Abstract
Ask-Upmark kidney is a rare diagnosis of segmental hypoplasia in pediatric population clinically characterized by severe hypertension potentially treatable with partial to total nephrectomy. Although originally was described only as a congenital anomaly, recent data suggest to be caused by vesicoureteral reflux, either in utero or in early childhood and pyelonephritis. The case we reported indicates that Ask-Upmark kidney should be considered as potential cause of hypertension and renal failure both in children and adults. The renal biopsy is necessary for early diagnosis and may consent to normalize blood pressure with nephrectomy; however, if renal damage is severe and progressive with tubulointerstitial nephritis, surgical management is excluded and renal transplant should be considered.
BACKGROUND
Segmental hypoplasia, known as the Ask-Upmark kidney is a scarred segment of the kidney characterized by thyroidization of tubules, intimal thickening of arteries, and arteriolar intimal hyalinization; dysplastic elements are absent, especially glomeruli.
Although originally it was described only as a congenital anomaly, recent data suggest that Ask-Upmark kidney may be caused by vesicoureteral reflux (VUR), either in utero or in early childhood and pyelonephritis. Severe hypertension is observed in over half of the patients and partial or total nephrectomy can be performed for treatment of hypertension.
The case we reported indicates that Ask-Upmark kidney should be considered as potential cause of hypertension and renal failure (RF) also in adults. Early diagnosis may consent to normalize blood pressure (BP) by nephrectomy; however, in presence of severe and progressive RF and tubulointerstitial nephritis (TIN), as in our patient, surgical management is excluded and renal transplant should be considered.
CASE REPORT
A 27-year-old woman was admitted to our department because of severe headache, nausea, and vomiting. Her BP was 180/120 mmHg and laboratory testing revealed RF (creatinine 2.7 mg/dL, BUN 30 mg/dL, ClCr 23 mL/min), uric acid 7.5 mg/dL, and anemia (Hb 10 g/dL). Serum potassium, sodium, calcium, erythrocyte sedimentation rate, and C reactive protein were within normal limits.
Emogasanalysis revealed mild metabolic acidosis. Urinalysis showed microscopic hematuria and proteinuria was 510 mg-24/h. In the past months, she reported headache in concomitance of elevated BP. She denied previous diagnosis of RF, recent infectious diseases, allergy symptoms, and recent use of drugs. Her family history was positive for hypertension. Autoimmunity testing was negative and serum complement was in the normal range. Ocular fundi revealed arteriolar narrowing, arteriovenous crossings, but no hemorrhages or exudates. Echocardiogram excluded signs of hypertension. Renal ultrasound (left kidney 97.5 mm, right 110.4 mm) showed in the lower pole of left kidney a circular iso-hyperechoic lesion (diameter 36.4 mm) sharply demarcated by the remaining parenchyma; left kidney had a cortical groove (). Kidney duplex ultrasonography excluded renal artery stenosis and the patient started therapy with irbesartan (150 mg/day) and nifedipine (60 mg/day). Renal perfusion and glomerular filtration rate (GFR) scintigraphy using technetium-99 m-diethylenetriaminepentaacetic acid showed a reduced global GFR of 37.65 mL/min (left kidney 17.83 mL/min, right kidney 19.82 mL/min).
Figure 1. Renal ultrasound showed left kidney pole with a circular iso-hyperechoic lesion sharply demarcated by the remaining parenchyma.
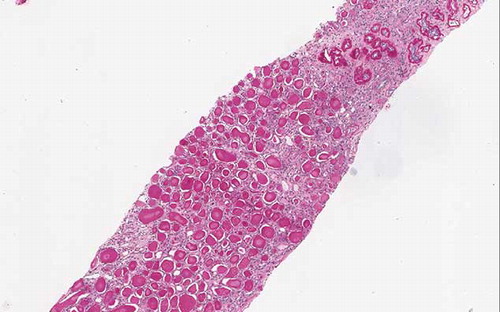
Because creatinine levels worsened until 4.3 mg/dL and BP was uncontrolled, percutaneous renal biopsy was performed to evaluate the etiology of RF. Renal tissue consisted of three biopsy cores, the first of them corresponding to the iso-hyperechoic lesion. Direct immunofluorescence performed on frozen sections was negative for IgA, IgG, IgM, C3, C1q, fibrinogen, k, and λ light chains. Light microscopy examination of the first core revealed renal cortex was made up of tubules often atrophic, dilated and separated by interstitial severe chronic inflammation made of lymphocytes and plasma cells; no glomeruli were found in this area ().
The remaining cores were both cortical and medullary renal tissue containing approximately 12 glomeruli all of them with advanced sclerosis; they appeared crowded together as a result of loss of the intervening renal tissue. Tubules were entirely atrophic, dilated, and filled with hyaline casts (so-called thyroidization) separated by fibrous tissue and chronic interstitial inflammation with mild arteriolar hyalinosis. These findings were not specific. The absence of glomeruli on the first core suggested that we dealt with an Ask-Upmark kidney.
The sclerotic crowded glomeruli and the extensive tubular atrophy were consistent with an advanced stage of TIN; this impression was supported also by the presence of plasma cells in the interstitial infiltrate.
In relation to histological findings, cystography denied VUR or other abnormalities, and a hormonal study revealed only mild increase of ranine plasma activity (26.1 pg/mL, normal range until 20.2 pg/mL).
We added in therapy doxazosin (2 mg/day) obtaining good BP control, even if RF worsened during 6 months follow-up (creatinine 5.6 mg /dL, urea 104 mg/dL). Because of rapid impairment of renal function the patient was a candidate for preemptive kidney transplant.
DISCUSSION
The rare abnormality known as Ask-Upmark kidney was described in 1929 by Eric Ask-Upmark and until a few years ago only 175 cases have been reported in literature with preponderance for women.Citation1,2 Pediatric population is more affected than adulthood, between the ages of 5 and 14 years.Citation3 Eric Ask-Upmark considered the lesion as a developmental abnormality.
One or both kidneys could be involved, characterized by outpunching of the renal pelvis into the renal parenchyma, reduced and retracted with grooving of the subcapsular surface. Microscopic scars are made up of tubules sometimes dilated and with thyroid-like appearance. There is intimal thickening of arteries and arteriolar intimal hyalinization; dysplastic elements, but especially glomeruli are absent. Sometimes it is possible to observe inflammatory cells.Citation4 In 1962, Batzenschlager et al. presented a classification of small kidneys introducing the term “aglomerular segmental hypoplasia,” which they considered to represent segmental absence of glomeruli.Citation5,6
The concept of segmental hypoplasia was developed in 1965 by Habib et al., reporting nine more cases of this rare condition, which they called “segmental hypoplasia of the kidney.” Thus, the terms Ask-Upmark kidney and segmental hypoplasia may be useful to identify the same lesions.Citation2
Royer et al.Citation7 in 1971 considered this lesion as an embryofetopathy resulting from an intrauterine insult to the growing kidney and most authors have continued to regard it as a congenital.
Recently, some authors reported in association with segmental hypoplasia, intrarenal and extra renal aneurysm, fibromuscular dysplasia, and renal artery stenosis. Segmental hypoplasia is frequently unilateral, but bilateral asymmetrical lesions have also been reported. Although originally was described only as a congenital anomaly, recent data suggest to be caused by VUR (in 70% of cases, either in utero or in early childhood) and pyelonephritis.Citation3 In reflux nephropathy, nephron loss might induce glomerular hypertension and hyperfiltration in the remnant glomeruli followed by glomerular hypertrophy, glomerulosclerosis, proteinuria, and RF. Important prognosis indicators of reflux nephropathy are size and decrease in the number of glomeruli in the specimens.Citation8 In our case, excluding the main causes of TIN (patient denied any drug consumption and autoimmunity profile was negative), we suppose that our patient had an advanced stage of TIN due to an early reflux in utero or in infancy, probably complicated by asymptomatic infection.
In fact, the renal abnormalities related to early reflux have a major clinical significance for long-term renal impairment and RF is rarely in infancy but can progress during the life.Citation9
Although our patient did not exhibit VUR in adulthood, the absence of reflux at the time of Ask-Upmark diagnosis cannot rule it out as initial cause of the atrophic kidney.Citation10 In fact, VUR is known to occur and disappear spontaneously prior to puberty.Citation5 Clinically, severe hypertension is observed in over half of the patients, other symptoms include proteinuria, recurrent urinary tract infections, and rarely, end-stage renal disease.Citation11 Regarding hypertension mechanism, increased renin levels have been reported,Citation12 suggesting renin-dependent hypertension as ischemic hypothesis. Some authors hypothesized that hypoplastic areas cannot release renin because of the absence of glomeruli and juxtaglomerular cells and secretion of renin may be produced by adjacent tissue.Citation3 Therefore, some patients have normal renin levels.Citation13 Nonetheless, partial or total nephrectomy can be performed as a curable cause of hypertension.Citation14 However, our patient presented renin levels slightly increased, progressive RF with GFR reduced in the right and left kidney and therefore was not considered for surgery. In literature, it is well known that nephrectomy is indicated in Ask-Upmark kidney as a treatment for hypertension, but the majority of patients reported in the studies not showed severe renal dysfunction probably due to its discovery during infancy. In fact, renal scarring in segmental hypoplasia is a progressive and not a static lesion.Citation2 The presence of glomerular sclerosis may be secondary to hypertension and advanced state of TIN. Thus, glomerular and arteriolar sclerosis in the non-hypoplastic part of the kidney demonstrates why nephrectomy does not usually abolish the hypertension and may also explain the functional impairment in the healthy kidney.Citation15
The case we reported here indicates that Ask-Upmark kidney should be considered as potential cause of hypertension and RF both in children and adults. Renal biopsy is necessary for diagnosis and may consent to normalize BP by nephrectomy; however, if renal damage is severe and progressive with TIN, as in our patient, surgical management is excluded and renal transplant should be considered.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Ask-Upmark E. Uber juvenile maligne Nephrosclerose und ihr Verhaltris zu Storunger in der Nierenentwicklung. Acta Path Microbiol Scand. 1929;6:383–442.
- Jennette JC, Olson JL, Schwartz MM, . Pyelonephritis and other infections, reflux nephropathy, hydronephrosis, and nephrolithiasis. In: Lippincott-Raven, ed. Heptinstall’s Pathology of the Kidney. 5th ed., Philadelphia, PA: Lippincott-Raven; 1998:992–1083.
- Marwali MR, Rossi NF. Ask-Upmark kidney associated with renal and extrarenal arterial aneurysms. Am J Kidney Dis. 1999;33(4):E4.
- Shindo S, Bernstein J, Arant BS Jr. Evolution of renal segmental atrophy (Ask-Upmark kidney) in children with vesicoureteric reflux: Radiographic and morphologic studies. J Pediatr. 1983;102(6):847–854.
- Arant BS Jr., Sotelo-Avila C, Bernstein J. Segmental “hypoplasia” of the kidney (Ask-Upmark). J Pediatr. 1979;95(6):931–939.
- Batzenschlager A, Blum E, Weill-Bousson M. The unilateral small kidney. (Anatomoclinical study). Acquired unilateral small kidney. Ann Anat Pathol. 1962;7:427–469.
- Royer P, Habib R, Broyer M, Nouaille Y. Segmental hypoplasia of the kidney in children. Adv Nephrol Necker Hosp. 1971;1:145–159.
- Matsuoka H, Nakashima Y, Oshima K. Prognostic significance of the number of renal glomeruli in reflux nephropathy. BJU Int. 2006;98(1):172–176.
- Peters C, Rushton HG. Vesicoureteral reflux associated renal damage: Congenital reflux nephropathy and acquired renal scarring. J Urol. 2010;184(1):265–273.
- Sugimoto T, Tanaka Y, Nitta N, Uzu T, Nishio Y, Kashiwagi A. Renal segmental hypoplasia, Ask-Upmark kidney, in a patient with adult-onset hypertension. Intern Med. 2006;45(19):1101–1102.
- Fuke T, Sugimoto T, Ugi S, . Renal segmental hypoplasia, Ask-Upmark kidney, in a patient with microalbuminuric hypertensive type 2 diabetes mellitus. Diabetes Res Clin Pract. 2008;80(1):e22–e24.
- Godard C, Vallotton MB, Broyer M. Plasma renin activity in segmental hypoplasia of the kidneys with hypertension. Nephron. 1973;11(5):308–317.
- Babin J, Sackett M, Delage C, Lebel M. The Ask-Upmark kidney: A curable cause of hypertension in young patients. J Hum Hypertens. 2005;19(4):315–316.
- Tash JA, Stock JA, Hanna MK. The role of partial nephrectomy in the treatment of pediatric renal hypertension. J Urol. 2003;169(2):625–628.
- Rosenfeld JB, Cohen L, Garty I, Ben-Bassat M. Unilateral renal hypoplasia with hypertension (Ask-Upmark kidney). Br Med J. 1973;2(5860):217–218.