Abstract
In this article, we report a patient with Crush Syndrome (CS) who developed acute renal failure (ARF) and acute pancreatitis. Continuous venovenous hemofiltration (CVVH) and intermittent hemoperfusion (HP) were successfully performed in this patient and satisfactory effects were achieved. The treatment of this patient suggested that early intervention with continuous renal replacement therapy (CRRT) may be useful and a multiple-mode treatment may be a better choice.
INTRODUCTION
Crush Syndrome (CS) is the systemic manifestation of the muscle breakdown caused by the prolonged compression of limbs and the trunk during a crush injury. CS is characterized by acute renal failure (ARF), metabolic acidosis, hypovolemic shock, and hyperkalemia, which are induced by the circulation of decomposition products in blood.Citation1 CS always occurs with multiple organ dysfunction, which creates severe clinical complications. The mortality due to ARF related to CS remains high, despite early intervention in intensive care units.Citation2 Continuous renal replacement therapy (CRRT) is an effective treatment for severely and critically ill patients and has been widely applied in ARF. However, the time of intervention and the type of CRRT remain controversial.
We report a CS patient with acute pancreatitis who was successfully treated using continuous venovenous hemofiltration (CVVH) and intermittent hemoperfusion (HP).
CASE REPORT
The patient was a 34-year-old male who was buried under a collapsed building for approximately 8 h after the Yushu earthquake in Qinghai Province. The patient presented with impercipience in the lower limbs after rescue, and he was immediately transferred to our hospital. The patient presented with oliguria (urine output <17 mL/h) under admission to our hospital.
The patient was alert and communicative upon examination. The patient exhibited the following characteristics: a temperature of 36.7°C, a blood pressure of 135/94 mmHg, a pulse of 102 beats per minute, a respiratory rate of 21 breaths per minute, and an oxygen saturation of 97% while breathing ambient air.
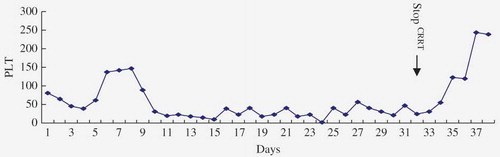
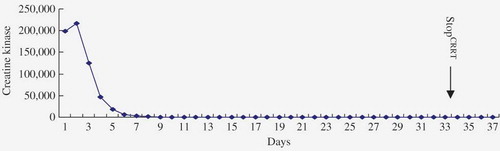
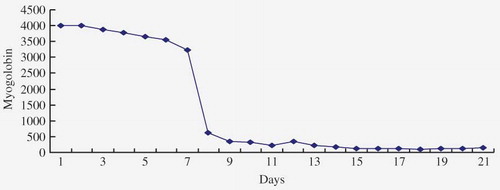
Massive ecchymosis appeared on the skin of his right lower limb, which was severely swollen. The dorsalis pedis artery was also clearly pulsating. The muscle tension of the lower limbs was decreased to 1 on a scale of 0 to 4. Chest auscultation revealed diffused crackles on both sides of the lungs. The heart sounds were normal and the abdomen was soft and tender. Laboratory tests indicated hemoglobin of 168 g/L, platelets of 80 × 109/L, white blood cells (WBCs) of 12.43×109/L, alanine aminotransferase (ALT) of 2484 IU/L, aspartate aminotransferase (AST) of 1028 IU/L, urea of 22.85 mmol/L, serum creatinine of 501 μmol/L, creatine kinase (CK) of 198,751 IU/L, myoglobin of 4000 ng/mL, sodium of 130 mmol/L, chlorine of 102.3 mmol/L, potassium of 7.4 mmol/L, and calcium of 1.59 mmol/L. The patient was diagnosed with CS, hyperkalemia, and right lower limb osteofascial compartment syndrome. CVVH [Diapact CRRT machine (Prismaflex; Gambro, Lund, Sweden) and Fresenius AV 600 hemofilter (Fresenius, Oberursel, Germany) (1.4 m2)] was applied with a 3000 mL/h pre-dilution replacement fluid at a 220 mL/min blood flow rate and 125 mL/h initial ultrafiltration which was adjusted by intravenous fluid input and central venous pressure. HP, using an endotoxin absorption cartridge (Toraymyxin PMX-20; Toray Industries Inc., Tokyo, Japan), was performed for 4 h daily in the blood fluid circuit prior to the hemofiltration. Low molecular weight heparin was used as an anticoagulant during HP. Regional citrate anticoagulation was used for hemofiltration. Nutritional support was supplied. A fat-rich diet induced abdominal distention and pain after 5 days of treatment. The abdomen was tender without shifting dullness on inspection. An abdominal computed tomography scan revealed pancreatic swelling. Laboratory test indicated a serum amylase of 821 IU/L and serum lipase of 1104 IU/L and the patient was diagnosed with acute pancreatitis. Subsequently, antibiotics were administered and CVVH + HP were performed unremittingly. The abdominal pain was gradually reduced. Both serum amylase (AMY) and serum lipase (LIP) decreased after 5 days. Thrombocytopenia presented during the treatment period (), which was treated using 2–4 platelet transfusions per day. Serum CK and myoglobin gradually decreased to normal levels ( and ). The urine output increased to 1100 mL/day on day 28 and CRRT was suspended on day 33. Laboratory tests demonstrated serum urea of 22.06 mmol/L and creatinine of 216.5 μmol/L. The patient was discharged and freely moving. All the laboratory tests were normal at 1-month follow-up.
DISCUSSION
CS is the second most common cause of death following earthquake injury. Muscular cells are damaged by the prolonged and extensive pressure or crushing of the body, and they subsequently release their contents. Crush injury bears many similarities to traumatic rhabdomyolysis. Cellular death followed by myonecrosis and ischemic injury, which are associated with an increased capillary permeability (>30–40 mmHg). This increased permeability leads to edema and sufficiently elevates compartment pressure to create compartment tamponade.Citation3 Patients with limbs compartment tamponade require fasciotomy or amputation. The blood reperfuses the tissue after the compression is released and the necrotic tissue releases myoglobin, lactic acid, CK, potassium, and other toxic substances into the bloodstream. In addition, abundant oxygen is available for recombination into oxygen-free radicals after reperfusion which further damage the cell membrane and lead to multiple organ failure, shock, hyperkalemia, metabolic acidosis, and ARF.Citation4
The severity of CS is related to the magnitude and duration of the compressing force and the bulk of the affected muscle. The incidence of ARF is 22–30%.Citation5 Multiple factors contribute to the pathophysiology of ARF. Hypovolemia and released vasoactive agents induce renal vasoconstriction. Myoglobin obstructs the renal tubular lumens, which is associated with the direct nephrotoxicity of other substances, such as phosphate and urate.Citation6,7 Nitric oxide (NO) from macrophages accumulates in crush injured musculature.Citation8 NO exerts cytotoxic effects on the renal tubular system which contributes to the progress of ARF.Citation8 Hyperkalemia and a high blood urea nitrogen/creatinine (BUN/CR) presented rapidly in our patient after rescue which was complicated by acute pancreatitis. The proinflammatory cytokines and activated inflammatory cells that are induced by the first injury lead to an imbalance in anti-inflammation, inflammation, and system stress conditions, which may underlie the patient’s condition. However, the mechanism of the second attack was uncertain. Deitch et al.Citation9 emphasized that effective treatment should be employed immediately after injury to control systemic inflammation.
Different types of renal replacement therapy (RRT) [intermittent RRT (IRRT) and continuous RRT] are generally applied to severe ARF. CRRT exhibits more advantages in CS with acute pancreatitis compared with IRRT, including improved hemodynamics, easier fluid removal, flexibility with parenteral nutrition, and the steady removal of inflammation.Citation10 Myoglobin, a 17 kDa molecule, cannot be removed by hemodialysis, but RRT is an effective treatment for removal of myoglobin and cytokines, including interleukin-1 (IL-1), IL-6, and TNF-alpha, which are increased in sepsis and related to a poor prognosis.Citation11 Severe infection was another important etiological factor in this case. Endocrine activity is relevant to the pathogenesis of severe sepsis, and elevated endocrine activity is associated with a poorer clinical outcome.Citation12 Multiple modes of blood purification using CVVH and HP were performed to control endocrine activity. A hemofilter with a high molecular weight cut-off level (65 kDa) was used during CVVH, which promoted the removal of small-to-medium-sized solutes such as cytokines. A column containing a special fiber composite of immobilized antibiotic polymyxin B was used during the HP. Polymyxin B effectively binds endotoxins in vitro and in vivo.Citation13 A randomized controlled trial in 2009 Early Use of Polymyxin B Hemoperfusion in Abdominal Sepsis (EUPHAS) studyCitation14 demonstrated that polymyxin B HP improved organ dysfunction and reduced the 28-day mortality in patients with severe sepsis from intra-abdominal Gram-negative infections. Furthermore, polymyxin B HP in vivoCitation15 effectively lowers the proinflammatory cytokines. HP overcomes the lower dose of replacement and reduces the loss of blood constituents and the contagious risk compared with plasmapheresis. The symptoms of pancreatitis and CS (e.g., high CK, myoglobin, and BUN/CR levels) were significantly relieved after the treatment combination.
The impact of different types of RRT on ARF remains controversial. No uniform strategy (i.e., an exclusive choice for severe ARF) exists for clinical decisions in severe ARF, including the choice of modality, the timing of initiation, and dose. Several randomized and prospective clinical trials in small samples have not demonstrated any difference between CRRT and intermittent hemodialysis (IHD).Citation16 However, two aspects should be considered. First, the curative effect could be underestimated. Second, trials should not consider the disease severity or specialty. Early CRRT treatment stabilization of the general patient status and classic intermittent hemodialysis for long-lasting and isolated ARF will be used as complementary extracorporeal treatment modalities in the future.Citation17
CRRT exhibited several drawbacks in this patient, including sustained thrombopenia. Thrombopenia is caused by several factors: the use of anticoagulation agents; alkaline conditions induced by sodium bicarbonate in the replacement fluid that increase the adhesiveness of platelets; the hemofilter membrane accumulation of platelets, which activates the clotting process; and high fluid shear stress, which fractures the platelets. Therefore, the mode, dose, and anticoagulation agent of RRT should be prudently selected.
CONCLUSION
Multiple-mode CRRT is a promising alternative for earthquake injuries complicated by severe CS and acute pancreatitis. The appropriate and timely choice of the blood purification mode is of great importance to the prognosis of these patients.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Kikta MJ, Meyer JP, Bishara RA, . Crush Syndrome due to limb compression. Arch Surg. 1987;122(9):1078–1081.
- Shaw AD, Sjlin SU, McQueen MM. Crush Syndrome following unconsciousness: Need for urgent orthopaedic referral. BMJ. 1994;309(6958):857–869.
- Bywaters EG, Popjak G. Experimental crushing injury: Peripheral circulatory collapse and other effects of muscle necrosis in the rabbit. Surg Gynecol Obstet. 1942;75:612–627.
- Better OS. Rescue and salvage of casualties suffering from the Crush Syndrome after mass disasters. Mil Med. 1999;164(5):366–369.
- Zager RA. Rhabdomyolysis and myohemoglobinuric acute renal failure. Kidney Int. 1996;49:314–326.
- Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009;361:62–72.
- Vanholder R, Sever MS, Erek E, Lameire N. Acute renal failure related to the Crush Syndrome: Towards an era of seismo-nephrology. Nephrol Dial Transplant. 2000;15(10):1517–1521.
- Stein H, Hoerer D, Weisz I, . Musculoskeletal injuries in earthquake victims: An update on orthopedic management. Orthopedics. 2000;23(10):1085–1087.
- Deitch EA. Spontaneous lymphocyte activity: An important but neglected component of the immunologic profile of the thermally injured patient. Surgery. 1985;98(3):587–593.
- Jakob SM, Frey FJ, Uehlinger DE. Does continuous renal replacement therapy favourably influence the outcome of the patients? Nephrol Dial Transplant. 1996;11(7):1250–1255.
- Erek E, Sever MS, Serdengecti K, . An overview of morbidity and mortality in patients with acute renal failure due to Crush Syndrome: The Marmara earthquake experience. Nephrol Dial Transplant. 2002;17:33–40.
- Marshall JC, Foster D, Vincent JL, . Diagnostic and prognostic implications of endotoxemia in critical illness: Results of the MEDIC study. J Infect Dis. 2004;190(3):527–534.
- Cruz DN, Perazella MA, Bellomo R, . Effectiveness of polymyxin B-immobilized fiber column in sepsis: A systematic review. Crit Care. 2007;11(2):R47.
- Cruz DN, Antonelli M, Fumagalli R. Early use of polymyxin B hemoperfusion in abdominal septic shock: The EUPHAS randomized controlled trial. J Am Med Assoc. 2009;301(23):2445–2452.
- Iba T, Okamoto K, Kawasaki S. Effect of hemoperfusion using polymyxin B-immobilized fibers on non-shock rat sepsis model. J Surg Res. 2011;171(2):755–761.
- Augustine JJ, Sandy D, Seifert TH, . A randomized, controlled trial, comparing intermittent with continuous venovenous dialysis in patients with AKI. Am J Kidney Dis. 2004;44(6):1000–1007.
- Lins RL, Elseviers MM, Van der Niepen P, . Intermittent versus continuous renal replacement therapy for acute kidney injury patients admitted to the intensive care unit: Results of a randomized clinical trial. Nephrol Dial Transplant. 2009;24(2):512–518.