Abstract
Background: Nephrologist-based multidisciplinary care (MDC) has a positive impact on slowing chronic kidney disease (CKD) progression. However, the benefits of MDC in patients with stage 5 CKD remain unclear. Methods: Stage 5 CKD patients who visited the Chang Gung Memorial Hospital, Chiayi, Taiwan during the period of 2002–2008 were enrolled. The incident dialysis and medical cost were compared between MDC recipients and nonrecipients. The MDC recipients were divided into two groups by educational duration to observe the clinical renal outcome and medical care expenses. The effect of MDC on renal disease progression was also compared in MDC recipients with and without diabetes. Results: Out of 307 patients, 171 received MDC. For MDC recipients, the temporary usage of catheter was reduced (54.7% vs. 79.4%, p < 0.001), the hospital stay was shorter (18.64 ± 1.20 vs. 24.63 ± 1.22 months, p = 0.001), and the total medical cost was lower [New Taiwan dollars (NTD) 105,948.54 ± 9,967.22 vs. NTD 160,388.61 ± 16,373.97, p = 0.005] than for nonrecipients. Out of the 171 MDC recipients, those with MDC for more than 1 year had slower renal disease progression (0.76 ± 0.27 mL/min per 1.73 m2 per year) and had an estimated per- capita annual cost savings of about NTD 336,500.66. MDC recipients with diabetes had a higher risk of requiring dialysis than those without diabetes. Conclusions: MDC could significantly reduce temporary use of the catheter, hospital stay, and total medical costs in patients with stage 5 CKD. Furthermore, longer (>1 year) MDC could preserve renal function and deliver annual medical cost savings.
INTRODUCTION
According to the US Renal Data System Annual Data Report, Taiwan had the world’s highest prevalence (2,584 per million population) and the third highest incidence (361 per million population) of end-stage renal disease (ESRD) in 2010.Citation1 Multiple factors contribute to this high rate of ESRD and a large population of patients with chronic kidney disease (CKD) may also account for this high rate. CKD is a common disease with a complex set of physiologic consequences. In advanced cases, patients require renal replacement therapy to survive. In Taiwan as well as the rest of the world, the prevalence of ESRD continues to rise and leads to increased medical costs.Citation1 The direct financial cost of ESRD is substantial, with the Bureau of National Health Insurance (BNHI) spending more than 25 billion New Taiwan dollars (NTD) per year on dialysis coverage, which represents an expenditure of 7.2% of the total budget for just 0.15% of the general population. The burden of ESRD in Taiwan is among the heaviest in the world, reflecting the expense associated with renal replacement therapy. Therefore, in recent years, the focus has shifted to optimizing care before beginning dialysis to treat ESRD or, more importantly, improving care throughout all stages of CKD.
Over the past several years, multidisciplinary care (MDC) was chosen to be an approach for the management of CKD populations with a positive impact on both the physical condition and medical economic benefits.Citation2 Ghossein et al.Citation3 reported that glomerular filtration rate (GFR) decreased at a slower rate in patients with stage 3 CKD, and that patients with CKD stages 4 and 5 had a more stable estimated GFR (eGFR) when an MDC team was involved throughout the 15-month follow-up. In addition to a study, which showed an improvement in the outcome of CKD patients,Citation4 a controlled cohort studyCitation5 showed that the change in renal function of patients with CKD stages 3–5 was 0.008 ± 0.139 mL/min per 1.73 m2 per month while receiving the MDC during 12 months of the follow-up. Often the CKD patients were referred at an advanced stage of renal failure, only few months before or even a few weeks prior to ESRD. The cost-effectiveness and benefits of the MDC approach for stage 5 CKD patients remain controversial.
The unique purpose of this observational study was to examine the clinical renal outcome as a function of two different clinical courses. Stage 5 CKD patients, in whom incidental dialysis was initiated, were divided into two groups for our comparisons namely those patients who received MDC and those patients who did not. All stage 5 CKD patients who received MDC were also evaluated for an extended period. Our hypothesis suggests that the stage 5 CKD patients who received MDC would have better clinical renal outcomes and incur lower medical expenses than the stage 5 CKD patients who did not receive any such intervention.
MATERIALS AND METHODS
Study Design
We performed a patient-based, retrospective study to investigate the impact of MDC on the delay of renal progression and cost-effectiveness of treatment for patients with advanced CKD. All patients with stage 5 CKD [eGFR < 15 mL/min per 1.73 m2, as determined by a simplified modification of diet in renal disease (MDRD) equation] were categorized according to whether they received MDC at Chang Gung Memorial Hospital, Chiayi, Taiwan, from January 2002 to May 2008. The nephrologist-based MDC team was established in January 2005 with nephrologists, nephrology nurse educators, and renal dietitians being the core members responsible for caring of the CKD patients. All CKD patients were invited to join the MDC program and received CKD educational intervention. Patients who did not receive CKD educational intervention prior to the establishment of the MDC team received care from the same group of nephrologists, but they did not receive nephrology nurse education and dietary counseling from nephrology nurse educators and renal dietitians. Patients aged 18–90 years were included. Because the per cent of peritoneal dialysis (PD) of incident ESRD patients was about 10% in our hospitals, PD patients were not included in this study. Patients with incomplete laboratory data, acute kidney injury, and those lost to follow-up were also excluded. Because all the direct personal identifiers were de-identified, the need to obtain informed consent was waived. This study was approved by the ethics committee of the institutional review board (IRB) at the Chang Gung Memorial Hospital.
Study Subjects
Between January 2002 and January 2005, the patient group that did not receive MDC consisted of 174 incident dialysis patients. The group that received MDC consisted of 202 patients who were further categorized according to the CKD educational intervention duration. In order to allow at least 3–6 months for predialysis education, we chose 1 year [i.e., shorter (<1 year, n = 101) vs. longer (>1 year, n = 101)] as the educational intervention duration to investigate whether the MDC program could improve clinical renal outcomes and reduce medical expenses from January 2005 to May 2008 (). The information collected at incident dialysis included demographic variables, presence of comorbidity, temporary usage of catheter, and the total cost of hospitalization for incidental dialysis. All decisions regarding the initiation or discontinuation of incidental dialysis were made by the treating nephrologist and were based on the criteria mandated by BNHI, Taiwan. For patients receiving MDC, data on kidney function, intervention duration, nutritional status (serum albumin), hemoglobin (Hb), and serum levels of calcium (Ca) and phosphate (P) were collected and compared between the shorter MDC group and longer MDC group.
Service Utilization and Medical Costs
Indicators of service utilization at dialysis initiation included hospitalization length, medicine prescription during hospitalization, dialysis-related surgery (Hickman implantation, double lumen implantation, and shunt creation), Electrocardiography (EKG) examination, an angiography for shunt evaluation, ward cost, nursing, hemodialysis, and total cost. Data on the length of hospitalization were obtained from electronic medical records of the medical institution. If dialysis therapy began during hospitalization, the number of days of hospitalization was calculated starting with the first day of dialysis therapy. The measurement of costs in this study only included direct medical costs for which the study hospitals made claims to the NHI for reimbursement. The salaries and overhead and the indirect costs of the care team were not included.
MDC Program and Quality of PreESRD Care
In the group of stage 5 CKD patients receiving MDC, every patient received clinical evaluation, laboratory examinations, and nursing and dietary education for every 1–2 months. A standardized curriculum and prespecified educational topics were delivered systematically with a teaching time of around 30–40 min at each visit. The CKD educational program contents included educational videos, standardized appropriate printed educational material, pharmacological and dietary interventions required for the management of advanced CKD, and access to review dialysis equipment and basic procedures. Under this program, stage 5 CKD patients were monitored for uremic complications, early referral for creation of dialysis access, pretransplant assessment, and timely initiation of renal replacement therapy. The MDC program was discontinued once renal replacement therapy was initiated for these patients.
Statistical Analysis
The declines in kidney function in all stage 5 CKD patients are represented as the linear equation (). The vertical axis (Y) shows the level of kidney function. The horizontal axis (X) shows time over an interval of several months. The horizontal line corresponds to the level of kidney function at the initiation of dialysis. The rate of decline in GFR is represented as diagonal lines (slope). The linear equation of two variables, x and y, is y = m − bx, where m and b are the designated constants. In this particular equation, the constant b determines the slope, and the constant term m determines the point at which the line crosses the Y-axis, otherwise known as the level of kidney function. Continuous variables are expressed as mean ± standard error (SE) and the categorical variables are given as per cent. The Student’s t-test was used to compare the mean values among the groups. The association between categorical variables was analyzed using the chi-square test. To assess the relationship between the total medical costs and the MDC program, univariate and multivariate odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. Statistical significance was defined as two-tailed p < 0.05. Statistical analysis was performed using the SPSS software package, version 13.0 (SPSS Inc., Chicago, IL, USA).
Figure 2. The effect of MDC duration on the rate of renal progression in stage 5 CKD patients.
The horizontal dotted line corresponds to the level of kidney function at the initiation of dialysis (eGFR = 5 mL/min/1.73 m2). The declines in kidney function are illustrated as diagonal lines.
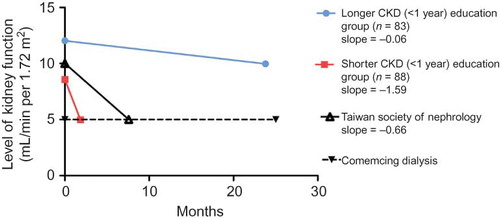
Figure 3. Delivery of annual medical cost savings.
Per capita medical cost savings resulting from longer (>1 year) MDC was estimated for the cases with delayed onset of hemodialysis.
Annual cost savings = delay time (months) × hemodialysis sessions per month × reimbursement ÷ 12 = [(83.33 − 7.57) × 13 × 4100 ÷ 12] = NTD 336,500.66 compared with the cost of care incurred by the Taiwan Society of Nephrology (1 USD = 29.7 NTD).
![Figure 3. Delivery of annual medical cost savings.Per capita medical cost savings resulting from longer (>1 year) MDC was estimated for the cases with delayed onset of hemodialysis.Annual cost savings = delay time (months) × hemodialysis sessions per month × reimbursement ÷ 12 = [(83.33 − 7.57) × 13 × 4100 ÷ 12] = NTD 336,500.66 compared with the cost of care incurred by the Taiwan Society of Nephrology (1 USD = 29.7 NTD).](/cms/asset/5a993d68-304f-4db9-a953-122a468436e9/irnf_a_731997_f0003_b.jpg)
RESULTS
Characteristics of Patients in the CKD NonEducational Intervention and CKD Educational Intervention Groups at Incidental Dialysis Initiation
We compared the characteristics of patients starting dialysis in the CKD noneducational intervention group (n = 136) and the CKD educational intervention group (n = 88). summarizes the demographic data of incidental dialysis initiation for the 224 eligible patients: the average age of the CKD noneducational intervention patients was 64.48 ± 1.12 years. There are more men in the educational group than in the noneducational group (61.4% vs. 45.6%, p < 0.05). The differences between the two study groups with respect to comorbidity were not significant. With respect to the temporary usage of catheters, there was a significant difference in the number of patients in whom dialysis was urgently initiated (i.e., required temporary access) between the two groups (79.4% of patients in the CKD noneducational group vs. 54.7% of patients in the CKD educational group; p < 0.001).
Table 1. Summary of demographics at incidental dialysis initiation in CKD noneducational intervention and CKD educational intervention groups.
The MDC Program Significantly Reduced Total Medical Costs
presents the comparisons of service utilization and medical costs between the two groups at the time of incidental dialysis. The total cost was significantly higher in the CKD noneducational intervention group than in the CKD educational intervention group (NTD 160,388.61 ± 16,373.97 vs. 105,948.54 ± 9967.22, p = 0.005). To evaluate the association between total medical cost and the MDC program, we used a multivariable logistic regression analysis to adjust for the confounding factors. According to the median of total medical cost, which was about NTD 87,850, all the stage 5 CKD patients were divided into two groups: the high medical costs group and the low medical costs group. Before this adjustment, we noted that the stage 5 CKD patients who were not part of the MDC program had a 2.968-fold increase in the medical costs than those of the stage 5 CKD patients who participated in the MDC program (OR = 2.968; 95% CI: 1.817–4.846). We further adjusted the age and gender, and found that stage 5 CKD patients who were not part of the MDC program had a 2.835-fold increase in medical costs than those of the stage 5 CKD patients who participated in the MDC program (OR = 2.835; 95% CI: 1.723–4.663; ).
Table 2. Unadjusted and adjusted OR and 95% CI of high medical costsFootnotea associated with stage 5 CKD patients without the MDC program.
Comparison of Laboratory Data and Renal Function in Stage 5 CKD Patients with Shorter and Longer MDC
Of the patients who received MDC (), the mean ages and comorbidities of the two groups were not significantly different. In the group that received longer (>1 year) MDC, 39.9% of the patients were men. The longer MDC group had a higher serum Hb level (9.57 ± 0.15 vs. 8.83 ± 0.17 g/dL, p = 0.003) and a higher serum albumin level (3.24 ± 0.05 vs. 2.97 ± 0.08 g/dL, p = 0.007) than the shorter MDC group. However, the serum Ca levels and P levels were not statistically significant between the two groups.
Table 3. The effect of MDC duration on the laboratory data and the rate of renal disease progression in stage 5 CKD patients between 1 January 2005 and 31 May 2008.
Table 4. The effect of MDC on the rate of renal progression in stage 5 CKD patients with DM and without DM between 1 January 2005 and 31 May 2008.
The patients in both the groups with advanced CKD, who were to begin receiving MDC, had different levels of kidney function (8.05 ± 0.30 vs. 10.39 ± 0.31 mL/min per 1.73 m2, p < 0.001) and changes in renal function, as determined by the eGFR, were significantly larger in the shorter MDC group than in the longer MDC group (19.12 ± 1.05 vs. 0.76 ± 0.27 mL/min per 1.73 m2 per year, p < 0.001). The mean durations of CKD educational intervention were 1.75 ± 0.07 months and 23.43 ± 0.98 months for the shorter and longer MDC groups, respectively (p < 0.001). In the group with the shorter MDC, the kidney function declined more rapidly, and these patients required dialysis earlier than patients who received longer MDC (mean eGFR = 4.94 ± 0.21 mL/min per 1.73 m2). The calculated slopes of renal function decline in the groups with shorter and longer MDC were −1.59 and −0.06, respectively.
The Effectiveness of MDC on the Rate of Renal Progression in Stage 5 CKD Patients with and without Diabetes Mellitus
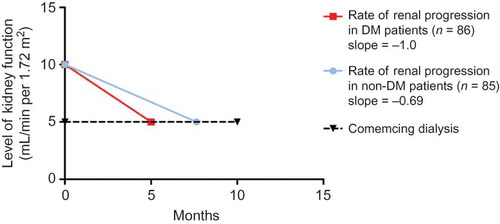
shows the effectiveness of MDC on the rate of renal progression in stage 5 CKD patients with diabetes mellitus (DM) (n = 86) and without DM (n = 85). The differences in the mean age and gender distribution between the DM and nonDM groups were not significant. When the stage 5 CKD was detected in patients entering the CKD educational intervention, those with DM and those without DM had different levels of kidney function (9.73 ± 0.31 vs. 8.64 ± 0.34 mL/min per 1.73 m2, p = 0.02), and the change in eGFR in the DM group was significantly faster than in the nonDM group (12.03 ± 1.28 vs. 8.37 ± 1.22 mL/min per 1.73 m2 per year, p = 0.04). The mean duration of MDC was 9.96 ± 1.16 months in the DM group and 14.60 ± 1.49 months in the nonDM group (p = 0.01). These data suggest that the stage 5 CKD patients with DM had a higher risk of requiring dialysis than the nonDM stage 5 CKD patients.
DISCUSSION
Globally, the burden of CKD and ESRD has substantially increased.Citation6,7 A recent comprehensive reviewCitation8 reported that several pharmacological and nonpharmacological interventions for patients with stages 1–4 CKD were cost-effective. However, those with stage 5 CKD incur substantial costs and these expenses increase with disease progression.Citation9–12 Our study showed that nephrologist-based MDC could significantly reduce the temporary use of catheter, the duration of hospitalization, and the total medical costs for patients with stage 5 CKD. Furthermore, we clearly demonstrated that a longer (more than 1 year) MDC program for stage 5 CKD patients could slow the decline of renal function and results in annual medical cost savings.
The recommendations for the optimal timing of referral of CKD patients to nephrology services were conflicting.Citation13–17 In fact, patients with an eGFR of 30 mL/min per 1.73 m2 or less should be referred to a nephrology-based care for appropriate CKD education in order to allow adequate time (at least 3–6 months) for predialysis education.Citation18,19 This study showed that a program with a nephrologist-based MDC approach could improve clinical renal outcome and reduce medical cost, even for patients with advanced renal failure (eGFR < 15 mL/min per 1.73 m2). Our study demonstrated that most of the stage 5 CKD patients who did not receive MDC underwent incident dialysis therapy with a catheter than those of the stage 5 CKD patients who received MDC. Additionally, our analysis showed that MDC, even in cases of late referral, was associated with less temporary use of catheter, decreased need for and duration of hospital admission, and decreased initial costs of care following the commencement of dialysis.
Among stage 5 CKD patients receiving MDC, those receiving longer MDC had significantly less deterioration of renal function (0.76 ± 0.27 mL/min per 1.73 m2 per year), longer follow-up period, and delayed initiation of dialysis than the patients receiving shorter MDC. In contrast, the stage 5 CKD patients with a shorter period of MDC had lower eGFR when entering the educational program, shorter follow-up period, steeper mean eGFR decline rate, and initiation of dialysis at lower levels of renal function, as documented by predicted eGFR < 5 mL/min per 1.73 m2. There were significant differences between the two groups with respect to Hb, albumin, and gender. Despite the better improvement of anemia and nutritional status in the longer MDC group, the levels were still below the standards suggested by the National Kidney Foundation Kidney Disease Outcome Quality Initiative (NKF KDOQI) guidelines. There were more males in shorter MDC group than the longer group. A recent study by Stengel stated that the mean MDRD eGFR decline rate was steeper in men than in women among the elderly patients with CKD (1.75 vs. 1.41 mL/min per 1.73 m2 per year).Citation20 Although this result was consistent with our findings, caution must be exercised in extrapolating these results to patients with advanced CKD.
The health services cost of hemodialysis delivered differed by country and the cost of the hemodialysis session was likely to vary between accounting methods.Citation21 In Taiwan, the BNHI adopted a capitation policy in July 1996, in which the reimbursement was approximately NTD 4100 per dialysis session. The reimbursement rate was fixed and included the medication, monthly laboratory tests, erythropoietin, overhead cost, cost for all supplies, renal anemia-related blood transfusion, nursing, and physician fee. A CKD care program (preESRD care program) was also launched by the Bureau of Health Promotion in 2002 in Taiwan. According to the National Kidney Foundation Kidney Disease Outcomes Quality Initiative guidelines and literature,Citation22–24 the mean rate of decline of GRF was highly variable for various causes of kidney disease, ranging from 2 mL/min per 1.73 m2 per year to 10.4 mL/min per 1.73 m2 per year, in patients with stage 5 CKD (assuming a serum creatinine level of 5 mg/dL for eGFR of 15 mL/min per 1.73 m2). In 2008, a Taiwan Society of Nephrology committee proposed a mean rate of decline in renal function (eGFR = 8 mL/min per 1.73 m2 per year and the calculated slope was −0.66) as the quality of care incentives for patients with stage 5 CKD in this integrated preESRD care program (). The nephrologist declared the fine quality of care incentives for annual rates of decline in eGFR of <8 mL/min per 1.73 m2 per year. Hence, assuming that the renal function of patients with stage 5 CKD entering the study is the same (eGFR = 10 mL/min per 1.73 m2), the time required before dialysis (i.e., eGFR = 5 mL/min per 1.73 m2) is 3.14 months in the group with shorter CKD educational intervention, 7.57 months according to the decline rate estimated by the Taiwan Society of Nephrology, and 83.3 months in the group with longer CKD educational intervention (). Therefore, the per capita medical cost savings resulting from longer CKD education were estimated for the cases with a delay in the initiation of hemodialysis. The group with longer MDC had an annual medical cost savings of approximately NTD 336,500.66 [(83.33 − 7.57) × 13 × 4100 ÷ 12], compared with the cost of medical care incurred by the Taiwan Society of Nephrology.
The most common cause of ESRD is diabetic nephropathy.Citation25 In our study, although the stage 5 CKD patients with diabetes received MDC when their renal function was better than those of the stage 5 CKD patients without diabetes, we found that the diabetic group had a steeper rate of decline in mean eGFR, with a shorter follow-up period than that of the non-diabetic group. Importantly, differences in age, gender, and follow-up eGFR during the observation period were not statistically significant between the two groups. Our data showed that stage 5 CKD patients with diabetes, even under MDC program, had poor renal outcome compared with those without diabetes. These educational interventions should start as early as possible in the continuum of CKD care for CKD patients with diabetes ().
Overall, our findings demonstrated that MDC was cost-effective for stage 5 CKD patients who starting dialysis. By comparison, the cost of starting dialysis and continuing the hospitalization care were driven not primarily by the temporary use of catheter but by the high total cost of hospitalization care. Importantly, our analysis showed that stage 5 CKD patients who received longer MDC had a relatively flat slope of mean eGFR decline that averaged 83.3 months, well over 6 years, before commencing dialysis. We believed that this flat slope delayed the initiation of dialysis and delivered annual medical cost savings with a more cost-effective treatment, MDC programs. In addition, the stage 5 CKD patients with diabetes had a steeper decline rate of mean eGFR and commenced dialysis earlier than stage 5 CKD patients without diabetes. Developing strategies to improve the clinical renal outcome of these stage 5 CKD patients with diabetes remain an important issue for nephrologist-based MDC.
Several limitations of this study should be addressed. First, because of nonrandomization of those participating in the MDC program, there was a potential selection bias in patients who were included in this study. Second, patients’ own characteristics and unmeasured factors, such as attitude, lifestyle, or other comorbidity, which may influence MDC programs, could not be collected. Third, this study included only incident dialysis; we did not study the mortality outcomes after dialysis.
CONCLUSION
This study described the role of MDC programs in improved clinical renal outcome and medical cost savings in the stage 5 CKD patients. Certainly, the duration of patient exposure to the MDC team could be important. We believed that there was an additional value of an MDC team in optimizing clinical renal outcome and reducing medical costs in stage 5 CKD patients. Therefore, comparative value studies of cost-effective interventions may be warranted, and research needs to be undertaken to prospectively follow patients from entry into CKD educational intervention in order to confirm these findings.
ACKNOWLEDGMENT
This work was supported in part by grants (CMRPG 6A0271 to Pei-Hsien Lee) from Chang Gung Memorial Hospital, Chiayi, Taiwan.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
REFERENCES
- US Renal Data System 2012 annual data report: Atlas of chronic kidney disease and end-stage renal disease in the United States [volume 2-atlas ESRD, international comparisons]. USRDS 2012. Available at: http://www.usrds.org/atlas.aspx.Accessed October 1, 2012.
- Inaguma D, Tatematsu M, Shinjo H, Batlle D. Effect of an educational program on the predialysis period for patients with chronic renal failure. Clin Exp Nephrol. 2006;10:274–278.
- Ghossein C, Serrano A, Rammohan M, Batlle D. The role of comprehensive renal clinic in chronic kidney disease stabilization and management: the northwestern experience. Semin Nephrol. 2002;22:526–532.
- Diaz-Buxo JA. The importance of pre-ESRD education and early nephrological care in peritoneal dialysis selection and outcome. Perit Dial Int. 1998;18:363–365.
- Wu IW, Wang SY, Hsu KH, . Multidisciplinary predialysis education decreases the incidence of dialysis and reduces mortality—a controlled cohort study based on the NKF/DOQI guidelines. Nephrol Dial Transplant. 2009;24(11):3426–3433.
- Lysaght MJ. Maintenance dialysis population dynamics: current trends and long-term implications. J Am Soc Nephrol. 2002;13(Suppl. 1):S37–S40.
- Meguid El Nahas A, Bello AK. Chronic kidney disease: the global challenge. Lancet. 2005;365(9456):331–340.
- Menzin J, Lines LM, Weiner DE, . A review of the costs and cost effectiveness of interventions in chronic kidney disease: implications for policy. Pharmacoeconomics. 2011;14:1–23.
- Smith DH, Gullion CM, Nichols G, Keith DS, Brown JB, . Cost of medical care for chronic kidney disease and comorbidity among enrollees in a large HMO population. J Am Soc Nephrol. 2004;15(5):1300–1306.
- London R, Solis A, Goldberg GA, Wade S, Ryu S. Health care resource utilization and the impact of anemia management in patients with chronic kidney disease. Am J Kidney Dis. 2002;40(3):539–548.
- Robbins JD, Kim JJ, Zdon G, Chan WW, Jones J. Resource use and patient care associated with chronic kidney disease in a managed care setting. J Manag Care Pharm. 2003;9(3):238–247.
- St Peter WL, Khan SS, Ebben JP, Pereira BJ, Collins AJ, . Chronic kidney disease: the distribution of health care dollars. Kidney Int. 2004;66(1):313–321.
- Huisman RM. The deadly risk of late referral. Nephrol Dial Transplant. 2004;19:2175–2180.
- Levin A. Consequences of late referral on patient outcomes. Nephrol Dial Transplant. 2000;15(Suppl. 3):S8–S13.
- Nissenson AR, Collins AJ, Hurley J, Petersen H, Pereira BJ, Steinberg EP. Opportunities for improving the care of patients with chronic renal insufficiency: current practice patterns. J Am Soc Nephrol. 2001;12:1713–1720.
- Pereira BJ. Optimization of pre-ESRD care: the key to improved dialysis outcomes. Kidney Int. 2000;57:351–365.
- Valderrábano F, Golper T, Muirhead N, Ritz E, Levin A. Chronic kidney disease: why is current management uncoordinated and suboptimal? Nephrol Dial Transplant. 2001;16(Suppl. 7):S61–S64.
- Heatley SA. Optimal referral is early referral. Perit Dial Int. 2009;29(Suppl. 2):S128–S131.
- Luxton G. Timing of referral of chronic kidney disease patients to nephrology services (adult). Nephrology. 2010;15(Suppl. 1):S2–S11.
- Stengel B, Metzger M, Froissart M, . Epidemiology and prognostic significance of chronic kidney disease in the elderly—the Three-City prospective cohort study. Nephrol Dial Transplant. 2011;26(10):3286–3295.
- Al Saran K, Sabry A. The cost of hemodialysis in a large hemodialysis center. Saudi J Kidney Dis Transpl. 2012;23(1):78–82.
- KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Available at: http://www.kidney.org/professionals/kdoqi/guidelines_ckd/p7_risk_g13.htm. Accessed October 1, 2012.
- Hannedouche T, Albouze G, Chauveau P, Lacour B, Jungers P. Effects of blood pressure and antihypertensive treatment on progression of advanced chronic renal failure. Am J Kidney Dis. 1993;21(5 Suppl. 2):131–137.
- Hannedouche T, Chauveau P, Kalou F, Albouze G, Lacour B, Jungers P. Factors affecting progression in advanced chronic renal failure. Clin Nephrol. 1993;39:312–320.
- Schieppati A, Remuzzi G. Chronic renal disease as a public health problem: epidemiology, social, and economic implications. Kidney Int. 2005;98(Suppl.):S7–S10.