Abstract
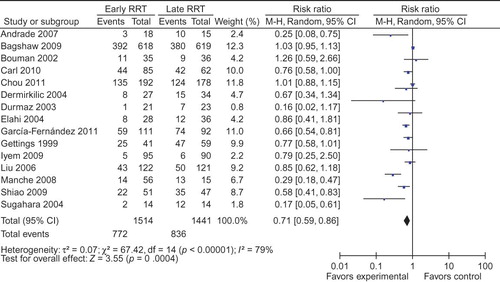
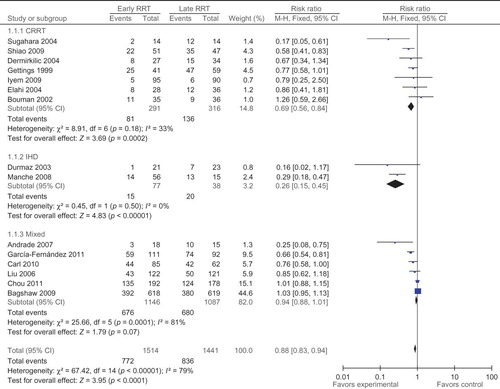
Objective: The aim of the study is to summarize the effects of timing of initiation of renal replacement therapy (RRT) on mortality. Methods: A systematic search for randomized controlled trials (RCTs) and other clinical studies was performed without language restriction in PubMed, Web of Science, and Embase. We estimated pooled relative risk ratios (RRs) and 95% confidence intervals (CIs) using fixed effects model or random effects model as appropriate. Heterogeneity, publication bias, and subgroup analyses were conducted. Results: We analyzed the date extracted from 15 studies (3 RCTs, 2 prospective, and 10 retrospective comparative cohort studies) with a total of 2955 patients. Overall, 51.0% (772/1514) patients died in the “early” RRT group compared with 58.0% (836/1441) in the “late” RRT group. The pooled RR was 0.71 (95% CI: 0.59, 0.86), but the heterogeneity existed (p < 0.00001). Subgroup analysis based on modality did not record heterogeneity across trials. In continuous RRT (CRRT) group (n = 607), patients treated with “early” CRRT suggested a significant decrease in mortality compared with those in “late” CRRT group (27.8% vs. 43.0%) and the RR was 0.69 (95% CI: 0.56, 0.84) without evidence of heterogeneity (I2 = 33%, p = 0.18). In intermittent hemodialysis (IHD) group (n = 115), the RR was 0.26 (95% CI: 0.15, 0.45) without evidence of heterogeneity (I2 = 0%, p = 0.50). In the mixed group, heterogeneity existed. Conclusion: “Early” CRRT and “early” IHD both could reduce the mortality of patients with acute kidney injury compared with “late” CRRT or IHD.
Although the renal replacement therapy (RRT) technology has been improved greatly and has been widely used in acute kidney injury (AKI) patients, the mortality caused by AKI was still very high in intensive care unit (ICU) during the last several decades.Citation1 Recently, it is controversial whether “early” RRT can reduce the mortality of patients with AKI compared with “late” RRT. One prospective randomized trialCitation2 could not show a significant survival benefit for early institution of RRT in patients with ARF, but the other oneCitation3 suggested that the early start dialysis therapy might be preferable for improvement of survival of the patients with AKI. Thus, we undertook a systemic review and meta-analysis to obtain current estimate on the effects of initiation time of RRT on mortality of patients with AKI.
SUBJECTS AND METHODS
Literature Search Strategy
We conducted a systematic search for clinical trials of PubMed, Web of Science, and Embase from 1990 to August 2011, using the following keywords together with RRT: timing, initiation, AKI, and ICU. There was no language restriction on the research. Details of the searching process are shown in .
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) randomized controlled trials (RCTs), prospective or retrospective studies; (2) comparing mortality and other clinical outcomes of “early” and “late” RRTs of patients with AKI. We excluded studies not accessible to full research data. Review, case report, letter, and editorial were excluded.
Data Extraction
Two authors (Xuan Wang and Wei Jie Yuan) independently reviewed each report found by the searching strategy, and results obtained by them were compared and discussed to reach an agreement. The study selection, data extraction, and reporting of results were all based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses checklist.Citation4 Data extracted included basic characteristics (publication year, study design, mean age, gender, total number of patients, and biochemical parameters at the initiation of RRT) and main characteristics (modality, patient population, and definition of “early” and “late” RRT). The main outcome was the mortality.
Statistical Analysis
Pooled estimates of the risk ratio (RR) and relevant 95% confidence interval (CI) were obtained by using random effect model or fixed effect model. Heterogeneity across trials was evaluated with Q and I2 statistic. I2 values ranged from 0% to 100%: 0% suggested no observed heterogeneity, 25–49% suggested low, 50–74% moderate, and ≥75% high heterogeneity.Citation5 p-Value <0.1 was defined as significant heterogeneity. If heterogeneity existed, a random effect model was used to assess the overall estimate. Otherwise, a fixed effect model was chosen.
Subgroup analysis was performed to account for heterogeneity. Despite potential advantages of an improvement in patients’ outcomes, using continuous RRT (CRRT) compared with intermittent hemodialysis (IHD) remains controversial. Two trials have studied the effects of CRRT versus IHD on the mortality of patients with AKI,Citation6,7 so we specified subgroup analysis based on the modality studies with all patients using CRRT listed in the CRRT group and studies with patients using the modality of IHD made up of the IHD group and in the remaining studies, a part of patients used CRRT, the others might use IHD or peritoneal dialysis (PD) or sustained low-efficiency dialysis (SLED), which were included in the mixed group.
Sensitivity analyses were performed to assess the effects of selected measures of study quality and clinical factors on heterogeneity. The influence of individual study on the conclusion was estimated by deleting the study from the analysis and noting the degree to which the pooled effect size changed. We considered a study influential if the exclusion changed our conclusion or the effect estimate by at least 20%.
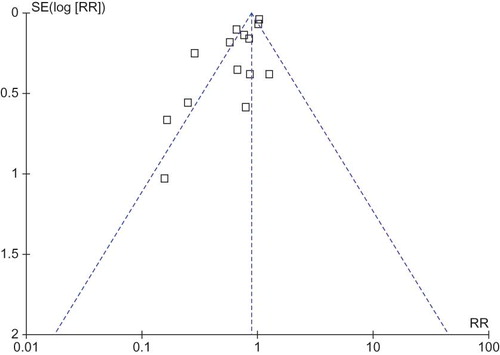
A funnel plot was used to assess the presence of publication and other reporting biases by plotting the standard error against the log RR. The shape of the funnel plot was symmetrical, indicating no significant publication bias. All analyses were performed using the software Review Manager 5.0 (Cochrane Collaboration, Oxford, UK).
Assessment of Methodological Quality
For the three RCTs, we use special criteria (sequence generation, concealment allocation, blinded assessment, incomplete outcome data, and free of selective reporting) to assess their quality, rather than any scale with regard to the limitation of this method.Citation8 The remaining 12 nonrandomized trials were evaluated in a descriptive fashion similar to a previous study,Citation9 including the reported criteria for RRT initiation, comparability of intervention/control arms, and a description of dropouts.
RESULTS
Study Selection
Our search strategy yielded 1238 citations shown in . We retrieved 47 citations for detailed evaluation, of which 32 were excluded. Fifteen studies,Citation2,3,10–22 which included 3 RCTs, 2 prospective and 10 retrospective comparative cohort studies, met the inclusion criteria. All these studies were written in English.
Characteristics of the Studies
The basic characteristics of the studies were reported in . A total of 2955 patients were enrolled. showed the modality of RRT, population, and the definition of “early” and “late” RRTs. Patients in seven studiesCitation2,3,13–15,18,19 used CRRT and patients in two studiesCitation10,17 used IHD. In the remaining studies,Citation11,12,16,20–22 a part of patients used CRRT modality, and the others used IHD or SLED or PD modality. The study conducted by Bouman et al.Citation2 included three treatment strategies of early high-volume hemofiltration, early low-volume hemofiltration, and late low-volume hemofiltration, and the early high-volume hemofiltration strategy was excluded from our analyses.
Table 1. The basic characteristics of studies included in meta-analysis.
Table 2. The main characteristics of studies included in meta-analysis.
Effects of Initiation Time of RRT on Mortality
shows the mortalities of individual studies and pooled analysis. The statistic p for heterogeneity is lower than 0.00001 (); thus, we used the random effects model. Overall, 51.0% (772/1514) patients died in the “early” RRT group compared with 58.0% (836/1441) in the “late” RRT group. The pooled RR was 0.71 (95% CI: 0.59, 0.86), indicating a statistically significant beneficial effect of “early” RRT on mortality. But internal heterogeneity existed.
Subgroup Analysis
To investigate the factors that may result in heterogeneity, we performed subgroup analysis based on the modality of RRT. In the CRRT group, there were seven studies with 607 patients. Patients treated with “early” CRRT had a lower mortality (27.8%) compared with those in the “late” CRRT group (43.0%), and statistical significance was reached (RR 0.69; 95% CI: 0.56, 0.84). There was no statistical heterogeneity (I2 = 33%, p = 0.18). In the IHD group, there were only two studies with 115 patients. One study by Durmaz et al.Citation10 showed no protective effect (RR 0.16; 95% CI: 0.02, 1.17), whereas the other study by Manche et al.Citation17 suggested some benefits (RR 0.29; 95% CI: 0.18, 0.47). As there was no statistical heterogeneity (I2 = 0%, p = 0.50), the two trials were pooled. Patients treated with “early” IHD suggested a significant decrease in mortality compared with those in the “late” IHD group (19.5% vs. 52.6%). The pooled RR was 0.26 (95% CI: 0.15, 0.45), confirming the beneficial effects by “early” Hiding mixed group; there were six studies with 2233 patients. The pooled RR was 0.94 (95% CI: 0.88, 1.01), indicating no favor. It was confirmed that heterogeneity existed (I2 = 79%, p < 0.00001). And we did not conduct meta-regression analysis to explore the factors causing heterogeneity ().
Assessment of Methodological Quality
The quality of the included studies was relatively low ( and ). In the three RCTs, only Durmaz et al.Citation10 described the special method of randomization, the others just mentioned that the patients were randomized into one of the groups. Double blinding and allocation concealment were impossible; all of the three studiesCitation2,3,10 used open-label design. Of the 12 nonrandomized trials, only 4Citation11,12,19,21 had a prospectively assembled control group and 2 studiesCitation12,14 accounted for withdrawals and dropouts.
Table 3. Quality assessment of the three randomized controlled trials.
Table 4. Quality assessment of the remaining 12 nonrandomized trials.
Sensitivity and Influence Analysis
The influence of each study was examined by omission from the analysis. Omission of any study in the CRRT group did not result in a change of the conclusion. In the IHD group, there were only two studies. The study by Durmaz et al.Citation10 showed no significant benefit of “early” IHD compared with “late” Hiding mixed group; the conclusion did not change without any one study.
Publication Bias
Publication bias was evaluated using a funnel plot (). The shape of the funnel plot was symmetrical, indicating no significant publication bias. Because of the small number of studies that met our inclusion criteria, publication bias was of concern.
DISCUSSION
The agreeable initiation time of RRT in patients with AKI remained uncertain. The initiation of RRT is extremely variable and based primarily on empiricism, local institutional practice, and resources.Citation23,24 There is also no consensus that “early” RRT has beneficial effect on mortality.
Our meta-analysis combined the results of 15 studies with 2955 patients. We revealed that “early” RRT could reduce mortality of patients with AKI, but heterogeneity across studies was found. Exploring the sources of heterogeneity by the subgroup analysis, we found that the modality influenced the heterogeneity. Therefore, we analyzed the effects in the subgroups of CRRT, IHD, and mixed.
Heterogeneity was not found in CRRT and IHD groups. The results suggested that in the CRRT group, “early” CRRT had beneficial effect on the mortality of patients with AKI (RR 0.69; 95% CI: 0.56, 0.84). We think that “early” CRRT could clear the inflammatory factor away effectively and timely. Inflammatory factors are now thought of as an important factor contributing to AKI. Removal of inflammatory factor may stop the injury of kidney and reduce mortality. “Early” CRRT also could clear wastes of body away which could aggravate the renal function. Similarly, in the IHD group, “early” IHD could also improve the survival (RR 0.26; 95% CI: 0.15, 0.45). However, in the IHD group, there were only two studies. The study by Durmaz et al.Citation10 did not confirm the conclusion; further investigations are required to explore the effect. Karvellas et al.Citation9 and Seabra et al.Citation25 had the same opinion that early institution of RRT in critically ill patients with AKI may have a measurable benefit on survival. However, compared with these meta-analysis,Citation9,25 we have two strengths. One was that we found the modality was the factor that resulted in heterogeneity, but neither Karvellas et al.Citation9 nor Seabra et al.Citation25 could succeed in finding the factors. The other was we have included two new clinical studiesCitation21,22 published recently, which made our results more convincing.
Our meta-analysis had some limitations. First, there were only 3 RCTs, the other 12 studies were non-RCTs, and the quality of many were not very high. Second, because of the small number of studies that met our inclusion criteria, publication bias existed. As a consequence, the beneficial effect of “early” RRT on mortality may be overstated compared with “late” RRT. Third, we did not perform meta-regression to assess the factors that resulted in heterogeneity; we specified subgroup analysis limited to patients with CRRT or IHD according to the opinion of some studies.Citation6,7
In conclusion, our study suggested that no matter “early” CRRT or “early” IHD both could reduce the mortality of patients with AKI. But due to the limitations of this meta-analysis, more prospective randomized trials are needed to confirm the results.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Uchino S, Kellum JA, Bellomo R, . Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators: Acute kidney injury in critically ill patients: a multinational, multicenter study. J Am Med Assoc. 2005;294:813–818.
- Bouman CS, Oudemans-Van Straaten HM, Tijssen JG, . Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: A prospective, randomized trial. Crit Care Med. 2002;30:2205–2211.
- Sugahara S, Suzuki H. Early start on continuous hemodialysis therapy improves survival rate in patients with acute renal failure following coronary bypass surgery. Hemodial Int. 2004;8:320–325.
- Moher D, Liberati A, Tetzlaff J, . Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012.
- Higgins JP, Thompson SG, Deeks JJ, . Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560.
- Uehlinger DE, Jakob SM, Ferrari P, . Comparison of continuous and intermittent renal replacement therapy for acute renal failure. Nephrol Dial Transplant. 2005;20:1630–1637.
- Vinsonneau C, Camus C, Combes A, . Continuous venovenous hemodiafiltration versus intermittent hemodialysis for acute renal failure in patients with multiple-organ dysfunction syndrome: A multicentre randomized trial. Lancet. 2006;368:379–385.
- Jüni P, Witschi A, Bloch R, . The hazards of scoring the quality of clinical trials for meta-analysis. J Am Med Assoc. 1999;282:1054–1060.
- Karvellas CJ, Farhat MR, Sajjad I, . A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: A systematic review and meta-analysis. Crit Care. 2011;15:R72.
- Durmaz I, Yagdi T, Calkavur T, . Prophylactic dialysis in patients with renal dysfunction undergoing on-pump coronary artery bypass surgery. Ann Thorac Surg. 2003;75:859–864.
- Liu KD, Himmelfarb J, Paganini E, . Timing of initiation of dialysis in critically ill patients with acute kidney injury. Clin J Am Soc Nephrol. 2006;1:915–919.
- Bagshaw SM, Uchino S, Bellomo R, . Timing of renal replacement therapy and clinical outcomes in critically ill patients with severe acute kidney injury. J Crit Care. 2009;24:129–140.
- Gettings LG, Reynolds HN, Scalea T. Outcome in post-traumatic acute renal failure when continuous renal replacement therapy is applied early vs. late. Intensive Care Med. 1999;25:805–813.
- Elahi MM, Lim MY, Joseph RN, . Early hemofiltration improves survival in post-cardiotomy patients with acute renal failure. Eur J Cardiothorac Surg. 2004;26:1027–1031.
- Demirkilic U, Kuralay E, Yenicesu M, . Timing of replacement therapy for acute renal failure after cardiac surgery. J Card Surg. 2004;19:17–20.
- Andrade L, Cleto S, Seguro A. Door-to-dialysis time and daily hemodialysis in patients with leptospirosis: Impact on mortality. Clin J Am Soc Nephrol. 2007;2:739–744.
- Manche A, Casha A, Rychter J, . Early dialysis in acute kidney injury after cardiac surgery. Interact Cardiovasc Thorac Surg. 2008;7:829–832.
- Iyem H, Tavli M, Akcicek F, . Importance of early dialysis for acute renal failure after an open-heart surgery. Hemodial Int. 2009;13:55–61.
- Shiao CC, Wu VC, Li WY, . Late initiation of renal replacement therapy is associated with worse outcomes in acute kidney injury after major abdominal surgery. Crit Care. 2009;13:R171.
- Carl DE, Grossman C, Behnke M, . Effect of timing of dialysis on mortality in critically ill, septic patients with acute renal failure. Hemodial Int. 2010;14:11–17.
- Chou YH, Huang TM, Wu VC, . Impact of timing of renal replacement therapy initiation on outcome of septic acute kidney injury. Crit Care. 2011;15:R134.
- García-Fernández N, Pérez-Valdivieso JR, Bes-Rastrollo M, . timing of renal replacement therapy after cardiac surgery: A retrospective multicenter Spanish cohort study. Blood Purif. 2011;32:104–111.
- Mehta RL, Pascual MT, Soroko S, . Spectrum of acute renal failure in the intensive care unit: The PICARD experience. Kidney Int. 2004;66:1613–1621.
- Ricci Z, Ronco C, D’Amico G, . Practice patterns in the management of acute renal failure in the critically ill patient: An international survey. Nephrol Dial Transplant. 2006;21:690–696.
- Seabra VF, Balk EM, Liangos O, . Timing of renal replacement therapy initiation in acute renal failure: A meta-analysis. Am J Kidney Dis. 2008;52:272–284.