Abstract
Coexistence of nephrotic syndrome and neoplasm is rarely observed in children. We report the diagnostic and therapeutic problems of a 16-year-old female with nephrotic syndrome, ovarian tumor, and increased levels of tumor markers. She was suspected to have paraneoplastic nephrotic syndrome. After ovarian tumor resection, the nephrotic syndrome remission was not observed, while increased tumor marker levels were noted. The patient’s final diagnosis was nephrotic syndrome in the course of primary mesangial proliferative glomerulonephritis. In conclusion, nephrotic syndrome in a patient with neoplasia might occur in the course of the primary and nonparaneoplastic glomerulopathy. Elevated serum tumor markers in patients with nephrotic syndrome might be nonspecific because of the stimulation of their production by peritoneal mesothelium, due to transudation to body cavities, that is, ascites.
INTRODUCTION
Coexistence of nephrotic syndrome (NS) and neoplasm is rarely observed in children.Citation1 In differential diagnosis of NS, paraneoplastic nephrotic syndrome (PNS) is considered in the case of coincidence of typical symptoms of NS and increased levels of tumor markers in body fluids. The diagnostic criteria of paraneoplastic glomerulopathy include clinical and histological remission of NS after tumor resection or after chemotherapy, renal relapse associated with recurrence of the neoplasia, and statement of pathophysiological connection between the two diseases.Citation1,Citation2 The causal association between cancer and PNS is suggested when nephrotic proteinuria appears 6 months before or after the diagnosis of cancer.
A 16-year-old female presented a diagnostic dilemma. She was suspected to have PNS; however, her final diagnosis was NS in the course of primary mesangial proliferative glomerulonephritis and mature ovarian teratoma.
CASE REPORT
A 16-year-old female was admitted to the hospital due to deterioration of general condition, abdominal distension, ankle edema, and swollen eyelids. Her past medical history was unremarkable. The family history was also insignificant. The patient’s physical development was normal. Her height and weight were 167 cm (75th percentile) and 60 kg (75th percentile), respectively. The patient had Tanner stage 5 pubertal characteristics and typical menstruation. Laboratory results showed the following: serum albumin 2.2 g/dL, cholesterol 390 mg/dL, C-reactive protein 0.19 mg/L, creatinine 0.65 mg/dL, and daily proteinuria 5.07 g; serum urea, electrolytes, blood count, and urine sedimentation were normal. Serum complement concentration (C3,C4), antinuclear antibody titer, and neutrophil cytoplasmic antibody titer were within the normal range. Urine culture was negative. The abdominal ultrasound revealed normal kidneys and the right ovarian cyst. Steroid therapy (prednisone 60 mg/day) was initiated. Additionally, symptomatic treatment was instituted, including diuretics (spironolactone and hydrochlorothiazide), proton pump inhibitor, and calcium carbonate. The patient was maintained on oral steroid therapy (60 mg/day). The NS partial remission was achieved within 16 days as manifested by selected lab test results: serum albumin 2.9 g/dL, protein 5.1 g/dL, cholesterol 260 mg/dL, and 24-h urine protein 0.3 g. Eighteen days after admission, the patient was discharged from the hospital but reported diarrhea and deterioration of her general condition at home. After 1 week, the patient was readmitted with minor edema of eyelids and lower extremities. Laboratory results revealed the following: serum albumin 2.3 g/dL, protein 4.6 g/dL, cholesterol 548 mg/dL, and 24-h urine protein 2.55 g. Despite medical treatment with oral prednisone (60 mg/day) and pulses of methylprednisolone (i.v. 0.5 g/dose daily for 3 days), the clinical condition of the patient deteriorated. General edema, ascites, and increase of proteinuria were noted. Abdominal/pelvic ultrasound revealed cystic structure with a piecewise thickened wall identified as an ovarian tumor. Serum CA-125 level was 69 U/mL (normal value: 0–35 U/mL).
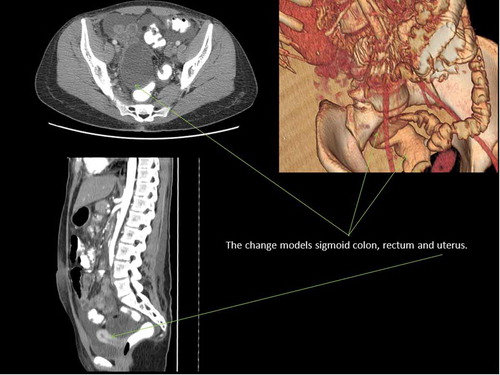
The patient was transferred to the surgical clinic, where computed tomography (CT) of the abdomen and pelvis was carried out. Abdominal CT scan revealed the presence of significant amounts of free fluid in the abdominal cavity and pelvis. The cystic structure with thin, reinforced coronary band and the lateral dimensions of approximately 7.5 × 6.1 cm (cc size of about 6 cm) was localized in the area of right ovarian adnexa. The cystic structure was hypodense and contained small inclusions of calcifications and fat on the left margin. On the front margin, the pathological lesion was visible (up to 0.6 cm), which might be the residual ovary. The tumor modeled rectum, sigmoid colon, and uterus, without obvious features of invasion (). CT scan results suggested the presence of teratoma originating probably from the right ovary.
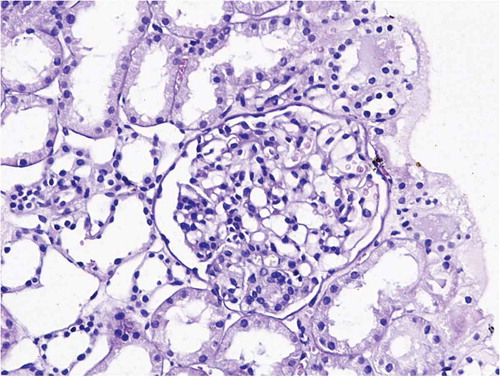
Figure 2. Result of kidney biopsy: mesangial proliferative glomerulonephritis (prof. Agnieszka Hałon, Department of Pathomorphology, Wroclaw Medical University, Poland).
The patient underwent surgery. The right ovary with the tumor and a small scrap of the right fallopian tube cyst were removed. A small part of the left ovary was taken for analysis with normal result. Histopathological examination of the tumor: maturum teratoma.
After ovarian tumor resection, NS remission was not observed. Furthermore, edema increased. Laboratory results showed the following: serum CA-125 173–200 U/mL, CA-19-9 88.97–100 U/mL (normal value 0–37 U/mL), serum albumin 1.6 g/dL, protein 4.1 g/dL, cholesterol 742 mg/dL, urea 114 mg/dL, creatinine 1.12 mg/dL, and 24-h urine protein 14.5 g. Intensive diuresis therapy was necessary. The patient was consulted by hematology, oncology, and gynecology.
During subsequent abdominal and pelvic CT, focal changes were not identified. However, the thickened peritoneum and fluid in the peritoneal cavity were observed. Because of the high suspicion of metastasis to peritoneum, nuclear magnetic resonance (NMR) was carried out, which showed no abnormalities. The values of tumor markers were variable. A kidney biopsy was performed, and chronic mesangial proliferative glomerulonephritis (MPGN) was diagnosed (). Immunofluorescence microscopy was negative. Cyclosporine A (CsA) therapy was started (200 mg/day) with gradual reduction in glucocorticoid dose. We observed regression of proteinuria, the improvement in serum biochemical parameters typical for NS, and normalization of serum CA-125 and CA-19-9 levels. Genetic analysis showed no mutation in WT1 gene. The girl was discharged home in good condition. She remains under the control of our department. The time of follow-up after resection of the right ovarian tumor is 8 months and from obtaining complete remission is 5 months. The patient’s general condition is very good. The results of blood and urine tests and abdominal ultrasound are normal. Current treatment: CsA 200 mg/day, prednisone 5 mg/48 h.
DISCUSSION
NS in children appears mostly in the course of primary glomerulonephritis. Initially, the clinical picture of the disease in our patient did not allow us to conclude any primary or secondary character of glomerulopathy. The lack of systemic symptoms and good response to glucocorticosteroid therapy initially suggested NS in the course of primary glomerulopathy. On the other hand, the return of symptoms typical for NS, secondary resistance to steroids, diagnosis of the right ovarian tumor, and an increase of CA-125 in serum suggested paraneoplastic glomerulopathy.
Changes in the right ovary, followed by the surgical resection, caused a delay in obtaining renal biopsy, especially in view of unclear oncological picture (suspicion of the metastasis to peritoneum, the increase in serum CA-125 and CA-19-9 levels).
Before the resection of the abnormal right ovary and histopathological diagnosis, the type of the ovarian tumor was not obvious. The patient’s age and the regular contours of the tumor suggested its benign character. However, the presence of solid structures within the tumor and ascites were typical for the malignant neoplasm. Ovarian tumors represent 1% of all childhood cancers, and mature teratoma is the most common cancer among the teenagers.Citation2 The benign teratomas are associated with different paraneoplastic syndromes. Thus far only one case of PNS in the course of teratoma has been reported.Citation3 In a 7-year-old girl treated for NS without complete remission, an abdominal tumor was revealed after 9 months of therapy. It was resected and histopathologically recognized as a benign teratoma. The intraoperative kidney biopsy showed membranous glomerulonephritis (MNGN). Ten days after the surgery, significant decrease of proteinuria was observed and then full remission of NS.
It is not known how often the secondary glomerulopathies in the course of neoplasms appear. However, it is known that they occur less often in children than in adults. They were described mostly in the patients with lymphogranulomatosis maligna and Hodgkin lymphoma, rhabdomyosarcoma, leukemia, and lately in the girl with Sertoli–Leydig ovarian tumor.3–Citation6 The glomerular lesions revealed by renal biopsy were in 70% of cases typical for MNGN and in other 30% of cases for submicroscopic glomerulonephritis and focal segmental glomerulosclerosis. However, mesangial proliferation (which was recognized in a kidney biopsy of our patient) has never been described as a secondary glomerulonephritis in the course of neoplastic disease. Remission of PNS was described at various times after the resection of tumors in children, from 3 to 11 months, which is connected with immunological dysregulation in the course of neoplastic disease.Citation1
In the described patient, the increase of tumor markers in serum was observed. The whole clinical picture indicates its nonspecific character. In children, due to the domination of primary glomerulonephritis, the tumor markers in serum are rarely tested in the course of the disease. In our patient, the tests were conducted due to the presence of the ovarian tumor shown on pelvic ultrasound examination. Interpretation of increased serum CA-125 level was difficult as CA-125 might be produced by normal epithelia not only by the ovarian cancer cells. Ascites itself can induce elevation in serum CA-125 level, as well as CA 19–9.Citation7–Citation9
The lack of NS remission and worsening of the patient’s condition after the removal of the ovarian tumor, coupled with a very good therapeutic response to CsA as well as the type of glomerulonephritis, suggests the primary glomerulopathy. In our case, the elevated tumor markers might be nonspecific because of the stimulation of their production by mesothelium of peritoneum due to transudation to body cavities, that is, ascites.
It must be stressed that the time of follow-up in our patient is relatively short, thus the interpretation of the reported case must be rather careful. Currently we are paying attention to the necessity of considering neoplastic disease as differential diagnosis in adolescents with NS. On the other hand, the disorders typical for NS such as ascites, pleural, and pericardial effusions might lead to nonspecific shifts in serum (elevation of tumor markers).
CONCLUSIONS
While interpreting the elevation of CA-125 and CA19-9 in the serum of NS patient, one must take into consideration the increased production of these glycoproteins by the mesothelial cells stimulated by the liquid in an abdominal cavity. NS in a patient with neoplasia might occur in the course of the primary and nonparaneoplastic glomerulopathy.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Bacchetta J, Juillard L, Cochat P, Droz JP. Paraneoplastic glomerular diseases and malignancies. Crit Rev Oncol Hematol. 2009;70:39–58.
- Wągrowska-Danilewicz M, Danilewicz M. Nephrotic syndrome and neoplasia: our experience and review of the literature. Pol J Pathol. 2011;62:12–18.
- Beauvais P, Vaudour G, Boccon Gibod LMembranous nephropathy associated with ovarian tumour in a young girl: recovery after removal. Eur J Pediatr. 1989;148:624–625.
- Chen A, Vander Lugt M, McAllister-Lucas LMAn unusual case of membranous nephropathy associated with an ovarian tumor. Pediatr Nephrol. 2011;26:2249–2251.
- Farruggia P, Trizzino A, Maringhini SHodgkin lymphoma and nephrotic syndrome in childhood. Indian J Pediatr. 2010;77:1147–1149.
- Olowu WA, Salako AA, Adelusola KAFocal segmental glomerulosclerosis and nephrotic syndrome in a child with embryonal rhabdomyosarcoma. Clin Exp Nephrol. 2008;12: 144–148.
- Basaran A, Zafer Tuncer S. Ascites is the primary cause of cancer antigen-125 (CA-125) elevation in systemic lupus erythematosus (SLE) patients with nephrotic syndrome. Med Hypotheses. 2007;68:197–201.
- Bokhari A, Rosenfeld GS, Cracchiolo BCystic struma ovarii presenting with ascites and an elevated CA-125 level. A case report. J Reprod Med. 2003;48:52–56.
- Mui MP, Tam KF, Tam FKCoexistence of struma ovarii with marked ascites and elevated CA-125 levels: case report and literature review. Arch Gynecol Obstet. 2009;279:753–757.