Abstract
Human parvovirus B19 (HPV B19) infection is well known as a cause of erythema infectiosum in children. Acute glomerulonephritis due to HPVB19 infection is rarely observed in adults. Here, we present the case of a 45-year-old female who showed acute glomerulonephritis induced by HPVB19 infection with various autoantibodies. She had proteinuria (175 mg/g creatinine) and hematuria (20–29 erythrocytes per high-power field) in a urinalysis, and various autoantibodies such as antinuclear antibodies, proteinase-3-antineutrophil cytoplasmic antibodies (PR3-ANCA), antiglomerular basement membrane (GBM) antibodies, and anticardiolipin antibodies in a blood examination. A renal biopsy showed that endocapillary proliferative glomerulonephritis comprised of mononuclear cell infiltration. By using immunofluorescence microscopy, IgG, IgA, IgM, C3, C4, and C1q deposits were detected mainly in glomerular capillaries. Electron-dense deposits were detected in the subendothelial area and mesangial area by using electron microscopy. All symptoms and abnormal laboratory data were self-improved. Our patient’s case may provide a clue to the etiology of ANCA-associated vasculitis or lupus nephritis.
INTRODUCTION
Endocapillary proliferative glomerulonephritis is a characteristic pathological feature of acute glomerulonephritis. Although the most common cause of acute glomerulonephritis is group A β-hemolytic streptococcus, other bacterial infections such as Staphylococcus aureus, Streptococcus viridans, viral infections, and parasitic infections often cause acute glomerulonephritis.Citation1
Human parvovirus B19 (HPVB19) infection is well known as a cause of erythema infectiosum in children. In adults, not only arthritis, arthralgia, and transient aplastic crisis but also acute glomerulonephritis are often observed following HPVB19 infection.Citation2 The pathogenesis of the erythema infectiosum and joint symptoms seems to be based on the deposition of immune complexes. As a glomerular disease, the deposition of circulating immune complexes in glomerular lesions is also a cause of disease onset,Citation3 but the direct infection of glomerular endothelial cells is assumed to be a mechanism of renal injury. Almost all of these symptoms are self-limiting, but some patients develop severe glomerulonephritis, such as antineutrophil cytoplasmic antibodies (ANCA)-associated vasculitisCitation4,5 or lupus nephritis.
We report here our patient’s case of acute glomerulonephritis due to HPVB19 infection that showed various autoantibodies. This report may provide a clue to the etiology of ANCA-associated vasculitis or lupus nephritis.
CASE
A 45-year-old Japanese female was admitted to our hospital because of oliguria, anasarca, and headache. She had a history of fever, arthralgia, and facial and pretibial edema 5 days before admission. Three days before admission, a nonsteroidal anti-inflammatory agent and a gastrointestinal agent were prescribed for her by a general practitioner. At this point, her serum creatinine level was 0.8 mg/dL. She had no children.
On examination, her blood pressure was 140/69 mmHg and the pulse rate was 75 beats/min. Her body temperature was 36.3°C. She had facial and pretibial edema. Laboratory data on admission showed that serum creatinine and blood urea nitrogen were 3.14 and 39.2 mg/dL, respectively. Hemoglobin and serum albumin were 10.9 and 3.6 g/dL, respectively. White blood cell, platelets, C-reactive protein, alanine aminotransferase, aspartate aminotransferase, lactate dehydrogenase, blood glucose, and electrolytes were all normal. Urinalysis showed proteinuria (175 mg/g creatinine) and hematuria (20–29 erythrocytes per high-power field) with granular casts (5–9 per high-power field). On immunological examination, serum immunoglobulin (Ig)G, IgA, and IgM were 1226, 145, and 163 mg/dL, respectively. Serum C3, C4, and CH50 were 49.5 mg/dL (normal range: 65–135 mg/dL), 10.4 mg/dL (normal range: 13–35 mg/dL), and less than 10 mg/dL (normal range: 29–48 mg/dL), respectively. The antinuclear antibodies titer was 160 times with a speckled pattern, and that of antistreptolysin O was 101.3 U/mL. Anti-double-stranded DNA antibodies, anti-Smith antibodies, hepatitis B virus surface antigen, and hepatitis C virus antibodies were all negative.
The patient’s myeloperoxidase-ANCA (MPO-ANCA), proteinase-3-ANCA (PR3-ANCA), and antiglomerular basal membrane (GBM) antibodies were 1.6 U/mL (normal range: <9 U/mL), 5.1 U/mL (normal range: <3.5 U/mL), and 15 EU (normal range: <10 EU), respectively. Anticardiolipin antibodies were 13.3 U/mL (normal range: <10 U/mL). IgM antibodies titers to HPVB19 were elevated at 13.83 (normal range: <0.8). Taken together, the patient’s antinuclear antibodies, PR3-ANCA, anti-GBM antibodies, anticardiolipin antibodies, and HPVB19-specific IgM antibodies were positive. In light of these results, we conducted a percutaneous renal biopsy to investigate the reasons for the patient’s acute renal failure.
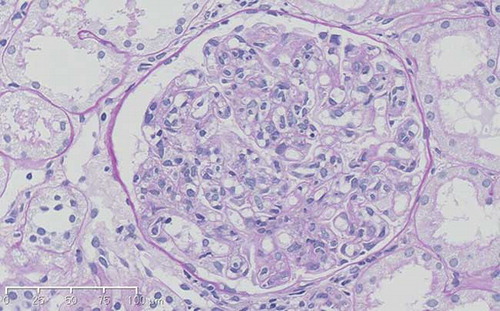
One needle biopsy core including nine glomeruli was submitted. One glomerular collapse was observed, and the other glomeruli were all enlarged and hypercellular; that is, indicative of endocapillary proliferative glomerulonephritis (). The main infiltration cells were mononuclear cells, and there were no neutrophils in the glomeruli. The impairment of interstitium and vessels was mild. Using immunofluorescence microscopy, IgG, IgA, IgM, C3, C4, and C1q deposits were detected in glomerular capillaries. The electron-dense deposits were detected in the subendothelial area and mesangial area, but not in the subepithelial area, by using electron microscopy (). Based on the renal biopsy results and the high titer of HPVB19-specific IgM antibodies, this patient was diagnosed as having acute glomerulonephritis due to HPVB19 infection. All symptoms and abnormal laboratory data improved gradually with no medication during admission, and she was discharged 10 days after the renal biopsy.
DISCUSSION
Although a relationship between HPVB19 infection and glomerulonephritis (such as endocapillary proliferative glomerulonephritis,Citation2,6–8 mesangioproliferative glomerulonephritisCitation9 and focal segmental glomerulosclerosisCitation10,11) has been reported by many investigators, no specific pathological features of renal disease with HPVB19 have been reported to the best of our knowledge. The first report of a link between HPVB19 infection and glomerulonephritis was that of two siblings with sickle cell disease and hypoplastic crisis after HPVB19 infection;Citation12 their pathological findings indicated focal segmental glomerulonephritis. Wierenga et al.Citation10 also described HPVB19-infected patients with sickle cell disease; proliferative glomerulonephritis and focal segmental glomerulonephritis were observed in these patients.
In adult patients without hemolytic disease, endocapillary proliferative glomerulonephritis seems to be a common pathological feature of HPVB19 infection-related renal disease (). Other clinical features that are often observed in patients with endocapillary proliferative glomerulonephritis due to HPVB19 infection are acute nephritic syndrome, hypocomplementemia, and self-limiting recovery.
Table 1. The characteristics of patients with endocapillary proliferative glomerulonephritis induced by HPVB19 infection.
Although our patient also showed the same manifestations as those in the previous reports, many of her autoantibody productions were distinctly different from those in the previous reports (). On admission, we considered the presence of lupus nephritis, ANCA-associated vasculitis or poststreptococcal acute glomerulonephritis in our patient because various autoantibodies, that is, antinuclear antibodies, PR3-ANCA, anti-GBM antibodies, and anticardiolipin antibodies were detected by blood examination, and we observed hypertension, acute renal failure, and hypocomplementemia. However, the titers of ANCA, anti-GBM antibodies, and anticardiolipin antibodies were low, while the titer of anti-parvovirus antibodies was high and anti-ds-DNA antibodies were absent. On renal biopsy, although the full-house pattern of immunofluorescence is consistent for lupus nephritis, this immunofluorescence feature is not characteristic of ANCA-associated vasculitis and poststreptococcal acute glomerulonephritis. Furthermore, the absence of subepithelial electron-dense deposits and tubuloreticular inclusions is not consistent with poststreptococcal acute glomerulonephritis or lupus nephritis. Based on these results, the presence of lupus nephritis, ANCA-associated vasculitis, and poststreptococcal acute glomerulonephritis was denied.
Our case differs from previous reports that showed endocapillary proliferative glomerulonephritis with HPVB19 infection. Hermann et al.Citation4 demonstrated that of six patients diagnosed with acute HPVB19 infection, one patient was tested positive for PR3-ANCA and two were tested positive for PR3-ANCA and MPO-ANCA. In addition, Hermann et al. observed that after 6 months of follow-up, all of the patients with raised ANCA at baseline were tested negative, and their peripheral joint disease and macular rush had subsided.
Although there are some studies about the relationship between HPVB19 infection and the detection of ANCA,Citation4,5 reports of a direct relationship between ANCA and renal lesions or renal vasculitis caused by ANCA are rare. A direct invasion of HPVB19 to vascular endothelial cells that present P-antigen may be a cause of vasculitis associated with HPVB19 infection. However, the precise relationship between ANCA-associated nephritis and HPVB19 infection remains unknown.
Although a lupus-like presentation in several patients with HPVB19 infection was reported, almost all of these cases were self-limiting and renal manifestation was absent.Citation16 Sève et al.Citation17 conducted a computer-assisted search of publications related to systemic lupus erythematosus (SLE) associated with HPVB19 infection dated from 1975 to 2003 and found that 19 out of 38 patients showed self-limited lupus-like symptoms, and none had renal involvement. Saeki et al.Citation18 also reported a case mimicking SLE caused by HPVB19 infection, and their patient had no urinary abnormality.
To our knowledge, there are few reports about the relationship between HPVB19 infection and lupus nephritis. Although our patient showed self-limited lupus-like symptoms including arthralgia, antinuclear antibodies, and immunologic disorder (anticardiolipin antibodies), the presence of renal disorder was different from Sève’s and Saeki’s reports. Sugimoto et al.Citation19 noted that renal manifestation might not be rare in patients with SLE-like presentations of HPVB19 infection, but they did not provide the pathological findings of their patient. The most conspicuous manifestations in our patient compared to the previous reports are the endocapillary glomerulonephritis after HPVB19 infection that showed SLE-like clinical manifestations and the laboratory data.
The mechanism of autoantibody production due to HPVB19 infection is not clear. In general, molecular mimicry seems to be one reason for viral-induced autoantigen production.Citation20 Park et al.Citation21 have demonstrated that Th1-associated cytokines play a crucial role in the pathogenesis and development of SLE after HPVB19 infection. Hession et al.Citation22 contend that the relative antinuclear antibody titers may be a prognostic indicator as to which patients will develop chronic HPVB19-induced SLE, as opposed to mere transient symptoms.
In conclusion, the possibility of HPVB19 infection should be considered when glomerulonephritis accompanied by the production of autoantibodies is encountered, and the further accumulation of case reports similar to the present case will provide clues to elucidate the pathogenic mechanisms of ANCA-associated vasculitis or lupus nephritis.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
REFERENCES
- Bernardo RI. Acute endocapillary glomerulonephritis. In: Davison AM, Cameron JS, Grunfeld JP, Kerr DN, Ritz E, Winearls CG, eds. Oxford Textbook of Clinical Nephrology. Oxford: Oxford University Press; 1998:545–557.
- Nakazawa T, Tomosugi N, Sakamoto K, . Acute glomerulonephritis after human parvovirus B19 infection. Am J Kidney Dis. 2000;35:E31.
- Watanabe T. Renal involvement in human parvovirus B19 infection. Pediatr Nephrol. 2003;18:996–997.
- Hermann J, Denel U, Stunzner D, Daghofer E, Tilz G, Graninger W. Clinical interpretation of antineutrophil cytoplasmic antibodies: parvovirus B19 infection as a pitfall. Ann Rheum Dis. 2005;64:641–643.
- Chou TN, Hsu TC, Chen RM, Lin LI, Tsay GJ. Parvovirus B19 infection associated with the production of anti-neutrophil cytoplasmic antibody (ANCA) and anticardiolipin antibody (aCL). Lupus. 2000;9:551–554.
- Abeygunasekara SC, Peat D, Ross CN. Endocapillary glomerulonephritis secondary to human parvovirus B19 presenting with nephrotic syndrome: a report of two cases and a review of the literature. Ren Fail. 2010;32:880–883.
- Komatsuda A, Ohtani H, Nimura T, . Endocapillary proliferative glomerulonephritis in a patient with parvovirus B19 infection. Am J Kid Dis. 2000;36:851–854.
- Takeda S, Takaeda C, Takazakura E, Haratake J. Renal involvement induced by human parvovirus B19 infection. Nephron. 2001;89:280–285.
- Ongure P, Dede F, Bodur H, . Glomerulonephritis associating parvovirus B19 infection. Ren Fail. 2006;28:85–88.
- Wierenga KJ, Pattison JR, Brink N, . Glomerulonephritis after human parvovirus B19 in an immunocompetent host. Lancet. 1995;346:475–476.
- Tolaymat A, Al Mousily F, MacWilliam K, Lammert N, Freeman B. Parvovirus glomerulonephritis in a patient with sickle cell disease. Pediatr Nephrol. 1999;13:237–238.
- Markenson AL, Chandra M, Lewy JE, Miler DR. Sickle cell anemia, the nephrotic syndrome and hypoplastic crisis in a sibship. Am J Med. 1978;64:719–723.
- Mori Y, Yamashita H, Umeda Y, . Association of parvovirus B19 infection with acute glomerulonephritis in healthy adults: case report and review of the literature. Clin Nephrol. 2002;57:69–73.
- Iwafuchi Y, Morita T, Kamimura A, Kunisada K, Ito K, Miyazaki S. Acute endocapillary proliferative glomerulonephritis associated with human parvovirus B19 infection. Clin Nephrol. 2002;57:246–250.
- Ieiri N, Hotta O, Taguma Y. Characteristics of acute glomerulonephritis associated with human parvovirus B19 infection. Clin Nephrol. 2005;64:249–257.
- Tovari E, Mezey I, Hedman K, Czirjak L. Self limiting lupus-like symptoms in patients with parvovirus B 19 infection. Ann Rheum Dis. 2002;61:662–663.
- Sève P, Ferry T, Koenig M, Cathebras P, Rousset H, Broussolle C. Lupus-like presentation of parvovirus B19 infection. Semin Arthritis Rheum. 2005;34:642–648.
- Saeki T, Shibuya M, Sawada H, . Human parvovirus B19 infection mimicking systemic lupus erythematosus. Mod Rheumatol. 2001;11:308–313.
- Sugimoto T, Tsuda A, Uzu T, Kashiwagi A. Emerging lupus-like manifestations in acute parvovirus B19 infection. Clin Rheumatol. 2008;27:119–120.
- Barnett LA, Fujinami RS. Molecular mimicry: a mechanism for autoimmune injury. FASEB J. 1992;6:840–844.
- Park SJ, Kim JH, Ha TS, Shin JI. Association of parvovirus B19 infection with systemic lupus erythematosus: role of Th1 predominance. J Rheumatol. 2011;38:1221.
- Hession MT, Au SC, Gottlieb AB. Parvovirus B19-associated systemic lupus erythematosus: clinical mimicry or autoimmune induction? J Rheumatol. 2010;37:2430–2432.