Abstract
Objective: Initial high peritoneal permeability in peritoneal dialysis (PD) patients was previously thought to be a poor prognostic factor. We aimed to study the factors that determine the initial transport status and prognosis in PD patients. Methods: This was an observation cohort study that enrolled 551 fresh uremic patients who commenced PD in a single PD center from January 1994 to December 2004. Patients with different initial peritoneal transport status were analyzed and determinants of the initial peritoneal transport status were evaluated. All patients were followed up to investigate the risks of mortality. Results: At the start of PD, only age and sex were determinants of the initial peritoneal transport status upon multiple linear regression analysis. The average duration of the study follow-up was 45.4 ± 29.4 months. In the follow-up, a regression toward mean of transport status was found. About 107 patients died during the observation period. Cox-multivariate analysis revealed only age (RR = 1.06, p < 0.001), comorbidity index (RR = 2.31, p < 0.001), serum albumin (RR = 0.58, p = 0.008), and percentage of lean body mass (RR = 0.97, p = 0.008) to be independent predictors of mortality. Conclusion: We observed that the initial peritoneal transport status is not a determinant factor of long-term mortality. The reason may be due to a consequence of regression toward mean of the transport status. Whether the observed longitudinal regression-to-mean phenomenon change represent any physiologic relevance is hard to define. Further studies on the underlying mechanisms are needed.
INTRODUCTION
Since the peritoneal equilibration test (PET) was first developed by Twardowski et al. in 1987, it has been used widely as a valuable tool for categorizing and monitoring functional changes in peritoneal membrane function.Citation1 High transporters undergo better clearance during dialysis but have poor ultrafiltration (UF) due to rapid absorption of glucose from the peritoneum and dissipation of the osmotic gradient. They (high transporters) would benefit from frequent short-duration dwells, whereas low transporters would benefit from long-duration, high-volume dwells. Different dialysis prescription strategies would prevent most patients of all transport types from either fluid overload or inadequate dialysis. However, several reports have suggested that a high peritoneal transport status is associated with a poor patient outcome.Citation2–4 Data from the CANUSA study indicated that high solute transporters are associated with a greater risk of combined technique failure and mortality.Citation2 Recently, Rumpsfeld et al. showed that a high peritoneal transport status is a very significant independent risk factor for mortality in peritoneal dialysis (PD) patients from Australia and New Zealand.Citation4 The definite reasons for this are unclear. One possible explanation is that a high peritoneal transport status is associated with a decrease in UF capacity, leading to UF failure in the worst affected patients.Citation5 Alternatively, a high transport status may be a marker of comorbidity, malnutrition, or inflammation.Citation6,Citation7 It may be that the poor prognosis associated with a high peritoneal transport status may relate more to these factors. Contrary to the above-mentioned studies, some studies demonstrated that a high peritoneal transport status by itself is not an independent risk factor for mortality.Citation7–10
The peritoneal transport rate is known to change over time in PD. Nevertheless, the reports on longitudinal changes in the peritoneal transport rate are diverse. Davies et al. reported that there is a gradual increase in the small solute transport status over the years with reduction in the UF capacity.Citation5 However, some groups have shown that longitudinal changes in the peritoneal permeability follow a centripetal or regression toward mean pattern, which may be beneficial to baseline high transporters by increasing UF.Citation11–13
In the present study, we analyzed the pattern of changes in peritoneal transport status over time in our PD patients. We also investigated the determinants of initial peritoneal transport status and its relevance with the prognostic factors.
MATERIAL AND METHOD
This clinical study was conducted in accordance with the Declaration of Helsinki and was approved by the Medical Ethics Committee of the Chang Gung Memorial Hospital (CGMH), Taipei.
This was a single-center observation cohort study that included 551 fresh uremic patients who commenced continuous ambulatory peritoneal dialysis (CAPD) in CGMH from January 1994 to December 2004. Patients that were ≥18 years of age and who underwent PD for more than 3 months were included. None of the patients had performed the test within the 2 months after diagnosis of peritonitis. Baseline data, including age, sex, body weight, body height, cause of end-stage renal disease, presence of diabetes mellitus (DM), and other comorbid diseases, were collected. Baseline PET was performed, using the 4 h standard method, within 3 months of commencing CAPD and repeated at least yearly or when changes were suspected.
The evaluation of comorbid diseases was done according to the categories used by Chung et al.Citation3 Cardiovascular diseases included previous and present history of congestive heart failure, ischemic heart disease, or cerebrovascular disease. Respiratory diseases were defined as active tuberculosis, chronic lung disease, or asthma attacks. Liver diseases included persistently elevated serum glutamic-pyruvic transaminase and serum glutamic-oxaloacetic transaminase or cirrhosis defined by abdominal echo and clinical symptoms. Systemic diseases included DM and systemic lupus erythematosus (SLE). The comorbidity was graded by the Davies index.Citation14 The comorbidity score of each patient was the number of comorbid diseases; grade 0 (low risk) is a 0 score, grade 1 (medium risk) is a score of 1–2, and grade 2 (high risk) is a score of ≥ 3.
Patients were categorized into one of the four peritoneal transport types according to the 4 h dialysate-to-plasma ratio of creatinine on the initial PET defined by Twardowski.Citation1 Briefly, a 4 h dwell study was performed using a 2 L exchange with a 2.27% glucose solution. We measured dialysate glucose and creatinine levels at 0, 2, and 4 h, and plasma glucose and creatinine levels at 2 h. The creatinine values in the dialysate were corrected for glucose interference before further calculation. The dialysate-to-plasma ratio of creatinine (D/P Cr) at 0, 2, and 4 h, the ratio between the glucose level in the dialysate effluent and that in the infused dialysate [(D/D0)G], and the UF volume at 4 h were also calculated.
The 24 h urine and drained dialysate were obtained to calculate the residual renal function (RRF), the weekly normalized creatinine clearance (Ccr), and the normalized whole body urea clearance (Kt/V urea). Both parameters Ccr and Kt/V urea were calculated for the kidney, peritoneum, and kidney + peritoneum.
Serum albumin concentration, the percentage of lean body mass (%LBM), and normalized protein equivalent of total nitrogen appearance (nPNA) were used as markers of nutrition. Serum albumin was determined by the bromocresol green method. The %LBM was determined from creatinine kinetics according to Forbes and Bruining and normalized to body weight.Citation15 The protein equivalent of nitrogen appearance (PNA) was derived from the urea generation rate using the formula proposed by Bergstrom et al. and was normalized to the ideal body weight of the patients.Citation16
Finally, all PET reports of the 551 patients in this observation period were collected and longitudinal changes in peritoneal transport status were analyzed. The endpoint of the study was the patient status (dead or alive) or termination of the follow-up period (December 2006). Data for patients who had transferred to hemodialysis or who had received renal transplantation were censored.
STATISTICAL ANALYSIS
Results are expressed as mean ± SD for continuous data and as frequencies and percentages for categorical data. The difference in clinical characteristics between different transporter groups was evaluated by one-way analysis of variance (ANOVA) using the Bonferroni test for post hoc analysis. Chi-square test or Fisher's exact test was used to compare the nominal variables between different transporter groups. This investigation utilized simple linear regression (SLR) analysis for demographic, biochemical, and other variables to identify factors associated with the peritoneal transport status. Significant factors were subjected to a multiple linear regression analysis with a backward-stepwise selection procedure to identify factors that are independent determinants of peritoneal transport status.
Survival analysis was done using the Kaplan–Meier method. A log-rank was used to compare the different survival curves. The Cox proportional hazard model was used to identify factors determining patient mortality. The major statistics were calculated on a personal computer using SPSS (version 16.0). Significance was considered at a p value of <0.05.
RESULTS
Clinical characteristics of the four transport groups
A total of 551 patients were studied, and there was a preponderance of female patients (61.5%). The mean age of the patients at the start of PD was 48.2 ± 14.5 years. The primary diagnosis of renal failure was chronic glomerulonephritis (n = 130, 23.6%), DM nephropathy (n = 98, 17.8%), hypertension (n = 64, 11.6%), small kidneys/unknown (n = 193, 35.0%), SLE (n = 18, 3.3%), and other causes (n = 48, 8.7%). The initial PET was performed at a mean of 57.5 ± 21.5 days from the start of PD.
When patients were categorized by their baseline peritoneal transport status, 52 patients (9.4%) were classified as high peritoneal transporters (H group), 271 patients (49.2%) as high-average transporters (HA group), 204 patients (37%) as low-average transporters (LA group), and 24 patients (4.4%) as low transporters (L group). The mean D/P Cr was 0.86 ± 0.05, 0.71 ± 0.04, 0.59 ± 0.04, and 0.43 ± 0.06 for the H, HA, LA, and L groups, respectively.
The main characteristics according to the peritoneal transport status are summarized in . Patients in H group were older than those in LA group with no difference when compared to other groups. The proportion of male patients in H group was more than those in L group but not significantly different when compared with HA and LA groups. We observed lower serum Cr, albumin, and net drained volume in H group. The presence of DM and comorbidity in all groups were similar. Although nPNA was statistically different among all groups (p = 0.045), we did not find a significant difference between each transport status using the Bonferroni test for post hoc analysis. Compared with H group and HA group, the LA group had higher peritoneal clearance as determined from the Kt/V value. The RRF was low in the L group but did not reach statistical significance when compared to the H group. There was no statistical difference among the four transport groups with regard to body weight, body mass index, kidney and total weekly Kt/V, and %LBM.
TABLE 1. Baseline characteristics of the patients according to peritoneal transport type (n = 551)
SLR analysis of variables related to D/P Cr revealed that age, sex, nPNA, and RRF were associated with D/P Cr. After adjusting for the above-mentioned significant variables via backward-stepwise multiple linear regression analysis, only age and sex were determinants of the initial peritoneal transport status ().
TABLE 2. Determinants of baseline D/P Cr in patients on peritoneal dialysis
Centripetal change of peritoneal transport status
The analysis of longitudinal changes in the solute transport status over time is shown in . We did not observe a change in D/P Cr over time among the entire study population. We further assessed the longitudinal changes in the solute transport status over time according to the baseline peritoneal transport status (). Patients with an initially high peritoneal transport status had a trend toward negative changes, while those with an initially low status had positive changes, which showed a centripetal pattern.
Clinical outcome and predictors of patient survival
During the study period from January 1994 to December 2006, there were 107 (19.4%) deaths. The average duration of the study follow-up was 45.4 ± 29.4 months. The causes of death were peritonitis (12.1%), nonperitonitis infection (41.1%), cardiovascular disease (25.2%), malignancy (1.9%), others (7.5%), and unknown (12.1%).
Among the remaining study patients, 239 patients (43.4%) were still on PD, 126 patients (22.9%) changed to hemodialysis, 46 patients (8.3%) received renal transplantation, and 32 patients (5.8%) had been transferred to other dialysis units. Of the 126 patients who transferred to hemodialysis, 9 patients were in the H group (n = 52, 7.1%), 55 patients were in the HA group (n = 271, 43.7%), 54 patients were in the LA group (n = 204, 42.9%), and 8 patients were in the L group (n = 24, 33.3%). High transport status had the least patient to transfer to HD.
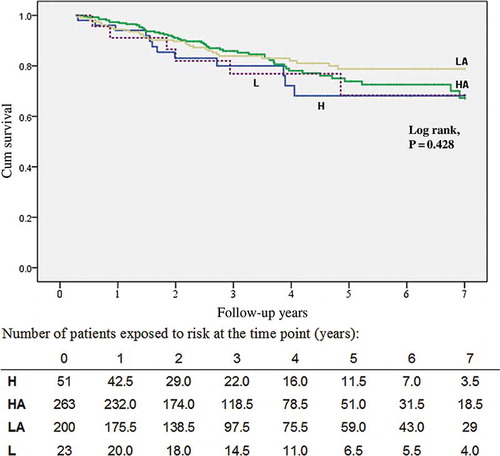
Of the 107 patients who died, 13 patients were in the H group (n = 52, 25.0%), 53 patients were in the HA group (n = 271, 19.6%), 35 patients were in the LA group (n = 204, 17.2%), and 6 patients were in the L group (n = 24, 25%). At the end of 1, 4, and 7 years, actuarial patient survival rates, respectively, were 94, 73, and 68% in the H group; 97, 78, and 68% in the HA group; 94.5, 82, and 78% in the LA group; 91, 77, and 70% in the L group. Kaplan–Meier analysis revealed that there was no significant difference in the cumulative patient survival rate between the groups (p = 0.428, ).
FIGURE 3. Patient survival curves. L, low transporter; LA, low-average transporter; HA, high-average transporter; H, high transporter.
Predictors of mortality and relative risk (RR) in the 551 patients are shown in . Age, increased comorbidity index, decreased serum Cr and albumin levels, lower nPNA, and %LBM at baseline were associated with a significant reduction in patient survival in the univariate analysis. Gender, net drained volume, and peritoneal transport rate, which were analyzed as continuous variables (D/P Cr), were not prognostic factors for long-term mortality in PD patients. Cox-multivariate analysis showed that only age (RR = 1.06, CI: 1.05–1.08, p < 0.001), comorbidity index (RR = 2.31, CI: 1.76–3.03, p < 0.001), serum albumin (RR = 0.58, CI: 0.39–0.87, p = 0.008), and %LBM (RR = 0.97, CI: 0.96–0.99, p = 0.008) were independent predictors of mortality.
TABLE 3. Cox regression analysis of the overall risk of all-cause mortality according to baseline prognostic factors in maintenance PD patients (n = 551)
DISCUSSION
Our study demonstrated that initial peritoneal membrane permeability, analyzed as either a categorical variable (H, HA, LA, and L transport status) or a continuous variable (D/P Cr), was not a risk factor for short-term or long-term mortality in PD patients. The main predictors of long-term mortality in our study were age, comorbidity index, serum albumin, and %LBM.
In our analysis, the determinant of a high initial peritoneal transport status was age and sex. The relation between age and transport rate was demonstrated in several studiesCitation2,Citation3,Citation14; the reason for this is not clear and some reports have suggested a collinear relationship with comorbid disease.Citation14 The finding of a higher proportion of male patients in the high transporter group was also similar to the findings of some earlier investigations.Citation14,Citation17,Citation18 The reason for this is also undetermined. Chung et al.Citation17 reported a correlation with more comorbid diseases in male patients. However, contrary to the finding of previous studies, the presence of DM and comorbid diseases was not associated with the high transport status in our study. Further study on inflammation state or uremic toxin at the start of PD may solve this question in our PD patients.
Our finding on the relationship between the peritoneal transport status and patient survival was similar to some of the findings reported earlier.Citation7–10,Citation19 Recently, Yang et al.Citation20 also demonstrated that the actuarial patient survival rates at the end of 1, 3, and 5 years were not significantly different among the different transport groups (p = 0.780). However, several studies suggested a relationship between higher peritoneal transport rates and poor patient survival.Citation2–4 The largest examination to date is a prospective, multicenter study by Rumpsfeld et al., which included 3702 incident PD patients.Citation4 Nevertheless, in their subgroup analysis, according to the type of PD therapy prescribed, a high transport status was not an independent predictor of mortality for patients who received automated peritoneal dialysis (APD). These results are in accordance with the European Automated PD Outcome Study (EAPOS),Citation9 which found that survival was not influenced by the peritoneal transport status in 177 anuric patients who received APD. One possible explanation for these results is that the APD may possibly eliminate the clinical consequence of an inadequate UF due to a high transport status. As such, these results suggested that the poor outcome associated with a high transport status may relate more to fluid overload over time rather than a high transport status per se.
In our cohort study, the penetration rate of APD is 13.4% and the number of patients on APD in H group was least (n = 1, 1.9%), making this very unlikely to be a significant confounding factor. This result in combination with the present study allows consideration of the possibility that the longitudinal change in the peritoneal transport status may be the reason for the favorable outcome in our PD patients with a high baseline transport status. In a retrospective, 7-year cohort study, Hung et al. found that patients with a higher initial D/P Cr tended to have larger decreases in their final D/P Cr and vice versa.Citation12 Similarly, Raj et al. also observed that there was a tendency for the extreme transport categories to move to the average group.Citation21 Although some studies had different results on the longitudinal change of peritoneal membrane properties,Citation5,Citation22 our finding is consistent with this centripetal pattern. The mechanisms that cause the change in the peritoneal permeability over time are still unknown. Wong et al. showed the observed centripetal change in D/P Cr is likely a bias observation reflecting a “regression toward mean” phenomenon without physiologic relevance.Citation13 Whether the observed change has any biological effect is difficult to define and some investigators considered that both phenomena are in fact occurring.Citation12,Citation14 It has been recognized that the peritoneal membrane permeability may alter in several clinical conditions such as DM, peritonitis, inflammation states, and other treatment-related factors. Whether the change in our PD patients is related to correction of the uremia and inflammation state needs to be demonstrated in the future.
The clinical outcome of PD may be influenced by many factors other than the peritoneal transport status. In our study, the two most significant predictors among these were serum albumin (RR = 0.58, CI: 0.39–0.87, p = 0.008) and comorbidity index (RR = 2.31, CI: 1.76–3.03, p < 0.001). Lower serum albumin has long been regarded as a significant risk factor of poor outcome in PD patients.Citation2,Citation6,Citation19,Citation23–25 In addition to its association with malnutrition, a lower serum albumin level was correlated with other clinical conditions, for example, more comorbidities, inflammation state, and fluid overload, which are, in fact, increasing mortality.Citation7,Citation19,Citation26 Not surprisingly, the presence of comorbidity at commencement of PD was a significant predictor of long-term mortality in our study population. It has been suggested that a high transport status and low serum albumin are the common consequences of an underlying comorbidity, which may be the real cause of the poor outcome.Citation27
It must be taken into consideration that some of these above-mentioned determinants interact with each other. It has been argued that a parameter like albumin should not be included in the survival analysis as it is not a true baseline value, but rather a possible consequence of high peritoneal transport status.Citation14 However, D/P Cr is still not a risk factor of long-term mortality upon alternative Cox regression analysis, excluding either serum albumin or %LBM in our study (data not shown).
There are several limitations in this study. First, the lack of relationship between transporter status and mortality as a consequence of “regression toward mean” may only be a survival bias observed in patients who survived long enough to have a change in their transporter status. However, transport status, which was analyzed as continuous variables (D/P Cr), was not a prognostic factor for short-term mortality (in the first year) in the univariate (p = 0.593) and multivariate analysis (p = 0.195). Second, in our study, the proportion of female patients was high (61.5%), and the mean age was 48.2 ± 14.5 years. It is a relatively distinct group as compared to groups in several previous large studies. Another characteristic of our study group was that the incidence of DM was lower than that reported previously, for example, the CANUSA studyCitation2 and data from Rumpsfeld et al.Citation4 (17.8 vs. 30.6% and 38.1%, respectively). Because the study was conducted at a single center and the analysis was of retrospective nature, the potential of selection bias is present. Third, deaths within a period of time after conversion to long-term hemodialysis were not included in our analysis, which might be an indirect consequence of PD. Fourth, the peritoneal transport status is a time-dependent covariable and using the baseline D/P Cr in the Cox regression analysis could not answer the real impact of average peritoneal transport status on patient mortality, thus warranting further study.
In conclusion, in our PD patients, the initial peritoneal transport status was not a determinant factor of long-term mortality. This result indicated that a high baseline peritoneal transport status may not be regarded as a critical problem as was previously thought. Instead, low serum albumin and a higher comorbidity index are a concern. Further investigations on the mechanisms underlying changes in the peritoneal transport over time are needed.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
REFERENCES
- Twardowski ZJ, Nolph KD, Khanna R, Prowant BF, Ryan LP, Moore HL. Peritoneal equilibration test. Perit Dial Bull. 1987;7:138–147.
- Churchill DN, Thorpe KE, Nolph KD, Keshaviah PR, Oreopoulos DG, Page D. Increased peritoneal membrane transport is associated with decreased patient and technique survival for continuous peritoneal dialysis patients. The Canada-USA (CANUSA) Peritoneal Dialysis Study Group. J Am Soc Nephrol. 1998;9:1285–1292.
- Chung SH, Lindholm B, Lee HB. Is malnutrition an independent predictor of mortality in peritoneal dialysis patients? Nephrol Dial Transplant. 2003;18:2134–2140.
- Rumpsfeld M, McDonald SP, Johnson DW. Higher peritoneal transport status is associated with higher mortality and technique failure in the Australian and New Zealand peritoneal dialysis patient populations. J Am Soc Nephrol. 2006;17:271–278.
- Davies SJ, Bryan J, Phillips L, Russell GI. Longitudinal changes in peritoneal kinetics: The effects of peritoneal dialysis and peritonitis. Nephrol Dial Transplant. 1996;11:498–506.
- Margetts PJ, McMullin JP, Rabbat CG, Churchill DN. Peritoneal membrane transport and hypoalbuminemia: Cause or effect? Perit Dial Int. 2000;20:14–18.
- Chung SH, Heimburger O, Stenvinkel P, Wang T, Lindholm B. Influence of peritoneal transport rate, inflammation, and fluid removal on nutritional status and clinical outcome in prevalent peritoneal dialysis patients. Perit Dial Int. 2003;23:174–183.
- Passadakis PS, Thodis ED, Panagoutsos SA, Selisiou CA, Pitta EM, Vargemezis VA. Outcome for continuous ambulatory peritoneal dialysis patients is not predicted by peritoneal permeability characteristics. Adv Perit Dial. 2000;16:2–6.
- Brown EA, Davies SJ, Rutherford P, Survival of functionally anuric patients on automated peritoneal dialysis: The European APD Outcome Study. J Am Soc Nephrol. 2003;14:2948–2957.
- Reyes MJ, Bajo MA, Hevia C, Inherent high peritoneal transport and ultrafiltration deficiency: Their mid-term clinical relevance. Nephrol Dial Transplant. 2007;22:218–223.
- Lo WK, Brendolan A, Prowant BF, Changes in the peritoneal equilibration test in selected chronic peritoneal dialysis patients. J Am Soc Nephrol. 1994;4:1466–1474.
- Hung KY, Huang JW, Tsai TJ, Chen WY. Natural changes in peritoneal equilibration test results in continuous ambulatory peritoneal dialysis patients: A retrospective, seven year cohort survey. Artif Organs. 2000;24:261–264.
- Wong TY, Szeto CC, Lai KB, Lam CW, Lai KN, Li PK. Longitudinal study of peritoneal membrane function in continuous ambulatory peritoneal dialysis: Relationship with peritonitis and fibrosing factors. Perit Dial Int. 2000;20:679–685.
- Davies SJ. Longitudinal relationship between solute transport and ultrafiltration capacity in peritoneal dialysis patients. Kidney Int. 2004;66:2437–2445.
- Forbes GB, Bruining GJ. Urinary creatinine excretion and lean body mass. Am J Clin Nutr. 1976;29:1359–1366.
- Bergstrom J, Heimburger O, Lindholm B. Calculation of the protein equivalent of total nitrogen appearance from urea appearance. Which formulas should be used? Perit Dial Int. 1998;18:467–473.
- Chung SH, Chu WS, Lee HA, Peritoneal transport characteristics, comorbid diseases and survival in CAPD patients. Perit Dial Int. 2000;20:541–547.
- Ates K, Erturk S, Nergisoglu G, Sex-dependent variations in peritoneal membrane transport properties in CAPD patients. Nephrol Dial Transplant. 1996;11:2375–2376.
- Park HC, Kang SW, Choi KH, Ha SK, Han DS, Lee HY. Clinical outcome in continuous ambulatory peritoneal dialysis patients is not influenced by high peritoneal transport status. Perit Dial Int. 2001;21 Suppl. 3:S80–85.
- Yang X, Fang W, Bargman JM, Oreopoulos DG. High peritoneal permeability is not associated with higher mortality or technique failure in patients on automated peritoneal dialysis. Perit Dial Int. 2008;28:82–92.
- Raj DS, Langos V, Gangam N, Roscoe J. Ethnic variability in peritoneal equilibration test and urea kinetics. Am J Kidney Dis. 1997;30:374–381.
- Struijk DG, Krediet RT, Koomen GC, Boeschoten EW, Hoek FJ, Arisz L. A prospective study of peritoneal transport in CAPD patients. Kidney Int. 1994;45:1739–1744.
- Gamba G, Mejia JL, Saldivar S, Pena JC, Correa-Rotter R. Death risk in CAPD patients. The predictive value of the initial clinical and laboratory variables. Nephron. 1993;65:23–27.
- Avram MM, Fein PA, Bonomini L, Predictors of survival in continuous ambulatory peritoneal dialysis patients: A five-year prospective study. Perit Dial Int. 1996;16(Suppl. 1):S190–194.
- Avram MM, Mittman N, Bonomini L, Chattopadhyay J, Fein P. Markers for survival in dialysis: A seven-year prospective study. Am J Kidney Dis. 1995;26:209–219.
- Yeun JY, Kaysen GA. Acute phase proteins and peritoneal dialysate albumin loss are the main determinants of serum albumin in peritoneal dialysis patients. Am J Kidney Dis. 1997;30:923–927.
- Blake PG. What is the problem with high transporters? Perit Dial Int. 1997;17:317–320.