Abstract
Background: Benign monoclonal gammopathy (MG) is an MG that is not accompanied by clinical manifestations of plasma cell dyscrasia, such as multiple myeloma, macroglobulinemia, amyloidosis, or other related disorders. Benign MG can progress to malignancy, but seldom causes organ damage. Case report: We presented a case denied any underlying disease who visited our hospital as acute uremia syndrome. Laboratory data indicated renal failure and abnormal paraprotein in the serum and urine. Renal biopsy indicated acute tubular necrosis and cast in the renal tubule. The plasma cell counts were normal in his bone marrow biopsy. The patient had received maintenance hemodialysis for the irreversible renal failure. Conclusion: Benign MG might progress to malignancy or other related disorders in a risk of 1% per year. It also might cause secondary organ impairment, such as kidney.
INTRODUCTION
Monoclonal gammopathy (MG) is the presence of excessive levels of paraprotein (a monoclonal gamma globulin) in the serum. Benign MG can progress to malignancy, but seldom causes organ damage, such as kidney.Citation1 The most common monoclonal plasma cell disorders are monoclonal gammopathy of undetermined significance (MGUS), multiple myeloma, smoldering multiple myeloma (SMM), light chain (AL) amyloidosis, and Waldenström macroglobulinemia.Citation1 Diagnosis of benign MG is important so that potentially harmful therapies, such as chemotherapy, are not administered.
CASE REPORT
A 74-year-old man was admitted to our hospital on 26 August 2008 because of poor appetite and general weakness. He visited our emergency department where laboratory tests indicated elevated serum creatinine (16.85 mg/dL), slightly elevated potassium (5.8 mEq/L), and metabolic acidosis with respiratory alkalosis.
On the day of admission to our hospital, renal sonography indicated acute renal parenchymal disease. Urinalysis revealed proteinuria (25 mg/dL) and the presence of occult blood. The rate of protein loss in the urine was 999 mg/day.
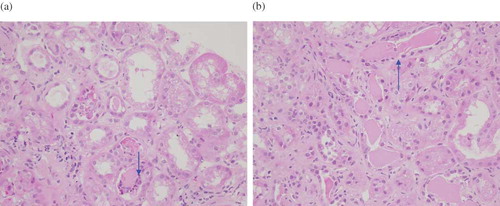
We performed a renal biopsy and the biopsy report indicated acute tubular necrosis with the presence of casts surrounded with macrophage in the renal tubules ( and b).
FIGURE 1. (a) The casts are surrounded by mononuclear cells, multinucleated giant cells, and neutrophils (hematoxylin and erosin stain, ×400). (b) A low-magnification photograph depicts large eosinophilic hyaline casts in the dilated tubular lumina (hematoxylin and eosin stain, ×400).
Blood electrophoresis indicated an M spike at the mid-γ region and urine electrophoresis with M spike at free light chains; immunofixation electrophoresis indicated MG with free kappa-light chains. The bone marrow biopsy indicated less than 20% increased plasma cells. A skull X-ray was negative for puncture lesion. Finally, we diagnosed the patient as having MGUS accompanied by kidney involvement. The patient remained on hemodialysis schedule for the irreversible acute kidney injury (AKI). Therefore, we would classify our patient as having benign MG with kidney damage, but no malignancy.
DISCUSSION
Plasma cell dyscrasias that involve renal function are mostly seen in patients with multiple myeloma (18–56%), cryoglobulinemic glomerulonephritis (16.5%), immunoglobulin light chain amyloidosis (5–11%), or light chain deposit disease (3–5%).Citation1 Aside from multiple myeloma, the presence of monoclonal paraprotein associated with abnormal kidney function is rare.
Based on the laboratory data and renal biopsy of this patient (marrow plasmacytosis < 20%, no lytic bone lesion, no serum M component > 3 g/dL, daily protein loss in the urine of 0.999 g/day, no presence of Bence-Jones protein in the urine), there was no indication of multiple myeloma or SMM. We excluded light chain deposit disease because there was no deposit of kappa light chain in immuno-fixative electrophoresis and the renal biopsy indicated negative staining of the κ-light chain and λ-light chain deposition. We also excluded light chain amyloidosis (a disease characterized by amyloid fibril deposits in multiple organs including the heart, kidney, and liver) because there was no deposition of light chain and the Congo-red stain was negative for amyloidosis.
The criteria for MGUS is monoclonal component <3 g/dL, no urinary Bence-Jones protein, marrow plasmacytosis <10%, no lytic bone lesion, anemia, hypercalcemia, or renal insufficiency. Our patient did not have a malignant gammopathy, such as multiple myeloma, Waldenström's macroglobulinemia, or chronic lymphocytic leukemia. However, he clearly had MG and renal disease in sustained loss stage and anemia (possibly a consequence of renal disease). Thus, we diagnosed our patient as having renal disease and MG of uncertain significance.
Ramos and PovedaCitation2 reported a patient with hematuria, proteuria, and renal failure with serum and urine immunofixation with a monoclonal component consisting of μ and κ chains. However, this patient's bone marrow biopsy was negative; his renal biopsy indicated subendothelial deposits of IgM, C3, and κ-type light chains. In an earlier report, Lima et al.Citation3 reported a patient who presented with bilateral pitting edema in the lower legs. Serum and urine electrophoresis indicated homogenous IgM-κ chains, but no paraprotein deposit in bone marrow and the kidney. In a case series of nine patients, Ramos et al.Citation4 concluded that the benign nature of MG does not exclude the possibility that it may lead to secondary renal impairment. Therefore, we would classify our patient as having benign MG with end organ damage, but no malignancy.
There are a few reports of MGUS that accompanied renal impairment, but most of these were associated with Fanconi syndrome,Citation5–9 in which there is no paraprotein deposit accompanying the renal failure. In our case, the kidney biopsy indicated no deposition of paraprotein but clear evidence of myeloma kidney. The poor renal function of our patient may have been due to the co-occurrence of myeloma kidney and MGUS.
In a case series of nine patients,Citation4 Ramos et al. concluded that the benign nature of MG does not exclude the possibility that it may lead to secondary renal impairment, with a 5-year survival rate of about 37%. Chemotherapy stabilizes or improves the renal function of 33% of patients with non-malignant MG.Citation4
Therefore, we would classify our patient as having benign MG-associated AKI, but no malignancy.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Leung N, Rajkumar SV. Renal manifestations of plasma cell disorders. Am J Kidney Dis. 2007;50:155–165.
- Ramos R, Poveda R. Renal involvement in non-malignant IgM gammopathy. Nephrol Dial Transplant. 2007;22:627–630.
- Lima J, Monteagudo M, Valles M, Garcia-Bragado F, Carrera M, Vilardell M. Proliferative endo- and extracapillary glomerulonephritis and benign monoclonal IGM gammopathy. Nephron. 1990;56:457–458.
- Ramos R, Poveda R, Bernís C, Renal involvement in benign monoclonal gammopathies: An underdiagnosed condition? Nefrologia. 2008;28:525–530.
- Kagaya M, Takahashi H. A case of type I cryoglobulinemia associated with a monoclonal gammopathy of undetermined significance (MGUS). J Dermatol. 2005;32:128–131.
- Ma CX, Lacy MQ, Rompala JF, Acquired Fanconi syndrome is an indolent disorder in the absence of overt multiple myeloma. Blood. 2004;104:40–42.
- Hashimoto T, Arakawa K, Ohta Y, Acquired Fanconi syndrome with osteomalacia secondary to monoclonal gammopathy of undetermined significance. Intern Med. 2007;46:241–245.
- Kobayashi T, Muto S, Nemoto J, Fanconi's syndrome and distal (type 1) renal tubular acidosis in a patient with primary Sjogren's syndrome with monoclonal gammopathy of undetermined significance. Clin Nephrol. 2006;65:427–432.
- Nagao T, Okura T, Miyoshi K, Fibrillary glomerulonephritis associated with monoclonal gammopathy of undetermined significance showing lambda-type Bence Jones protein. Clin Exp Nephrol. 2005;9:247–251.
