal BP and hypertension in a representative sample of general Chinese adolescents with the largest sample size covering dozens of ethnicities. This facilitated the early detection and early management of pediatric high normal BP and hypertension, as it has been reported that high normal BP and hypertension were frequently undiagnosed in this pediatric population (Citation28).
Based on the popular hypertension and high normal BP standard (the fourth report), we found that the overall prevalence rates were 4.15% for hypertension and 29.85% for high normal BP in Chinese adolescents aged 8–18 years old, which were different from other studies conducted in other parts of the world (Citation11–18). In China, a cross-sectional study with a small sample size from a Chinese northeast rural zone reported the overall prevalence of high normal BP and hypertension was 15% and 20.2% among adolescents aged 5–18 years old (Citation19). Liang et al. found that the prevalence of high normal BP and hypertension increased dramatically from 1991 to 2004, with average relative increases of 6.38% and 8.13% in adolescents aged 6–17 years in China, respectively (Citation29). However, these previous studies were conducted in only a province of China and just included a small sample size, whose results could not represent the real situation of the general adolescent population in this vast country. Furthermore, given that our analysis excluded participants suffering from some severe chronic disease and having a fever in the last 15 days, we believe that the true prevalence of high normal BP and hypertension in general Chinese adolescents would be a little underestimated. In addition, hypertension and high normal BP were defined based on the fourth report in this study. Compared with the European Society of Hypertension (ESH) guidelines in children and adolescents (Citation30), the 90th and 95th percentiles of blood pressure in the fourth report were mostly higher. The higher BP values for 90th and 95th percentiles in the fourth report were expected due to the fact that the Fourth-Report blood pressure references did not exclude overweight children (Citation31). The prevalence of high normal BP and hypertension in this study would be higher if hypertension and high normal BP were defined according to the ESH guidelines.
Consistent with previous studies (Citation13,Citation32–34), we found that the risk of high normal BP and hypertension generally increased with aging in both genders, and after 13 years old, the risk of high normal BP in boys increased more drastically than in girls. China is a multi-ethnic country and people have their specific dietary habits and lifestyles, which could affect their blood pressure status. In this study, the adolescent subjects were ethnically diverse and the prevalence rates of high normal BP and hypertension were statistically different between ethnicities, which was consistent with previous studies (Citation16,Citation17), and so racial differences can influence the prevalence of high normal BP and hypertension.
Adolescents with family history of cardiovascular diseases were found to be associated with higher prevalence risks of high normal BP or hypertension, which was in line with the previous findings (Citation35,Citation36). We did not find any association between smoking and high normal BP or hypertension because only a small portion of adolescents had the habit of smoking. Adolescents dwelling at rural districts had higher prevalence rates maybe because they have not developed more healthy lifestyles than those dwelling at urban districts. The strong association between obesity and pediatric high normal BP was consistent with many previous findings (Citation15–17,Citation37). Furthermore, the present study indicated that obese and overweight boys had larger prevalence risk of high normal BP or hypertension than counterpart girls. The finding among Portuguese school adolescents aged 10–18 also showed a higher risk of being hypertensive among obese and overweight boys than girls (Citation37). Although some reports have mentioned high-salt diet could increase risk for hypertension (Citation38,Citation39), the association of high-salt diet and high normal BP was not statistically significant in the present paper. This may be caused by some reporting bias resulting from the self-reported diet conditions.
Three limitations should be mentioned. First, this is a cross-sectional study and the risk factors found in the present study could not be a considered established cause of high normal BP or hypertension. Second, the definition of hypertension and high normal BP was established based on one visit and further follow-up was not conducted, which might affect the accuracy of diagnosis of hypertension and high normal BP. Finally, reporting bias cannot be avoided because some factors (such as smoking and diet) are self-reported.
In conclusion, a high prevalence rate of pediatric high normal BP and hypertension was general in Chinese adolescents and appropriately one third of subjects were hypertensive or prehypertensive. The prevalence rates of high normal BP and hypertension increased with aging for both genders. In addition, ethnicity, obesity, overweight, abnormal WC, family history of cardiovascular diseases and dwelling at rural districts were significantly associated with pediatric high normal BP or hypertension.
Acknowledgements
The study is supported by the basic performance key project by the Ministry of Science and Technology of the People's Republic of China (No. 2006FY110300).
Declaration of conflicting interests: The authors declare that there is no conflict of interest.
References
- Ikeda A, Iso H, Yamagishi K, Inoue M, Tsugane S. Blood pressure and the risk of stroke, cardiovascular disease, and all-cause mortality among Japanese: The JPHC Study. Am J Hypertens. 2009;22:273–280.
- Schiele F. Renal dysfunction and coronary disease: A high-risk combination. J Nephrol. 2009;22:39–45.
- Whitworth JA. Blood pressure and control of cardiovascular risk. Vasc Health Risk Manag. 2005;1:257–260.
- Redwine KM, Acosta AA, Poffenbarger T, Portman RJ, Samuels J. Development of hypertension in adolescents with pre-hypertension. J Pediatr. 2012;160:98–103.
- Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180.
- Nelson MJ, Ragland DR, Syme SL. Longitudinal prediction of adult blood pressure from juvenile blood pressure levels. Am J Epidemiol. 1992;136:633–645.
- Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: The Bogalusa Heart Study. Am J Hypertens. 1995;8:657–665.
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in adolescents. Pediatrics. 2004;114:555–576.
- Bassareo PP, Mercuro G. Pediatric hypertension: An update on a burning problem. World J Cardiol. 2014;6:253–259.
- Fallah Z, Qorbani M, Motlagh ME, Heshmat R, Ardalan G, Kelishadi R. Prevalence of prehypertension and hypertension in a nationally representative sample of Iranian adolescents: The CASPIAN-IV study. Int J Prev Med. 2014;5: S57–S64.
- Koebnick C, Black MH, Wu J, Martinez MP, Smith N, Kuizon BD, et al. The prevalence of primary pediatric prehypertension and hypertension in a real-world managed care system. J Clin Hypertens (Greenwich). 2013;15:784–792.
- Ellenga Mbolla BF, Okoko AR, Mabiala Babela JR, Ekouya Bowassa G, Gombet TR, Kimbally-Kaky SG, et al. Prehypertension and hypertension among school children in Brazzaville, Congo. Int J Hypertens. 2014;2014:803690.
- Kuciene R, Dulskiene V. Associations of short sleep duration with prehypertension and hypertension among Lithuanian adolescents: A cross-sectional study. BMC Public Health. 2014;14:255.
- Rahman AJ, Qamar FN, Ashraf S, Khowaja ZA, Tariq SB, Naeem H. Prevalence of hypertension in healthy school children in Pakistan and its relationship with body mass index, proteinuria and hematuria. Saudi J Kidney Dis Transpl. 2013;24:408–412.
- Narayanappa D, Rajani HS, Mahendrappa KB, Ravikumar VG. Prevalence of prehypertension and hypertension among urban and rural school going children. Indian Pediatr. 2012;49:755–756.
- Badi MA, Garcia-Triana BE, Suarez-Martinez R. Overweight/obesity and hypertension in schoolchildren aged 6–16 years, Aden Governorate, Yemen,2009. East Mediterr Health J.2012;18:718–722.
- Ostrowska-Nawarycz L, Nawarycz T. Prevalence of excessive body weight and high blood pressure in adolescents in the city of Łódź. Kardiol Pol. 2007;65:1079–1087; discussion 1088–109.
- Akis N, Pala K, Irgil E, Utku AM, Bingol S. Prevalence and risk factors of hypertension among schoolchildren aged 12–14 years in Bursa, Turkey. Saudi Med J. 2007;28: 1263–1268.
- Guo X, Zheng L, Li Y, Yu S, Zhou X, Wang R, et al. Gender-specific prevalence and associated risk factors of prehypertension among rural adolescents in Northeast China: A cross-sectional study. Eur J Pediatr. 2013;172: 223–230.
- Xue J, Wang Y, Li J. Blood pressure and the relevant factors among adolescents aged 7–18 years in Shandong province. Chin J Child Health Care. 2013;21:1142–1144, 1154.
- Qiu X, Ding X, Zhang C, Mao D, Lu X, Jiao Y, et al. Prevalence of hypertension and its associated risk factors among children aged from 6 to 13 years old in Chongqing. J Trop Med. 2013;13:1129–1131.
- Okosun IS, Boltri JM, Anochie LK, Chandra KM. Racial/ethnic differences in prehypertension in American adults: Population and relative attributable risks of abdominal obesity. J Hum Hypertens. 2004;18:849–855.
- Agyemang C, van Valkengoed I, van den Born BJ, Stronks K. Prevalence and determinants of prehypertension among African Surinamese, Hindustani Surinamese, and White Dutch in Amsterdam, the Netherlands: The SUNSET study. Eur J Cardiovasc Prev Rehabil. 2007;14:775–781.
- Chinese guidelines for hypertension prevention and treatment Revision Committee. Chinese guidelines for hypertension prevention and treatment (revised edition 2005). Beijing: People's Medical Publishing House, 2006.
- Group of physical fitness and health research of Chinese school students. Reports of the physical fitness and health research of Chinese school students. Higher Education Press; 2012.
- Group of China Obesity Task Force. Body mass index reference norm for screening overweight and obesity in Chinese adolescents. Chin J Epidemiol. 2004;25:97–102.
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–1243.
- Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in adolescents. JAMA. 2007;298:874–879.
- Liang YJ, Xi B, Hu YH, Wang C, Liu JT, Yan YK, et al. Trends in blood pressure and hypertension among Chinese adolescents: China Health and Nutrition Surveys 1991–2004. Blood Press. 2011;20:45–53.
- Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al. Management of high blood pressure in children and adolescents: Recommendations of the European Society of Hypertension. J Hypertens. 2009;27:1719–1742.
- Lurbe E. Reference blood pressure values in childhood: An issue to be solved. J Hypertens. 2012;30:1911–1912.
- Agyemang C, Redekop WK, Owusu-Dabo E, Bruijnzeels MA. Blood pressure patterns in rural, semi-urban and urban children in the Ashanti region of Ghana, West Africa. BMC Public Health. 2005;5:114.
- Moore WE, Eichner JE, Cohn EM, Thompson DM, Kobza CE, Abbott KE. Blood pressure screening of school children in a multiracial school district: The Healthy Kids Project. Am J Hypertens. 2009;22:351–356.
- Ejike CE, Ugwu CE, Ezeanyika LU, Olayemi AT. Blood pressure patterns in relation to geographic area of residence: A cross-sectional study of adolescents in Kogi state, Nigeria. BMC Public Health. 2008;8:411.
- Sobrino J, Domenech M, Camafort M, Vinyoles E, Coca A; ESTHEN group investigators. Prevalence of masked hypertension and associated factors in normotensive healthcare workers. Blood Press Monit. 2013;18:326–331.
- Chaudhry K, Diwan SK, Mahajan SN. Prehypertension in young females, where do they stand? Indian Heart J. 2012;64:280–283.
- Rebelo D, Teixeira J, Marques-Vidal P, Oliveira JM. Obesity markers and blood pressure in a sample of Portuguese adolescents. Eur J Cardiovasc Prev Rehabil. 2008;15:73–77.
- Montasser ME, Douglas JA, Roy-Gagnon MH, Van Hout CV, Weir MR, Vogel R, et al. Determinants of blood pressure response to low-salt intake in a healthy adult population. J Clin Hypertens (Greenwich). 2011;13:795–800.
- Weidmann P, Ferrari P, Allemann Y, Ferrier C, Shaw SG. Developing essential hypertension: A syndrome involving ANF deficiency? Can J Physiol Pharmacol. 1991;69: 1582–1591.