Abstract
Objectives: The aims of this study were to evaluate whether hidden chronic renal insufficiency (CRI) may be considered an independent cardiovascular risk factor in patients with hypertension and to calculate cardiovascular risk in this population. Methods: A total of 756 hypertensive patients of ages from 35 to 74 years (mean 57.0 years; 58.2% women) and without evidence of cardiovascular disease were studied and followed during 10 years. Their glomerular filtration rate (GFR) was estimated using the simplified MDRD (result of the Modification of Diet in Renal Disease study) and Cockcroft–Gault formulas. Hidden CRI was identified by a GFR <60 mL/min/1.73 m2 with normal serum creatinine concentration (<1.4 mg/dL men; <1.3 mg/dL women). Results: Of the patients with hidden CRI using the MDRD equation, 22% presented cardiovascular events (RR, 1.60; 95% confidence interval (CI), 1.06–2.43; p < 0.05). While the estimated coronary risk using the original Framingham function was similar in patients with and without hidden CRI (18.2%), using the REGICOR function it was higher in those with CRI (7.7 vs. 7.2%, p < 0.05). Logistic regression analysis showed that smoking, male sex, age, and diastolic blood pressure were predictors of cardiovascular events. The presence of hidden CRI was not a statistically significant predictor using either the MDRD (OR, 1.37; 95% CI, 0.72–2.61; p = 0.340) or the Cockcroft–Gault (OR, 1.05; 95% CI, 0.50–2.23; p = 0.893) formulas. Conclusions: The hypertensive population of 35–74 years in age with hidden CRI showed a higher incidence of cardiovascular events, but hidden CRI may not be considered an independent cardiovascular risk factor.
INTRODUCTION
Chronic kidney disease (CKD) has been considered an independent risk factor for cardiovascular disease.Citation1–4 Recently, therefore, the recommendation has been to include patients with CKD in the highest risk group for subsequent cardiovascular events.Citation5–8
Currently, five stages are recognized in CKD,Citation9,Citation10 and chronic renal insufficiency (CRI) has been defined as an estimated glomerular filtration rate (GFR) below 60 mL/min/1.73 m2 (patients with CKD at stages 3–5).Citation6 The term “hidden” CRI has been applied to patients with CRI but normal creatinine levels. Most CRI patients fall into this group. Identifying these patients is the main objective in the prevention of the morbidity and mortality associated with renal failure, because early treatment in hidden CRI contributes to slowing the progression of the disease and reducing the cardiovascular morbidity associated with severe renal failure.Citation11
Hypertensive patients with renal failure have an increased risk of cardiovascular mortality and/or an increased incidence of acute myocardial infarction.Citation1,Citation4,Citation12–15 Also, an independent inverse relationship has been found between GFR and coronary disease mortality in hypertensive subjects followed for more than 9 years.Citation16 These data suggest that hypertensive patients with kidney disease are suitable candidates for stricter control of their blood pressure and secondary measures of cardiovascular prevention.Citation6
Various descriptive studies in Spanish primary care centers have shown that renal failure is an independent cardiovascular risk factor in hypertensive patients.Citation17 Furthermore, the prevalence of cardiovascular disease is inversely proportional to the level of renal function.Citation18 It has also been observed that patients with hypertension have a higher cardiovascular risk in the original FraminghamCitation19 and Framingham-REGICORCitation20 tables. Moreover, a higher prevalence of diabetes and target organ damage was found in these subjects.Citation21 However, the cross-sectional design of these retrospective studies means that, while they may suggest the formulation of hypotheses, no definitive conclusions may be drawn from them. We consider that an important aspect of epidemiological investigation in this area is to determine whether the higher prevalence of hidden CRI in hypertensive patients is a consequence of their hypertension or an independent cardiovascular risk factor.
Given this context, the aims of the present observational cohort study were (1) to evaluate whether hidden CRI, as estimated using GFR formulas, is an independent cardiovascular risk factor, and is therefore associated with higher values of cardiovascular morbidity and mortality in these hypertensive patients aged 35–74 years, followed for 10 years; and (2) to calculate the cardiovascular risk in this population.
PATIENTS AND METHODS
We performed a post hoc analysis of an observational study of a group of hypertensive patients included in a larger cohort of 1011 individuals aged 35–74 years, without cardiovascular disease recorded in their medical history, followed during 10 years in a primary health-care center.Citation22 The subjects included in the study had systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg, or were taking antihypertensive drugs. The criterion for inclusion in the study cohort was that their medical history included the laboratory variables needed to estimate (1) the GFR by applying the Cockcroft–Gault formulaCitation23 corrected for body surface area (BSA),Citation24 and the simplified Modification of Diet in Renal Disease (MDRD) study formulaCitation25; and (2) coronary risk with the original FraminghamCitation19 and the Framingham function calibrated for the Spanish population (Framingham-REGICOR).Citation20 Additional data recorded included glycemia, body mass index (BMI), triglycerides, total cholesterol, low-density lipoprotein (LDL) cholesterol, and medication with hypolipidemic or antihypertensive drugs. Serum creatinine levels were measured by a single regional laboratory using a Jaffé reaction (Beckman ASTRA CX-3). CKD was staged according to The National Kidney Foundation criteria,Citation9,Citation10 and hidden CRI was defined as an estimated GFR below 60 mL/min/1.73 m2 (CKD stages 3–5) and serum creatinine levels <1.4 mg/dL in men and <1.3 mg/dL in women.Citation26 We excluded 37 hypertensive patients on overt CRI (24 men and 13 women with serum creatinine levels ≥1.4 mg/dL or ≥1.3 mg/dL, respectively). Finally, the resulting group consisted of 756 hypertensive patients. The cardiovascular events investigated were those included in the calculation of total coronary risk (angina and myocardial infarction, fatal and nonfatal) and fatal cardiovascular disease (cardiac death of coronary and noncoronary origin, death of cerebrovascular origin, and deaths from other cardiovascular causes). Acceptance as an event of cardiovascular origin required confirmation of the diagnosis by specialists in the field or by the pertinent tests in the referral hospital (stress test, thallium, coronary angiography, inter alia). Similarly, the acceptance of a cardiovascular cause for death required confirmation in the hospital archives, inquiry in the Civil Registry Office to review the death certificate, and contact by telephone with relatives for confirmation of the event.
Statistical analysis
The statistics used as representative of the sample for the univariate descriptive analysis were the mean and standard deviation for normal distributions, the median and quartile 1–3 range for non-normal distributions, and the observed frequencies and proportions for categorical variables. Normality of the variables was verified by the Kolmogorov–Smirnov test and normality diagrams, and homoscedasticity by the Levene test. In the bivariate analyses, a t-test for independent samples was used for normally distributed quantitative variables, a nonparametric Mann–Whitney U-test for non-normal variables, and a chi-squared test or Fisher's exact test for categorical variables. Multivariate analysis was performed using a binary logistic regression model, including all the clinically or statistically significant variables from the bivariate analyses. The minimum significance level was taken to be p < 0.05, and the odds ratio (OR) was used as a measure of risk, with a 95% confidence interval (CI). The Kaplan–Meier method was used for a survival study using the Breslow statistic to compare the curves, with a prior analysis of the risk ratios by means of a Cox proportional hazards model.
The data were processed and analyzed using the software packages SPSS for Windows in 12.0 (SPSS Inc., Chicago, Illinois, USA), the R environment 2.5.0 (free software, R Development Core Team), Epi Dat 3.1 (free software, Conselleria de Sanidade, Xunta de Galicia, Spain, and OPS-OMS), and Epi Info 6.04 (free software, CDC, Centers for Disease Control and Prevention).
RESULTS
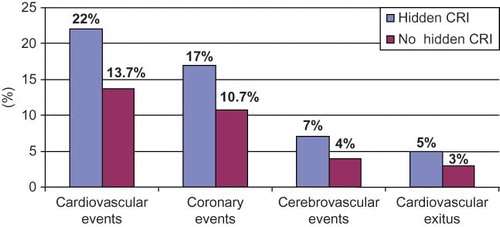
lists the relevant baseline characteristics of the study subjects. The mean age was 57.2 years, 58.2% were women, the mean BMI was 29.1 kg/m2, 24.5% of the patients had diabetes, and 21.3% were smokers. The mean coronary risk was moderate using either the original Framingham (18.2%) or the calibrated REGICOR (7.3%) functions. Women were older, had higher SBP and BMI, and were under antihypertensive treatment in higher proportion than men. The proportion of subjects with hidden CRI according to the criteria established (all of them with CKD stage 3) was 13.2% using the MDRD or 9.8% using the Cockcroft–Gault formulas. Patients with the hidden CRI criteria using the MDRD formula were more commonly women (88%), obese (BMI 30.1 kg/m2), older (65.2 vs. 55.8 years, p < 0.001), and showed higher SBP and proportions of diabetes and prescription antihypertensive therapy as compared to patients without hidden CRI (). During the period of the study, 22.0% of hypertensive patients with hidden CRI according to the MDRD formula had some cardiovascular event versus 13.7% of patients without hidden CRI ( and ) (relative risk (RR) of 1.60; 95% CI, 1.06–2.43). The rates of coronary events were 17.0 versus 10.7%, respectively (RR, 1.59; 95% CI, 0.98–2.59). The Framingham-REGICOR function underestimated the real coronary risk of these patients (7.7 vs. 17.0%, p < 0.05), while the original Framingham function gave an estimate that was similar to the real risk of this population (18.2 vs. 17.0%, p = 0.852).
TABLE 1. General characteristics of the patients in the study
TABLE 2. General characteristics, cardiovascular events, and coronary risk in the patients with and without hidden chronic renal insufficiency criteria as estimated by the MDRD equation
FIGURE 1. Percentage of cardiovascular events in the cohort during the 10-year follow-up, with glomerular filtration rate calculated using the MDRD equation. MDRD, abbreviated formula from the Modification of Diet in Renal Disease study; CRI, chronic renal insufficiency.
Patients who developed some cardiovascular event during the follow-up period () were older (61.2 vs. 56.3 years, p < 0.001), predominantly male (55.4 vs. 39.4%, p < 0.01), with higher values of SBP, DBP, glycemia, and serum creatinine, higher percentages of diabetes, smoking, and under medication with antihypertensive drugs, and a higher proportion of hidden CRI by the MDRD formula (19.6 vs. 12.1%, p < 0.05). These cardiovascular event patients also had increased coronary risk according to both of the coronary risk functions tested: with the original Framingham function they would be considered as high risk (risk of 24.5%) and with the Framingham-REGICOR function they would be close to this category (risk of 9.8%).
TABLE 3. General characteristics of the patients with and without cardiovascular events
The dependent variable in the logistic regression multivariate analysis was the presence of cardiovascular events. In the final model that used the MDRD formula to determine hidden CRI (), the significant predictors of cardiovascular events in hypertensive patients were age, sex (male), DBP, diabetes, and smoking. The OR for smoking was 2.71 (95% CI, 1.50–4.88; p < 0.001). The presence of hidden CRI did not reach statistical significance as a predictor (OR, 1.37; 95% CI, 0.72–2.61; p = 0.340). Neither was this factor statistically significant (OR, 1.05; 95% CI, 0.50–2.23; p = 0.893) in the model that used the Cockcroft–Gault formula (), in which the same variables as in the previous case again were distinguished as cardiovascular risk factors. In a separate analysis by gender, CRI was not an independent significant risk factor for cardiovascular disease in men or women.
TABLE 4. Predictors of cardiovascular events in the logistic regression multivariate analysis and estimation of renal function with the MDRD and Cockcroft-Gault formulas
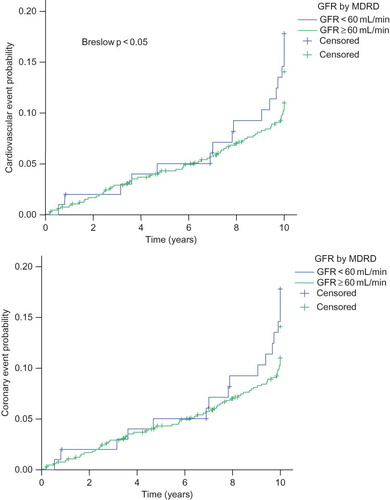
The Kaplan–Meier survival curves () showed patients with hidden CRI estimated with the MDRD formula to have a greater likelihood of cardiovascular events during follow-up (p < 0.05). The case was similar for the likelihood of coronary events, but the difference did not quite reach statistical significance (p = 0.084).
FIGURE 2. Kaplan–Meier survival curves for cardiovascular and coronary events in patients with and without hidden renal insufficiency with glomerular filtration rate calculated using the MDRD equation. MDRD, abbreviated formula from the Modification of Diet in Renal Disease study; GFR, glomerular filtration rate.
DISCUSSION
Renal dysfunction has been associated with an increased risk of cardiovascular and total mortality in the general populationCitation4,Citation12,Citation27–32 and in hypertensive patients.Citation13,Citation14,Citation33 This association is detectable already at a mild-to-moderate stage, when the estimated GFR drops below 60 mL/min.Citation4,Citation13,Citation34 In Spain, the observed prevalence of kidney dysfunction in hypertensive patients has varied between studies depending on the population analyzed, from 9.8% in the CORONARIA studyCitation21 to 32.4% in the FRESHA study.Citation17 In the present case, we found a prevalence of 13.2% of hidden CRI, intermediate between the values reported in the aforementioned two studies. These differences in the prevalence of hidden CRI in hypertensive populations may be explained by the lower average age of our population and the profile of the patients chosen for inclusion, because in our case we only included hypertensive patients without a history of cardiovascular disease. In Spain, those two multicenter studiesCitation17,Citation21 analyzed the cardiovascular risk of hypertensive patients with renal dysfunction treated in primary care. Their patients had a greater target organ damage ratio and increased coronary risk using the original Framingham and the calibrated Framingham-REGICOR charts. This also was confirmed in this study. The original Framingham function overestimated coronary risk in our hypertensive population (18.2 vs. 11.5%, p < 0.001; ) but was in keeping with the real coronary risk in the subgroup with hidden CRI (18.2 vs. 17.0%, p = 0.852; ), indirectly confirming the well-known better performance of this function in higher cardiovascular risk populations. The Framingham-REGICOR function underestimated coronary risk in both the total population (7.3 vs. 11.5%, p < 0.01) and the subgroup with hidden CRI (7.7 vs. 17.0%, p < 0.05). These findings are further evidence of the need for an adjustment, calibration, and validation of the risk function on large populations representative of each country's reality such as that recently reported for the United Kingdom.Citation35
The high cardiovascular risk of hypertensive patients with renal dysfunction could be explained by a higher prevalence of the different risk factors in this subgroup of patients (age, percentage of smokers, SBP). In this sense, the greater morbidity and mortality of hypertensive patients with kidney disease could be a consequence of the impact of hypertension on the entire vascular system – heart, kidney, and other vascular territories. If, on the contrary, the CRI in hypertensive patients were an independent marker of cardiovascular risk, it would only be discernable in observational studies with enough follow-up time for cardiovascular events to emerge. One such studyCitation16 analyzed 9929 hypertensive patients followed for an average of 9.6 years and found an inverse relationship between GFR and ischemic heart disease mortality in hypertensive patients. Our results indicate that hidden CRI diagnosed using the MDRD-estimated GFR was associated with an increased risk of cardiovascular events in the 10-year follow-up (RR, 1.60; 95% CI, 1.06–2.43; p < 0.05). However, adjusting for the different risk factors in the logistic regression analysis left only the variables smoking, diabetes, sex (male), age, and DBP as significant predictors of cardiovascular events in the final model, regardless of whether the hidden CRI was diagnosed by estimating the GFR with the MDRD or the Cockcroft–Gault formulas (). It may not be surprising that hidden CRI is not a risk factor after adjustment for age, because there is a decline in GFR with age. The data therefore did not confirm what had been found in the general population of the cohort,Citation36 that hidden CRI behaves as an independent cardiovascular risk factor. The same conclusion is reached when the value of GFR estimated by the MDRD or the Cockcroft–Gault formulas was introduced directly in the logistic regression multivariate analysis, rather than the dichotomy variable of GFR less than 60 mL/min or not. Even though the limited size of the sample of patients and of the number of cardiovascular events that occurred during the follow-up (only 112) might have reduced the statistical power of the study, the higher ORs of smoking, diabetes, and sex add biological plausibility to the results. Moreover, the serum creatinine assays were done in the same hospital laboratory for the entire cohort, so that the technique to quantify the creatinine has to be eliminated as a possible source of variability, increasing the internal validity of the study. Because the formulas to estimate the GFR are not accurate enough to measure GFR in patients with normal creatinine values and mild decreased renal function,Citation37 the measurement of GFR with endogenous or exogenous filtration markers is the most accurate strategy for the assessment of renal function in this population with normal serum creatinine levels. However, similar results obtained with the MDRD and the Cockcroft–Gault definition of hidden CRI is further evidence of consistency. Many studies have chosen to use the MDRD formula for its relative ease of implementation, as knowledge of the patient's weight is not required. The Cockcroft–Gault formula, on the other hand, requires the knowledge of height to adjust the GFR to 1.73 m2 of BSA and to facilitate comparison with MDRD. In our case, the two formulas led to similar final results, but, because of the lack of height data, 70 or fewer patients could be classified for the presence or absence of hidden CRI using the Cockcroft–Gault formula. The good correlation indices observed between the Cockcroft–Gault and MDRD formulas in hypertensive populationsCitation17,Citation38 lend support to the use of the latter, although it should be borne in mind that they are both inaccurate in situations of normal renal function or hyperfiltration, in which cases they introduce significant biases.Citation39
This study has clear limitations. The small size of the cohort and the small number of cardiovascular events may limit the statistical power of any associations found. The population was not randomly selected, but corresponded to patients who had been attended to at the center and had a clinical history available that included the information necessary for the Framingham coronary risk calculations and the Cockcroft–Gault and MDRD GFR formulas. Our results therefore correspond to hypertensive patients with an existing anamnesis at an urban health center and with no history of cardiovascular disease, and may not be extrapolatable to the general hypertensive population. The period when data collection started coincided with the first years of health-care reform in Spain and the setting up of primary care centers. Most of the patients assigned to these centers had no proper clinical history. It was only then that regular histories really began to be constructed progressively. The prevalence and mean values of the risk factors of our cohort have therefore to be seen in this context, although they were very similar to those described for Spain's overall hypertensive population. The number of the hidden CRI in males was small (only 12 out of 100 cases, ). In addition, female sex and normal or underweight were factors associated with high risk of misclassification of impaired kidney function in older adults with normal serum creatinine.Citation40 Furthermore, hidden CRI was diagnosed with a single GFR determination. We have no information on the temporal stability of these determinations, and hence nor on whether the renal dysfunction observed at the recruitment of the patients was a transient or chronic alteration. However, this is a commonly used methodological approach in studies that investigate aspects of CKD,Citation13,Citation16,Citation17,Citation21,Citation41,Citation42 so that our results should be comparable with them. Another potential limitation of the study is the possibility of inadequate identification and quantification of cardiovascular events during cohort follow-up. However, the method established to search for and confirm events of this nature made it difficult for them to be overlooked during the 10-year follow-up.Citation22 Finally, as the results are from a post hoc analysis of an observational study, the existence of other unidentified confounding factors cannot be completely excluded, and, as is general with studies of this type, the results can only be used to generate new hypotheses.
In summary, the study has provided evidence that hypertensive patients of 35–74 years in age, with hidden CRI and no history of cardiovascular disease, present an increased incidence of cardiovascular events during a follow-up period of 10 years. However, hidden CRI defined by a GFR <60 mL/min/1.73 m2 as estimated by both MDRD and Cockcroft–Gault formulas does not behave as an independent predictor of cardiovascular events in hypertensive patients with normal creatinine values.
Acknowledgments
This study was funded by redIAPP (Innovation and Integration of Prevention and Health Promotion in Primary Care), thematic coo perative research network G03/170, and by a grant from the Program for Promotion of Research in Primary Care, of the Instituto de Salud Carlos III. The second and third authors of the article also received a predoctoral scholarship from the Spanish Society of Family and Community Medicine.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Zanchetti A, Hansson L, Dalhöf B, Effects of individual risk factors on the incidence of cardiovascular events in the treated hypertensive patients of the Hypertension Optimal Treatment Study. J Hypertens. 2001;19:1149–1159.
- Santopinto JJ, Fox KAA, Goldberg RJ, Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: Findings from the global registry of acute coronary events (GRACE). Heart. 2003;89:1003–1008.
- Mann JF, Gerstein HC, Pogue J, Bosch J, Ysusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: The HOPE randomized trial. Ann Intern Med. 2001;134:629–636.
- Henry RM, Kostense PJ, Bos G, Mild renal insufficiency is associated with increased cardiovascular mortality: The Hoorn study. Kidney Int. 2002;62:1402–1407.
- Guidelines Committee. 2003 European Society of Hypertension – European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–1053.
- Chobanian AV, Bakris JL, Black HR, The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. The JNC 7 report. JAMA. 2003;289:2560–2572.
- Segura J, Campo C, Gil P, Development of chronic kidney disease and cardiovascular prognosis in essential hypertensive patients. J Am Soc Nephrol. 2004;15:1616–1622.
- Ruilope LM. Renal function and cardiovascular risk in hypertensive patients. J Hypertens. 2005;23:1787–1788.
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification and stratification. Am J Kidney Dis. 2002;39(Suppl 1):S1–S266.
- Levey AS, Coresh J, Balk E, National Kidney Foundation practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Ann Intern Med. 2003;139:137–147.
- Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med. 2004;164:659–663.
- Rahman M, Brown CD, Coresh J, The prevalence of reduced glomerular filtration rate in older hypertensive patients and its association with cardiovascular disease: A report from the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Arch Intern Med. 2004;164:969–976.
- Ruilope LM, Salvetti A, Jamerson K, Renal function and intensive lowering of blood pressure in hypertensive participants of the hypertension optimal treatment (HOT) study. J Am Soc Nephrol. 2001;12:218–225.
- De Leeuw PW, Thijs L, Birkenhager WH, Prognostic significance of renal function in elderly patients with isolated systolic hypertension: Results from the Sys-Eur trial. J Am Soc Nephrol. 2002;13:2213–2222.
- Rahman M, Pressel S, Davis BR, Cardiovascular outcomes in high-risk hypertensive patients stratified by baseline glomerular filtration rate. Ann Intern Med. 2006;144:172–180.
- Hailpern SM, Cohen HW, Alderman MH. Renal dysfunction and ischemic heart disease mortality in a hypertensive population. J Hypertens. 2005;23:1809–1816.
- Herrero P, Marín R, Fernández Vega F, Renal function and cardiovascular risk in patients with essential hypertension. The “FRESHA” study. Nefrología. 2006;26:330–338.
- Redón J, Cea-Calvo L, Lozano JV, Kidney function and cardiovascular disease in the hypertensive population: The ERIC-HTA study. J Hypertens. 2006;24:663–669.
- Wilson PWF, D´Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847.
- Marrugat J, Solanas P, D´Agostino R, Coronary risk estimation in Spain using a calibrated Framingham function. Rev Esp Cardiol. 2003;56:253–261.
- Cosín-Aguilar J, Hernándiz-Martínez A, Arístegui-Urrestarazu R, Coronary disease risk and prevalence of heart disease in primary care patients with hypertension and renal disease. Rev Esp Cardiol. 2006;59:1026–1032.
- Cañón L, Díaz N, Cruces E, Nieto T, Garrote T, Buitrago F. Predictive capacity, comparison and clinical consequences of Framingham-WILSON and REGICOR equations in patients taken care in a Badajoz primary health centre. Rev Esp Salud Pública. 2007;81:353–364.
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41.
- Dubois D, Dubois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med. 1916;17:863–871.
- Vervoort G, Willems HL, Wetzels JFM. Assessment of glomerular filtration rate in healthy subjects and normoalbuminuric diabetic patients: Validity of a new (MDRD) prediction equation. Nephrol Dial Transplant. 2002;17:1909–1913.
- Marín R, Fernández-Vega F, Gorostidi M, Blood pressure control in patients with chronic renal insufficiency in Spain: A cross-sectional study. J Hypertens. 2006;24:395–402.
- Garg AX, Clark WF, Haynes RB, House AA. Moderate renal insufficiency and the risk of cardiovascular mortality: Results from the NHANES I. Kidney Int. 2002;61:1486–1494.
- Muntner P, He J, Hamm L, Loria C, Welthon PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol. 2002;13:745–753.
- Manjunath G, Tighiouart H, Ibrahim H, Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003;41:47–55.
- Fried LF, Shlipak MG, Crump C, Renal insufficiency as a predictor of cardiovascular outcomes and mortality in elderly individuals. J Am Coll Cardiol. 2003;41:1364–1372.
- Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events and hospitalization. N Engl J Med. 2004;351:1296–1305.
- Anavekar NS, McMurray JJV, Velázquez EJ, Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295.
- Schillaci G, Reboldi G, Verdecchia P. High-normal serum creatinine concentration is a predictor of cardiovascular risk in essential hypertension. Arch Intern Med. 2001;161:886–891.
- Abramson JL, Jurkovitz CT, Vaccarino V, Weintraub WS, McClellan W. Chronic kidney disease, anemia, and incident stroke in a middle-aged, community-based population: The ARIC Study. Kidney Int. 2003;64:610–615.
- Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: Prospective open cohort study. BMJ. 2007;335:136–148.
- Calvo JI, Cañón L, Gómez-Jiménez C, Martín MV, Espigares M, Buitrago F. Cardiovascular risk in patients with renal failure. Med Clin (Barc). 2008;131:41–46.
- Bostom AG, Kronenberg F, Ritz E. Predictive performance of renal function equations for patients with chronic kidney disease and normal serum creatinine levels. J Am Soc Nephrol. 2002;13:2140–2144.
- Ruilope LM, Zanchetti A, Julius S, Prediction of cardiovascular outcome by estimated glomerular filtration and estimated creatinine clearance in the high-risk hypertension population of the VALUE trial. J Hypertens. 2007;25:1473–1479.
- Fontseré N. Kidney and cardiovascular disease: Are the predictive equations of glomerular filtration useful? Med Clin (Barc). 2007;129:697–698.
- Giannelli SV, Patel KV, Windham BG, Pizzarelli F, Ferrucci L, Guralnik JM. Magnitude of underascertainment of impaired kidney function in older adults with normal serum creatinine. J Am Geriatr Soc. 2007;55:816–823.
- De Francisco ALM, De la Cruz JJ, Cases A, Prevalence of kidney insufficiency in primary care population in Spain: EROCAP study. Nefrología. 2007;27:300–312.
- Cea-Calvo L, Redón J, Martí-Canales JC, Prevalence of low glomerular filtration rate in the elderly population of Spain. The PREV-ICTUS study. Med Clin (Barc). 2007;129:681–687.
