Abstract
We report a case of hydralazine-induced alveolar hemorrhage and anti-neutrophil cytoplasmic antibody (ANCA)-positive pauci-immune glomerulonephritis, with serum anti-histone antibodies present, features not previously described in the literature with this drug. A 50-year-old Caucasian female had hypertension treated with hydralazine 75mg TID for three years, and a lung nodule followed up periodically with chest-computed tomographies. She was admitted to the hospital for hemoptysis and newly discovered diffuse pulmonary ground-glass opacities. Transbronchial lung biopsy showed alveolar hemorrhage. Serum creatinine was 3.5 mg/dL and urinalysis showed 2+blood, 30-50RBC/hpf and red blood cell casts. ANCA against myeloperoxidase were present. Anti-double-stranded DNA, ANA, and anti-histone antibodies were positive. Serum complements were normal. Renal biopsy revealed focal crescentic necrotizing glomerulonephritis with negative immunofluorescence, consistent with pauci-immune ANCA-positive vasculitis. Serum creatinine returned to baseline three days after hydralazine was discontinued, and the hemoptysis resolved after treatment with cyclophosphamide and prednisone was started. We concluded that this case represents a hydralazine-induced small vessel vasculitis rather than an idiopathic one. The possibility of hydralazine-induced vasculitis should be considered when patients treated with hydralazine develop a pulmonary-renal syndrome. Anti-histone antibodies may be present in the absence of full classification criteria of drug-induced lupus.
CASE REPORT
A 50-year-old Caucasian female with hypertension, ischemic cardiomyopathy, two drug eluting stents, an implantable cardioverter defibrillator, and chronic kidney disease stage III was followed up periodically with chest computed tomographies for a lung nodule, incidentally discovered three years earlier. She was admitted to the hospital for elective bronchoscopy after newly discovered diffuse pulmonary ground glass opacities. For the prior three years, the patient had been treated with hydralazine 75 mg three times daily, lisinopril 5 mg daily, isosorbide mononitrate 30 mg daily, digoxin 0.125 mg daily, torsemide 5 mg daily, metoprolol succinate 25 mg daily, aspirin 81 mg daily, clopidogrel 75 mg daily, and atorvastatin 80 mg daily.
Upon admission, the patient reported mild cough with blood tinged sputum, which were present for seven days. She denied fever, malaise, weight loss, skin rash, nasal congestion, myalgia, arthralgia, dysuria, and hematuria. The physical examination revealed bilateral dry crackles on lung auscultation, but was otherwise unremarkable. Bronchoscopy with lung biopsy revealed diffuse alveolar hemorrhage and was otherwise non-diagnostic. Admission serum creatinine was 3.55 mg/dL (baseline 1.8–2 mg/dL), and the urinalysis showed 2+ blood. Examination of the urine sediment showed a red blood cell cast and 30–50 red blood cells per high power field. Serological studies showed positive perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA), titer 1:320, with strongly positive anti-myeloperoxidase (MPO) antibodies (97 U/mL) and weakly positive anti-proteinase 3 (21 U/mL). Anti-histone, antinuclear (ANA), and anti-double stranded deoxyribonucleic acid (DNA) antibodies were also positive (105 AU/mL [0–99], 1:320, homogeneous pattern and 58.8 IU/mL [positive >35], respectively).
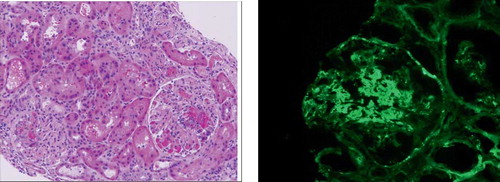
Complement C3 and C4 were normal. Subsequently, a kidney biopsy revealed focal and segmental necrotizing glomerulonephritis with crescents (<50%), with negative immuno-fluorescence, consistent with pauci-immune ANCA positive vasculitis (see and ).
Figure 1. (a) Hematoxylin and eosin stain. Segmental endocapillary cellular proliferation (black arrow) and foci of tuft necrosis (white arrow). (b) Immunofluorescent microscopy. Focal glomerular C3 staining is evident in the mesangium.
Hydralazine was discontinued, and the patient began immunosuppressive therapy with cyclophosphamide and prednisone. The serum creatinine level returned to baseline within three days and hemoptysis resolved within several days.
DISCUSSION
Hydralazine has been often reported to cause ANCA positive pauci-immune glomerulonephritis, but concomitant lung involvement is extremely rare.Citation[1–6] There are very few cases reported in which both renal and pulmonary structures were involved.Citation[3–6] We report a case of hydralazine-induced alveolar hemorrhage and ANCA-positive pauci-immune glomerulonephritis, with serum anti-histone antibodies present, features not previously described in the literature with this drug.
The etiology of most cases of ANCA-positive pauci-immune glomerulonephritis remains unknown.Citation[7] Moreover, the pathophysiology of drug-induced glomerular form is also ill-defined.Citation[8] Almroth et al. suggest that because ANCAs react with antigens in the cytoplasm of neutrophils and monocytes, the presence of anti-MPO and ANCA in patients with hydralazine-associated nephritis may indicate that leukocyte antigens are involved in the pathogenesis of the renal damage.Citation[3] When hydralazine is suspected of being the culprit, the temporal relationship between the discontinuation of the medication and the improvement in renal function is strongly suggestive of a drug-induced disease.Citation[9]
Hydralazine may be associated with two clinical autoimmune syndromes: hydralazine-induced lupus and hydralazine-induced ANCA-associated vasculitis. Several risk factors for drug-induced lupus have been identified: the drug dose (more than 200 mg/day and/or a cumulative dose of more than 100 g), female sex, slow hepatic acetylation, HLA-DR4 genotype, and the null gene for the fourth component of the complement, C4.Citation[10,11] The presence of drug-induced lupus should be strongly suspected when a lupus-like syndrome develops in a patient taking hydralazine and has antihistone antibodies present, in the absence of other autoantibodies.Citation[9] Kidneys are usually spared in drug-induced lupus; however, an immune complex glomerulonephritis identical with that seen in the classical systemic lupus erythematosus has been reported.Citation[12]
Studies of hydralazine-induced ANCA-positive glomerulonephritis have underlined the utility of MPO antibodies in the diagnosis of drug-induced vasculitis.Citation[5,13–15]
An extensive review of the literature shows only twelve patients with ANCA-positive hydralazine-associated vasculitis with both kidney and lung involvement (see ). The hydralazine dose ranged from 50 to 200 mg per day, and the treatment duration varied from 1 to 14 years. Almost all patients had MPO antibodies present, but none had anti-histone antibodies reported. The latter are thought to represent an autoimmune response directed against histone DNA complexes triggered by hydralazine metabolites in susceptible individuals.Citation[4]
Table 1 Hydralazine-associated ANCA-positive pauci-immune glomerulonephritis
Anti-histone antibodies have been described in a number of autoimmune diseasesCitation[9] but never before in association with pauci-immune glomerulonephritis.
The presence of antihistone antibodies and hydralazine use would suggest drug-induced lupus.Citation[9,16] However, the renal involvement in drug-induced lupus is rare (only 5% of the cases), while arthritis and arthralgia are present in 95% of the cases. In addition, serum antibodies other than ANA and anti-histone antibodies are rarely encountered.Citation[9] Our patient did not fulfil the American Rheumatism Association criteria for systemic lupus erythematosus, and did not have symptoms typical of drug-induced lupus.
Review of the literature shows that hydralazine-associated ANCA-positive vasculitis patients with lung involvement may have lung infiltrates or nodules, with or without lung hemorrhage,Citation[5] respiratory symptoms, hemoptysis, and pleuritis.Citation[3] None of the studies reported any lung biopsies. Our patient presented with hemoptysis and had a chest CT showing reticulo-nodular pattern and a transbronchial biopsy revealing alveolar hemorrhage, but no vasculitis.
CONCLUSION
Based on the clinical presentation, laboratory data, and kidney biopsy findings, we concluded that this case represents a hydralazine-induced small vessel vasculitis rather than an idiopathic one. Ultimately, regardless of the etiology, treatment includes both steroids and cytotoxic therapy (i.e., cyclophosphamide).
The differential diagnosis of pulmonary renal syndrome should include hydralazine-associated small vessel vasculitis in patients treated with this medication. Anti-histone antibodies may be present in the absence of full classification criteria of drug-induced lupus.
DECLARATION OF INTEREST
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Nassberger L, Johansson AC, Bjorck S, Sjoholm AG. Antibodies to neutrophil granulocyte myeloperoxidase and elastase: Autoimmune responses in glomerulonephritis due to hydralazine treatment. J Intern Med. 1991;229(3):261–265.
- Peacock A, Weatherall D. Hydralazine-induced necrotizing vasculitis. BMJ. 1981;282:1121–1122.
- Almroth G, Enestrom S, Hed J, Samuelsson I, Sjostrom P. Autoantibodies to leucocyte antigens in hydralazine-associated nephritis. J Intern Med. 1992;231(1):37–42.
- Cambridge G, Wallace H, Bernstein RM, Leaker B. Autoantibodies to myeloperoxidase in idiopathic and drug-induced systemic lupus erythematosus and vasculitis. Br J Rheumatol. 1994;33(2):109–114.
- Choi HK, Merkel PA, Walker AM, Niles JL. Drug-associated antineutrophil cytoplasmic antibody-positive vasculitis: Prevalence among patients with high titers of antimyeloperoxidase antibodies. Arthritis Rheum. 2000;43(2):405–413.
- Short AK, Lockwood CM. Antigen specificity in hydralazine associated ANCA positive systemic vasculitis. Q J Med. 1995;88:775–783.
- Savige J, Davies D, Falk RJ, Jennette CJ, Wiik A. Antineutrophil cytoplasmatic antibodies and associated diseases: A review of the clinical and laboratory features. Kidney International. 2000;57:846–862.
- Ten Holder SM, Joy MS, Falk RJ. Cutaneous and systemic manifestations of drug- induced vasculitis. Ann Pharmacother. 2002;36:130–147.
- Hess E. Drug-induced lupus. N Engl J Med. 1988;318:1460.
- Speirs C, Fielder AH, Chapel H, Davey NJ, Batchelor JR. Complement system protein C4 and susceptibility to hydralazine-induced systemic lupus erythematosus. Lancet. 1989;1(8644):922–924.
- Batchelor JR, Welsh KI, Tinoco RM, Hydralazine-induced systemic lupus erythematosus: Influence of HLA-DR and sex on susceptibility. Lancet. 1980;1(8178):1107–1109.
- Ihle BU, Whitworth JA, Dowling JP, Kincaid-Smith P. Hydralazine-associated glomerulonephritis. Clin Nephrol. 1984;22:230–238.
- Merkel PA. Drugs associated with vasculitis. Curr Opin Rheumatol. 1998;10(1):45–50.
- Nassberger L, Sjoholm AG, Jonsson H, Autoantibodies against netrophil cytoplasm components in systemic lupus erythematosus and in hydralazine-induced lupus. Clin Exp Immunol. 1990;81:380.
- Ohtani H, Wakui H, Komatsuda A, Differences between myeloperoxidase-specific and nonspecific P‐ANCA-associated renal disease. Ren Fail. 2007;29(2):183–187.
- Burlingame RW, Rubin RL. Drug-induced anti-histone autoantibodies display two patterns of reactivity with substructures of chromatin. J Clin Invest. 1991;88(2):680–690.
