Abstract
Reversible posterior leukoencephalopathy syndrome (RPLS) is a neurological syndrome characterized by headache, seizures, and visual loss, often associated with an abrupt increase in blood pressure. It was first described by Hinchey and colleagues in 1996 when they described a case series. RPLS has been described in number of medical conditions, renal dysfunction being one of them. Prompt diagnosis and therapy with antihypertensives, anticonvulsants, removal of any offending medication, and treatment of associated disorder are essential because early treatment might prevent progression to irreversible brain damage. Here, we report a case of young man with focal segmental glomerulosclerosis (FSGS) and heavy proteinuria, who developed classical, clinical, and neurological features of RPLS with complete recovery.
INTRODUCTION
Reversible posterior leukoencephalopathy syndrome (RPLS) is a clinical radiological syndrome of heterogeneous etiologies that are grouped together because of similar neuroimaging findings. This phrase of RPLS was first used by Hinchey et al.Citation1 in 1996 when they described a clinical syndrome of insidious onset of headache, confusion or decreased level of consciousness, visual changes, and seizures associated with the characteristic neuroimaging findings of posterior cerebral white matter edema. Here we report a case of RPLS in a young patient who was referred to our institution with diagnosis of steroid-resistant nephrotic syndrome.
CASE REPORT
A 23-year-old man was referred to our institution with a diagnosis of steroid-resistant nephrotic syndrome. Further enquiry revealed that he had lower limb swelling for 6 months, which was associated with frothy urine, but no hematuria, joint pain, or skin rash was reported. The patient was treated with steroids and angiotensin-converting enzyme inhibitor (ACEI) during this period. Examination showed a young man having cushingoid features, abdominal striae, normal volume regular pulse, blood pressure of 150/100 mmHg, bilateral pitting lower limb edema extending up to the thighs, and normal jugular venous pressure (JVP). Systemic examination revealed lower limb weakness of 3/5 mainly in the proximal group of muscles, exaggerated deep tendon jerks, up-going planters, and ill-sustained ankle clonus with no sensory abnormality, intact sphincteric control, and absent papilledema. The rest of the systemic examination was unremarkable.
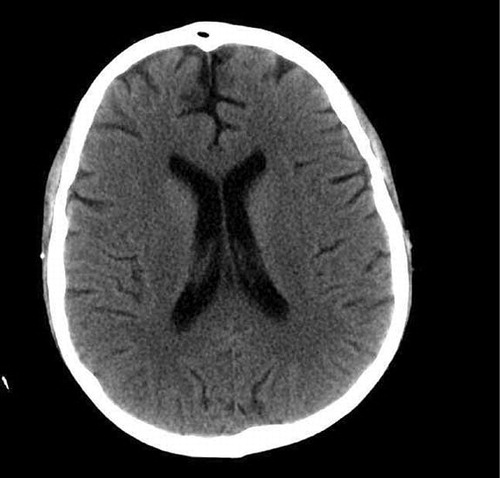
Initial labs revealed WBC (12,600), Hb (92 g/L), platelets (190,000), urea (33 mmol/L), creatinine (190 μmol/L), calcium (1.72 mmol/L), phosphorous (1.68 mmol/L), albumin (15 g/L), urine dip stick (UDS) blood 2+, protein 4+, 24-h urine protein (37.7 g/day), and normal chest x-ray. All the necessary serological markers were requested and the plan was to perform a renal biopsy. The next morning patient had a blood pressure of 160/110 mmHg and later complained of headache and visual blurring, which was followed by repeated episodes of generalized tonic–clonic seizures requiring endotracheal intubation; he was transferred to the intensive care unit. Subsequent neuroimaging, which initially included a plain CT scan of brain followed by an MRI (a–c), showed extensive multifocal area of edema along with a focus of hemorrhage in left temporal lobe highly suggestive of posterior reversible leukoencephalopathy syndrome (PRLS).
FIGURE 1. (a) A focus of hemorrhage in the left temporal area with associated edema. An MRI of the brain showing extensive multifocal parenchymal areas of edema, with hemorrhage (b) in the left temporal lobe and (c) in the inferior temporal gyrus region.
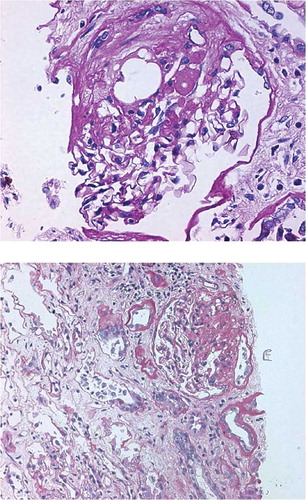
Blood pressure was controlled urgently by maximizing the doses of ACEI and short-acting calcium channel blockers. He was successfully extubated in the next few days with no more seizures and headache observed, and was shifted back to floor. A renal biopsy was performed later, which confirmed the diagnosis of focal segmental glomerulosclerosis (FSGS) (). CT scan of the brain () repeated after 2 weeks, which showed complete resolution of previous lesions, confirming the diagnosis of PRLS. Unfortunately, the patient showed gradual deterioration of his renal functions, requiring hemodialysis, and died 4 months later due to septicemia.
DISCUSSION
The finding of heavy proteinuria in this patient with hypertension, brisk deep tendon jerks, up-going planters, and weakness of lower limbs without any sensory disturbance raises the possibility of RPLS, although differential diagnosis is always quite broad in such a clinical scenario. Steroid-induced myopathy later confirmed by EMG further complicated the clinical picture in this patient. Renal biopsy confirmed FSGS and repeat CT scan () confirmed the diagnosis showing complete resolution of previous lesions.
RPLS is a clinical radiological syndrome of heterogeneous etiologies that are grouped together because of similar findings on neuroimaging studies. It was first accepted as single-named syndrome described in a 1996 case seriesCitation1 and it is often not confined to either the white matter or the posterior region of brain. The pathogenesis of RPLS remains unclear, but it appears to be related to disordered cerebral autoregulation and endothelial dysfunction.Citation1 A wide variety of medical conditions have been implicated as causes of RPLS.Citation2 Hypertensive disorders, renal disease, and immunosuppressive therapies remain the major risk factors for this disorder. Nephrotic state remains a risk factor and RPLS has been reported in a patient of FSGS previously.Citation3 There are no specific diagnostic criteria for RPLS. The clinical findings are not specific for RPLS and can resemble other neurological conditions like stroke, venous thrombosis, toxic or metabolic encephalopathy, demyelinating disorders, vasculitis, encephalitis, and bilateral posterior cerebral artery infarction. In an appropriate clinical setting, clinicians should recognize the neurological syndrome and order a neuroimaging study. Although considered to be a benign entity before, one of the largest case series reported highlights the potential grave consequences of this disorder.Citation4 Early recognition and lowering of blood pressure remain the optimum management strategy.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
REFERENCES
- Hinchey J, Chaves C, Appignani B, A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494.
- Lamy C, Openheim C, Meder JF, Mas JL. Neuroimaging in posterior reversible encephalopathy syndrome. J Neuroimaging. 2004;14(2):89–96.
- Tarek D, Burud S. Reversible posterior leukoencephalopathy syndrome: A review with two illustrated cases. Kuwait Med J. 2006;38(2):94–99.
- Covarrubias DJ, Luetmer PH, Campeau NG. Posterior reversible leukoencephalopathy syndrome: Prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol. 2002;23:1038.