Abstract
Culture-negative peritonitis, which results from a variety of etiologies, such as problems in culture techniques, prior use of antibiotics, infection caused by unusual organisms, and noninfectious causes, accounts for up to 20% of cases of peritonitis in peritoneal dialysis patients and sometimes poses diagnostic and therapeutic dilemmas. A 62-year-old woman on continuous ambulatory peritoneal dialysis (CAPD) presented with minimal abdominal pain and a turbid dialysate. Under the impression of infectious peritonitis, empirical intraperitoneal (IP) antibiotic treatment was administered. All cultures from the effluent were negative, although the white blood cell count in the effluent was elevated. Despite initial clinical improvement and resolution of abdominal pain, mild fever persisted, even after removal of the CAPD catheter. The first CT scan before removal of the catheter demonstrated no evidence of intra-abdominal pathology, except for the possibility of peritonitis, but a follow-up CT scan after removal of the catheter demonstrated a perforated appendix with a peri-appendiceal abscess. The patient recovered completely after removal of the appendix and the abscess. This case suggests that a follow-up CT scan and/or surgical exploration should be considered to identify the intra-abdominal pathology in patients with culture-negative refractory peritonitis, even after removal of CAPD catheter.
INTRODUCTION
Peritonitis is the most frequent complication of continuous ambulatory peritoneal dialysis (CAPD). Most cases of peritonitis are associated with the indwelling peritoneal catheter and are caused by a single organism (especially Gram-positive organisms), and are usually treated with IP antibiotics.Citation1 However, in some cases, dialysis effluent cultures may be negative for a variety of technical and clinical reasons. Culture-negative peritonitis accounts for up to 20% of the cases of CAPD-related peritonitis.Citation2,Citation3 The etiologies include problems in culture techniques, prior use of antibiotics, infection caused by unusual organisms, and non-infectious causes (especially drug reactions, malignancies, and abdominal and retroperitoneal inflammation).Citation1,Citation4–8
Most commonly, culture-negative peritonitis results from problems in culture techniques and readily resolves with standard IP antibiotic treatment.Citation2,Citation4 However, the clinical outcome of culture-negative peritonitis may not be satisfactory, and sometimes a life-threatening condition occurs. Therefore, culture-negative peritonitis poses a significant diagnostic and therapeutic dilemma.Citation3,Citation9,Citation10 We report a case that was initially treated as a CAPD-related peritonitis with a turbid dialysate and minimal symptoms, but was finally diagnosed as appendicitis with perforation.
CASE REPORT
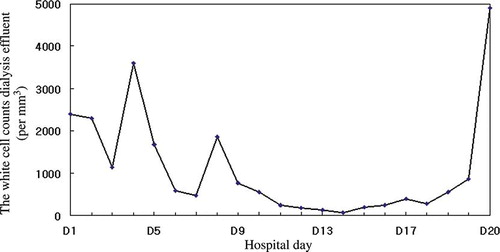
A 62-year-old woman presented with mild abdominal pain and a turbid dialysate of 24 h duration. She had undergone CAPD for 5 years because of end-stage renal disease secondary to diabetes mellitus. She had no previous history of peritonitis and antibiotic use. She was not in a poor general health condition. Her temperature was 37.8°C with no distinctive change in recent weight, blood pressure was 153/64 mmHg, and pulse rate was 90 beats/min. On physical examination, the heart and lungs were found to be functioning normally. The abdomen was soft but showed diffuse mild tenderness on palpation. The bowel sounds were normal. The white blood cell count in the dialysate was 2400/mm3, with 92% polymorphonuclear leukocytes. The white blood cell count was 12,480/mm3, the hemoglobin level was 8.2 g/dL, the hematocrit was 26.0%, and the thrombocyte count was 199,000/mm3. The Blood urea nitrogen level was 53.2 mg/dL, the serum creatinine level was 7.82 mg/dL, and the C-reactive protein (CRP) level was 4.03 mg/dL. Under the diagnostic impression of CAPD-related peritonitis, empirical IP cefazolin and ceftazidime were administered. The white blood cell count in the dialysis effluent declined to 840/mm3, and the mild abdominal discomfort subsided after 2 days of administration of IP antibiotics. Gram stain and culture of effluent and blood were negative. However, 4 days later, the cell count in the effluent increased to 3600/mm3. A CT scan of the abdomen showed ascites in the abdominopelvic cavity, with peritoneal thickening and enhancement in the pelvic cavity, suggesting the possibility of peritonitis (see A); however, the white blood cell count decreased to 590/mm3.
FIGURE 1. A CT scan of the abdomen in a patient on peritoneal dialysis who presented with peritonitis. (A) The first CT scan showed ascites in the abdominopelvic cavity, with some particular peritoneal thickening with enhancement in the pelvic cavity, suggesting possibility of peritonitis. (B) The second CT scan showed increased ascites, peritoneal thickening with enhancement, and thickening of the diffuse bowel loop, suggesting peritonitis and reactive bowel wall thickening, and dilatation and increased enhancement of appendiceal loop (arrow). (C, D) The third CT scan demonstrated perforated appendicitis with peri-appendiceal abscess (arrow).
Thereafter, the white blood cell counts in the effluent remained between 100 and 300/mm3 (see ), and she did not have any symptoms. Because she strongly refused the removal of the CAPD catheter, we maintained IP antibiotic treatment. On the twentieth day of IP antibiotic treatment, the white blood cell count rose again to 4900/mm3. Considering culture-negative refractory peritonitis, we removed the CAPD catheter and substituted intravenous (IV) imipenem, vancomycin, and oral rifampin for IP cefazolin and ceftazidime. She received hemodialysis thereafter. Another abdominal CT scan was performed 6 days after removal of the catheter because of a mild fever (36.5°C–37.8°C) and increased CRP. The CT scan revealed increased ascites, peritoneal thickening with enhancement, and thickening of diffuse bowel loops, suggesting peritonitis and reactive bowel wall thickening, and dilatation and increased enhancement of the appendiceal loop (see B). Percutaneous catheter drainage (PCD) was inserted in the pelvic cavity. Despite removal of the catheter and antibiotic treatment, a mild fever and an increase in the white cell count in the ascites developed intermittently. A follow-up CT scan 15 days after catheter removal demonstrated perforated appendicitis with a peri-appendiceal abscess (see C and D). An appendectomy was performed. Enterobacter cloacae were isolated in the culture obtained from the abscess. After surgery her symptoms and laboratory findings completely resolved.
DISCUSSION
We presented a case in which culture-negative refractory CAPD peritonitis with minimal symptoms was finally diagnosed as a suppurative appendicitis.
Although the most common cause of peritonitis in patients on CAPD is infectious peritonitis, 15–20% of the cases are culture-negative peritonitis.Citation1–3 Patients with culture-negative peritonitis have repeatedly sterile effluent cultures, despite turbid dialysates, and elevated white blood cell counts in the effluent. Of the variable etiologies associated with culture-negative peritonitis, peritonitis secondary to intra-abdominal pathology, such as inflammation, perforation, or ischemia of intra-abdominal organs, accounts for approximately 10% of the cases of peritonitis.Citation10,Citation11 Intra-abdominal inflammation, such as cholecystitis, small bowel incarceration, and appendicitis, may present with clinical manifestations indistinguishable from those of infectious peritonitis.Citation12,Citation13 Furthermore, there are cases in which the initial CT scan sometimes fails to demonstrate the underlying pathology,Citation13,Citation14 which can lead to increased morbidity and mortality due to the difficulty in diagnosis and often delayed surgical intervention, with a mortality rate of 50%.Citation10,Citation15,Citation16 Therefore, in patients with culture-negative peritonitis, a non-localizing physical examination and nonspecific results of a CT scan should not rule out intra-abdominal pathology. In this clinical scenario, the combined diagnostic and therapeutic use of surgical exploration may be needed to reduce morbidity and mortality.Citation11,Citation14
In our case, the first CT scan of the abdomen demonstrated no evidence of appendicitis with any typical symptoms. However, the second CT scan showed findings suspicious for appendicitis, and the third CT scan demonstrated a perforated appendix with a peri-appendiceal abscess. It is interesting that appendicitis in a patient on CAPD manifested as sterile peritonitis without symptoms from the onset. The reasons that our patient did not develop typical symptoms despite the progression of inflammation by appendicitis can be explained as follows: continuous antibiotic treatment may have led to partial treatment of inflammation and made the presentation and course of symptoms atypical. In addition, the continuous peritoneal lavage may have diluted the bacterial load and retarded abscess formation. Conversely, it is possible that appendicitis developed secondary to CAPD-related peritonitis in this case. However, considering the continued refractoriness to a standard antibiotic treatment protocol and clinical improvement after the appendectomy, it is more likely that the appendicitis was manifested as culture-negative peritonitis from the beginning.
In conclusion, in culture-negative peritonitis, intra-abdominal pathology may be initially masked under antibiotic therapy and revealed at a later date. Therefore, in patients with culture-negative refractory peritonitis in whom signs and symptoms do not rapidly resolve with established antibiotic therapy, a follow-up CT scan should be performed, even after removal of the CAPD catheter, and surgical exploration should be considered to identify the intra-abdominal pathology.
Acknowledgments
This publication was supported by grant A070001 from the Korea National Enterprise for Clinical Trials (KONECT).
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
REFERENCES
- Piraino B, Bailie GR, Bernardini J, Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int. 2005;25:107–131.
- Bunke M, Brier ME, Golper TA. Culture-negative CAPD peritonitis: the Network 9 Study. Adv Perit Dial. 1994;10:174–178.
- Szeto CC, Wong TY, Chow KM, Leung CB, Li PK. The clinical course of culture-negative peritonitis complicating peritoneal dialysis. Am J Kidney Dis. 2003;42:567–574.
- de Freitas DG, Gokal R. Sterile peritonitis in the peritoneal dialysis patient. Perit Dial Int. 2005;25:146–151.
- Rocklin MA, Teitelbaum I. Noninfectious causes of cloudy peritoneal dialysate. Semin Dial. 2001;14:37–40.
- Hsu YH, Huang MC, Ting CC, Tu HY, Hsia CC. Pseudomyxoma peritonei as a cause of culture-negative peritonitis for a patient undergoing peritoneal dialysis. Am J Kidney Dis. 2006;47:905–907.
- Lang CL, Chiang CK, Hung KY, Wu KD. Tubo-ovarian abscess presenting as culture-negative peritonitis in a patient undergoing treatment with peritoneal dialysis. Am J Kidney Dis. 2008;51:711–712.
- Yang CC, Lin SH, Tzeng YH, Chen CA, Tsai SH. Splenic infarction: An unrecognized cause of culture-negative peritonitis in a continuous ambulatory peritoneal dialysis patient. Clin Nephrol. 2007;68:262–265.
- Johnson DW, Gray N, Snelling P. A peritoneal dialysis patient with fatal culture-negative peritonitis. Nephrology (Carlton). 2003;8:49–55.
- Shrestha BM, Brown P, Wilkie M. Surgical peritonitis in patients on peritoneal dialysis. Perit Dial Int. 2008;28:331–334.
- Harwell CM, Newman LN, Cacho CP, Mulligan DC, Schulak JA, Friedlander MA. Abdominal catastrophe: Visceral injury as a cause of peritonitis in patients treated by peritoneal dialysis. Perit Dial Int. 1997;17:586–594.
- Steiner RW, Halasz NA. Abdominal catastrophes and other unusual events in continuous ambulatory peritoneal dialysis patients. Am J Kidney Dis. 1990;15:1–7.
- Yang CY, Chuang CL, Shen SH, Chen TW, Yang WC, Chen JY. Appendicitis in a CAPD patient: A diagnostic challenge. Perit Dial Int. 2007;27:591–593.
- Carmeci C, Muldowney W, Mazbar SA, Bloom R. Emergency laparotomy in patients on continuous ambulatory peritoneal dialysis. Am Surg. 2001;67:615–618.
- Wellington JL, Rody K. Acute abdominal emergencies in patients on long-term ambulatory peritoneal dialysis. Can J Surg. 1993;36:522–524.
- Kern EO, Newman LN, Cacho CP, Schulak JA, Weiss MF. Abdominal catastrophe revisited: The risk and outcome of enteric peritoneal contamination. Perit Dial Int. 2002;22:323–334.