Abstract
Human brucellosis is a systemic disease that involves multiple organs and tissues concomitantly. In this case, we describe a patient with pancarditis and nephrotic syndrome requiring hemodialyses, which is an unusually fatal condition resulting from brucellosis. He was successfully treated with early aortic valve replacement and intensive medical therapy.
INTRODUCTION
Human brucellosis is a zoonotic and systemic disease that involves multiple organs. The major contamination sources of Brucella are occupational contact of animals, animal products, and unpasteurized dairy products. Brucellosis is also an endemic disease that seems to be more prevalent in the Mediterranean basin, Middle East, Western Asia, Africa, and South America.Citation1 It presents as an acute (2 months) or subacute (2–12 months) febrile illness, which may progress to a chronic disease (>1 year) with severe complications.Citation2 It has various clinical manifestations including osteoarticular, genitourinary, gastrointestinal, nervous, cardiovascular, skin, and mucous membranes, and respiratory complications such as acute glomerulonephritis, epididymo-orchitis, sacroiliitis, panniculitis, arthritis, spondylitis, optic neuritis, acute cholecystitis, thrombocytopenic purpura, endocarditis, meningoencephalitis, depression, dementia, vascular stroke, and osteomyelitis.Citation3
To the best of our knowledge, there is no reported case on the concurrence of pancarditis and glomerulonephritis in brucellosis like this case.
CASE
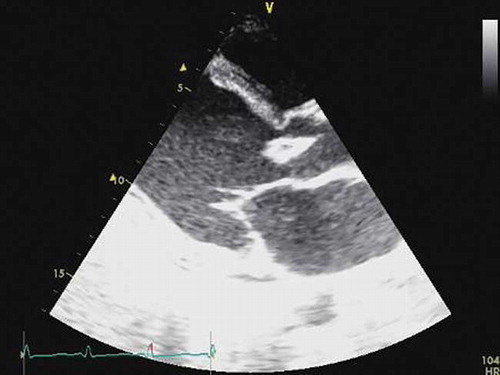
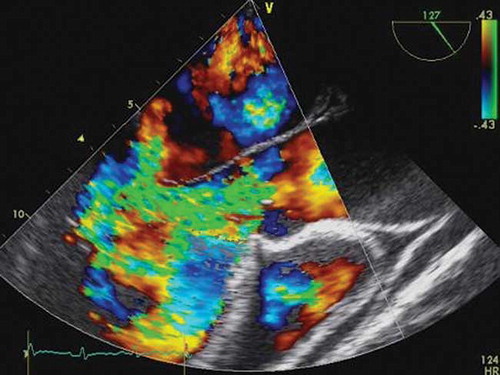
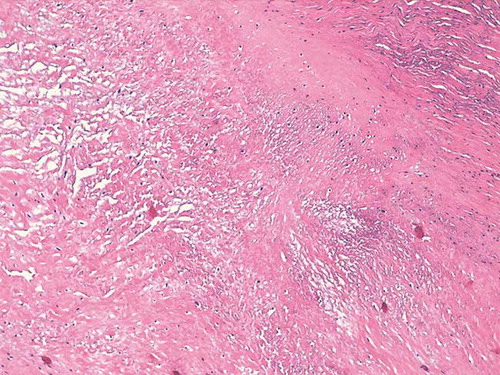
A 22-year-old man who worked in an animal husbandry presented to our clinic with a complaint of ankle and scrotal edema. He had been asymptomatic until 3 weeks before and had no history of using any drug. At admission he had no fever, and his creatinine was 1.7 mg/dL (0.7–1.3) and potassium 6.6 mmol/L (3.5–5.5). He had 5.8 g/day proteinuria upon urinalysis and the value of serum albumin was 2.6 g/dL. Laboratory analysis also yielded a hemoglobin level of 9.9 g/dL, an erythrocyte sedimentation rate of 82 mm/h, a C-reactive protein level of 62 mg/dL (0–4 mg/dL), a blood urea nitrogen level of 82 mg/dL (8–26), an alanine aminotransferase level of 21 U/L (0–40), and an aspartate aminotransferase level of 44 U/L (0–55) at admission. ANCA, ANA, anti-dsDNA antibodies, and Direct Coombs were all negative. Also, levels of serum direct and indirect bilirubin and reticulocyte were normal. Level of serum haptoglobulin was normal. Urinalysis showed many red blood cells and granular casts on examination of urine hematuria. Renal ultrasonography showed normal-sized kidneys with normal parenchymal echogenicity. Complement C3C was 19.6 mg/dL (79–152) and complement C4 was 14.8 mg/dL (16–38). Because of a fever of 38.5°C, white blood cells 12,000/µL with neutrophil predominance, and many leucocyte cylinder in the urine sediment, intravenous imipenem was given to the patient with a prediagnosis of urinary infection on the second day after admission. For persistent hyperpotassemia, hypervolemia, and worsening renal function he underwent hemodialysis and ultrafiltration four times a week. Renal biopsy showed both cortical and medullary tissue, with up to three glomeruli present in each representative tissue section. The biopsy revealed proliferative glomerulonephritis () with widening of the lobules, increase in cellularity, neutrophilic infiltration, and obliteration of capillary lumens of the glomerulus. Direct immunofluorescence staining showed C3 deposition in the glomeruli and no staining for IgG, IgM, IgA, and fibrinogen. We detected poststreptococcal glomerulonephritis, but he had a low antistreptolysin anticore and brucella was demonstrated upon drawing three blood culture. Brucella Wright agglutination test was found positive at 1/320 titration in the serum and he also had 176 IU/mL (0–20) value of rheumatoid factor. Intravenous rifampicin and peroral doxycycline were started after positive blood culture. To determine why the patient had pericardial frotman on physical examination and persistent high fever every passing third day after antibiotherapy, electrocardiography and echocardiography were applied. He had negative T waves in the precordial derivations on electrocardiogram with increased cardiac enzymes and troponin T. Echocardiography demonstrated a large vegetation in the ventricular surface of the aortic valve related with both non-coronary and right coronary cusps with a severe aortic regurgitation (). He also had increased left ventricular diameters with 49% ejection fraction, global left ventricular hypokinesia, moderate mitral regurgitation, mild tricuspid regurgitation, and minimal pericardial effusion around the heart. Intravenous ceftriaxone was quickly added to the antibiotic therapy. Transesophageal echocardiogram revealed vegetation in the aortic valve () and severe aortic regurgitation (). Three days after adequate medical therapy, proteinuria and fever resolved and renal functions were also recovered. The patient underwent early surgery and aortic valve replacement was applied. Endocarditis was histologically confirmed after the surgery ().
Figure 1. Renal biopsy of the patient revealed mesangial cellularity with mesangial cells and neutrophils, endocapillary proliferation, and obliterated capillary loops.
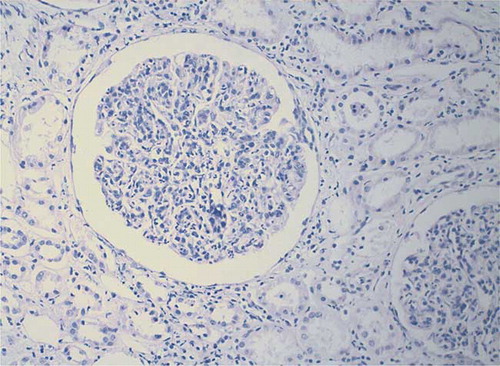
Figure 3. The vegetation was related with both non-coronary and right coronary cusps of the aortic valve in the transesophageal echocardiogram.

DISCUSSION
Cardiovascular involvement is very uncommon in brucellosis. Endocarditis is the most frequent type of cardiovascular involvement.Citation4 The first step in the diagnosis of endocarditis is to suspect the presence of endocarditis. An echocardiogram must be performed quickly after the suspicion of Brucella endocarditis, because endocarditis was found to be the major cause of death in brucellosis.Citation5 Isolated pericardial or myocardial involvement in brucellosis is non-ordinary.Citation6–11 Pericarditis may be almost asymptomatic but cardiac tamponade might also be seen after Brucella pericarditis.Citation6,Citation11,Citation12 Brucella myocarditis is also seen rarely, but it is very important that it is diagnosed because it may progress to heart failure.Citation10,Citation13 In our case, pericard, myocard, and endocard were involved in brucella but surgery was applied along with medical therapy before any other serious complications such as septic emboli, heart failure, or tamponade developed.
Brucellosis can also involve the genitourinary tract and can cause various types of renal diseases such as acute interstitial nephritis,Citation14 chronic granulomatous interstitial nephritis such as renal tuberculosis,Citation15 renal abscess,Citation16 mixed cryoglobulinemia,Citation17 and acute glomerulonephritis with or without endocarditis. In our patient we first detected acute renal failure because of acute glomerulonephritis and then brucella was detected in the blood cultures. Nephrotic syndrome and renal insufficiency at the onset of the brucella disease are also the major clinical predictors of poor prognosis with cardiac involvement.Citation18 Upon observing persistent high fever in the patient, we suspected endocarditis complicated by nephrotic syndrome, and the vegetation was demonstrated using transthoracic echocardiography. Our purpose was to emphasize that echocardiography should be performed in all patients with Brucella nephritis with or without high fever. In the diagnosis of brucellosis, concomitance of endocarditis and glomerulonephritis has occurred rarely.
This is the first case report demonstrating the involvement of endocard, myocard, and pericard in a patient with Brucella glomerulonephritis. In this case study of a 22-year-old man working in an animal husbandry diagnosed with brucellosis, a high mortality condition was seen because of endocarditis with myopericarditis complication, severe valve regurgitation resulting in cardiac involvement, and postinfectious glomerulonephritis that required hemodialysis.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Maurin M. Brucellosis at the dawn of the 21st century. Med Mal Infect. 2005;35:6–16.
- Mantur BG, Amarnath SK, Shinde RS. Review of clinical and laboratory features of human brucellosis. Indian J Med Microbiol. 2007;25:188–202.
- Gür A, Geyik MF, Dikici B, Complications of brucellosis in different age groups: A study of 283 cases in southeastern Anatolia of Turkey. Yonsei Med J. 2003;44:33–44.
- Reguera JM, Alarcón A, Miralles F, Pachón J, Juárez C, Colmenero JD. Brucella endocarditis: Clinical, diagnostic, and therapeutic approach. Eur J Clin Microbiol Infect Dis. 2003;22:647–650.
- Ferreira P, Gama P, Correia J, Brucella endocarditis – case report and literature review. Rev Port Cardiol. 2008;27:1309–1315.
- Anguita M, Díaz V, Bueno G, Pericarditis brucelósica: Dos formas diferentes de presentación para una etiología poco frecuente. Rev Esp Cardiol. 1991;44:482–484.
- Chocarro Matínez A, González López A, Zuazola P, García García I. Pericarditis brucelar. An Med Interna. 2002;19:50–51.
- Marcos Sánchez F, Vázquez García A, Juárez de Ucelay F, López Anega P, Durán Pérez-Navarro A. Afección pericárdica y miocárdica como forma de presentación de brucellosis. An Med Interna. 1991;8:100–101.
- García de Lucas MD, Castillo Domínguez JC, Martínez González MS. Brucella myopericarditis. Rev Esp Cardiol. 2004;57:709.
- Efe C, Can T, Ince M, Tunca H, Yildiz F, Sennaroglu E. A rare complication of Brucella infection: Myocarditis and heart failure. Intern Med. 2009;48:1773–1774.
- Ugartemendia MC, Curós-Abadal A, Pujol-Rakosnic M, Pujadas-Capenany R, Escrivá-Montserrat E, Jané-Pesquer J. Brucella mellitensis pericarditis. Am Heart J. 1985;109:1108.
- Karagiannis S, Mavrogiannaki A, Chrissos D, Papatheodoridis G. Cardiac Tamponade in Brucella Infection. Hellenic J Cardiol. 2003;44:222–225.
- Villaverde M, Gurini L, González A, Cohen R. Febryle syndrome: Miocarditis and brucellosis. Medicina. 1995;55:145–146.
- Dunea G, Kark RM, Lannigan R, D'Alessio D, Muehrcke RC. Brucella nephritis. Ann Intern Med. 1969;70:783–790.
- Petereit MF. Chronic renal brucellosis: A simulator of tuberculosis. Case report. Radiology. 1970;96:85–86.
- Onaran M, Sen I, Polat F, Irkilata L, Tunc L, Biri H. Renal brucelloma: A rare infection of the kidney. Int J Urol. 2005;12:1058–1060.
- Hermida Lazcano I, Saez Mendez L, Solera Santos J. Mixed cryoglobulinemia with renal failure, cutaneous vasculitis and peritonitis due to Brucella melitensis. J Infect. 2005;51:257–259.
- Bakri FG, Wahbeh A, Mahafzah A, Tarawneh M. Brucella glomerulonephritis resulting in end-stage renal disease: A case report and a brief review of the literature. Int Urol Nephrol. 2008;40:529–533.