Abstract
Background and aims: Hypercytokinemia is believed to be harmful and reducing cytokine levels is considered beneficial. Extracorporeal blood purification (EBP) techniques have been studied for the purpose of cytokine reduction. We aimed to study the efficacy of various EBP techniques for cytokine removal as defined by technical measures. Method: We conducted a systematic search for human clinical trials which focused on technical measures of cytokine removal by EBP techniques. We identified 41 articles and analyzed cytokine removal according to clearance (CL), sieving coefficient (SC), ultrafiltrate (UF) concentration and percentage removed. Results: We identified the following techniques for cytokine removal: standard hemofiltration, high volume hemofiltration (HVHF), high cut-off (HCO) hemofiltration, plasma filtration techniques, and adsorption techniques, ultrafiltration (UF) techniques relating to cardiopulmonary bypass (CPB), extracorporeal liver support systems and hybrid techniques including combined plasma filtration adsorption. Standard filtration techniques and UF techniques during CPB were generally poor at removing cytokines (median CL for interleukin 6 [IL-6]: 1.09 mL/min, TNF-alpha 0.74 mL/min). High cut-off techniques consistently offered moderate cytokine removal (median CL for IL-6: 26.5 mL/min, interleukin 1 receptor antagonist [IL-1RA]: 40.2 mL/min). Plasma filtration and extracorporeal liver support appear promising but data are few. Only one paper studied combined plasma filtration and adsorption and found low rates of removal. The clinical significance of the cytokine removal achieved with more efficacious techniques is unknown. Conclusion: Human clinical trials indicate that high cut-off hemofiltration techniques, and perhaps plasma filtration and extracorporeal liver support techniques are likely more efficient in removing cytokines than standard techniques.
Introduction
Multiorgan dysfunction syndrome (MODS) results in high mortality despite advances in intensive care.Citation1,Citation2 Variations in etiology, whether induced by microbials or tissue injury, often result in a similar pattern of deterioration.Citation3 The stimulus for cytokine activation occurs through both pathogen-associated molecular patterns (PAMPS) or damage-associated molecular patterns (DAMPS) initiating common pathways which will ultimately lead to hypercytokinemia.Citation4
Although cytokines play a role in limiting damage and helping the process of wound healing, the excessive presence of cytokines in the circulation is believed to be harmful. Thus, reducing its level to a more homeostatic range is believed to improve outcome.Citation5,Citation6 The use of cytokine antibodies to counteract hypercytokinemia has been found ineffective, and even harmful in critically ill patients.Citation7,Citation8 Another potential approach is the use of extracorporeal techniques for the purpose of cytokine removal.Citation9--Citation11 Cytokines are water soluble middle molecules (molecular weight 0.5–60 kDa), which exist in free form in the circulation. These characteristics make them suitable targets for removal by extracorporeal blood purification (EBP) techniques, yet no systematic analysis has been performed to understand which technique and which filtration devices achieve the highest level of efficiency of cytokine removal in critically ill patients.
Methods
We conducted a systematic search using Pubmed database up to November 2012, for relevant articles on human studies on cytokine removal using known modalities of EBP. We then systematically assessed the efficacy of all EBP techniques previously reported in the literature using these data.
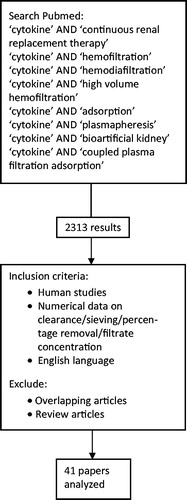
Our approach at identifying relevant articles for analysis is outlined in .
The following search terms were used: “cytokine” AND “continuous renal replacement therapy”; “cytokine” AND “hemofiltration”; “cytokine” AND “hemodiafiltration”; “cytokine” AND “high volume hemofiltration”; “cytokine” AND “adsorption”; “cytokine” AND “plasmapheresis”; “cytokine” AND “bioartificial kidney” and “cytokine” AND “coupled plasma filtration adsorption.” All the terms used were MESH terms except for “continuous,” “bioartificial kidney,” “high volume hemofiltration” and “coupled plasma filtration adsorption” which are keyword searches.
Abstracts of articles retrieved were then screened for two inclusion criteria: human experimental studies and the reporting of a numerical value of at least one of these measures of cytokine removal: clearance, sieving, percentage removal or concentration in the filtrate. Two independent researchers performed the search and then manually screened retrieved articles for those which met both inclusion criteria. Abstracts which did not include enough details as well as publications with no abstracts provided were traced using library resources and each paper screened for inclusion criteria. We excluded review articles and articles published in language other than English.
We used four main ways of expressing cytokine removal: clearance (CL), sieving coefficient (SC), ultrafiltrate (UF) concentration and percentage removed. As this review is concerned with technical aspects of cytokine removal and not patient outcome, we did not focus on survival or other clinical outcomes.
In terms of definitions, we used the term “standard technique” to refer to the use of standard high flux hemofilters (nominal cut-off point of 30–40 kDa) at standard doses of filtrate flow (<25 mL/kg/h), while the term “high cut off techniques” was used to refer to the use of super high flux hemofilters with a nominal cut-off point of greater than 60 kDa.Citation11 The term “high volume hemofiltration” (HVHF) was used to refer to techniques of hemofiltration using standard hemofilters at doses higher than 50 mL/kg/h. HVHF using standard filters was labeled as Std/HVHF and classified under standard hemofiltration. The term “plasma filtration” was used to refer to techniques involving the passing of blood through a large pore plasma filter that resulted in filtration of plasma, where this filtered plasma was discarded and replaced by another source of colloid/plasma. The term liver extracorporeal support was used to refer to the use of devices in liver failure for the purpose of blood purification where blood was dialyzed across an albumin-impermeable membrane (MARS) or where plasma separation was followed by adsorption (Prometheus). The term “Adsorption techniques” included all techniques where either whole blood or plasma was exposed to a sorbent. The term “Combined plasma filtration adsorption” (CPFA) was used to refer to techniques where there was initial plasma separation followed by the filtrate being exposed to an adsorption device. The term CPFA was also used to refer to a technique in which the proposed mechanism was filtration or diafiltration using a filter that offered a degree of cytokine adsorption. A few techniques relating to cytokine removal during cardiopulmonary bypass were identified; conventional ultrafiltration (CUF) which referred to ultrafiltration performed during the rewarming phase, modified ultrafiltration (MUF) which referred to ultrafiltration after separation from bypass and zero balanced ultrafiltration (ZBUF) which referred to ultrafiltration commenced after 15 min of CPB. Other techniques were labelled as “UF in bypass” with a description of how the technique was performed.
Data which were reported only in the form of graphs or figures had their numerical values estimated from the details given in the graphs. When more than one measurement was available, an average value was calculated. Where both UF concentration and plasma concentration are provided for the same time period, SC was taken as the fraction of UF over plasma concentration. CL was then calculated as the product of SC and ultrafiltration rate. The information on CL, SC and percentage removed was analyzed to seek out techniques that offered the highest rate of cytokine removal based on human studies. Where sufficient data were available, these techniques were then analyzed for operating characteristics which appeared to offer the best rate of cytokine removal.
Due to the limited amount of data, we only calculated medians and interquartile ranges for cytokines of which three of more values had been identified. We did not make any statistical comparisons due to the limited number of observations and the variation in operational characteristics.
Results
The data extraction process is summarized in .
We identified the following main approaches: standard hemofiltration, high volume hemofiltration (HVHF), high cut-off (HCO) hemofiltration, plasma filtration techniques, adsorption techniques, ultrafiltration (UF) techniques relating to cardiopulmonary bypass (CPB), extracorporeal liver support systems and hybrid techniques, for example combined plasma filtration and adsorption (CPFA). The number of papers studying a particular technique as well as the total number of patients who were studied according to each technique is shown in . Many articles studied more than one technique and also measured the levels of multiple cytokines. A few papers reported on hybrid therapies such as combined plasma filtration adsorption,Citation32 adsorption combined with standard hemodiafiltrationCitation14 and plasma filtration combined with standard hemodiafiltration.Citation47
Table 1. Number of papers and total number of patients studied for each technique.
Standard techniques include both hemofiltration using standard filters at standard dosesCitation13,Citation17,Citation18,Citation20,Citation22,Citation23,Citation35,Citation39–Citation41,Citation43,Citation49,Citation51 as well as hemofiltration at high volume dosesCitation19,Citation49 according to current definitions; with the latter labeled as HVHF. Standard or high cut-off techniques included continuous hemofiltration,Citation13,Citation15–Citation18,Citation20,Citation22,Citation23,Citation35,Citation39–Citation41,Citation43,Citation49,Citation51 continuous hemodialysisCitation15,Citation18,Citation27,Citation45 and continuous hemodiafiltration.Citation21,Citation24–Citation26,Citation36
The main cytokines measured in the clinical studies were interleukin-1b (IL-1b), interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10), tumor necrosis factor-alpha (TNF-alpha) and interleukin-1 receptor antagonist (IL-1Ra) Other cytokines measured were interleukin-2 (IL-2), interleukin-2 receptor (IL-2R), interleukin-6 receptor (IL-6R) and soluble TNF-alpha receptors I and II (sTNFαRI and sTNFαRII). One paperCitation52 studied many other cytokines and details are included in the footnote of . Two of the high cut-off studies and a plasma filtration study also included data on albumin loss.Citation15,Citation16,Citation42
and show data on clearance (CL) and sieving coefficient (SC) extracted from human studies respectively. The percentage removed data shown in . The number of patients that contributed data to each measurement is shown for each technique and treatment characteristics. shows a list of all devices studied including other relevant details when reported.
Table 2. Clearance (CL) data according to techniques, devices and treatment characteristics.
Table 2.1. Summary of CL values for Std/CVVH and HCO/CVVH.
Table 3. Sieving coefficient (SC) data for different techniques and devices with specific treatment characteristics.
Table 4. Percentage removal data for different cytokines.
Table 5. Device codes.
The standard techniques achieved low clearance, for all cytokines measured even when combined with high volume hemofiltration. Std/HF techniques also had overall poor SC for various cytokines, mostly in the range of less than 0.1 to 0.2 regardless of operating characteristics. Some exceptions include IL-8, IL-1β and IL-1Ra although the ranges were very wide with some studies finding very poor SC. The percentage removed data shown in demonstrated that removal of cytokine was poor for standard techniques even when combined with high volume hemofiltration.
HCO techniques were more consistent in offering moderate to high degree of cytokine clearance, for all cytokines measured. For illustration, the median value of CL for IL-6 using standard HF (Std/HF) was 1.09 mL/min while the corresponding median value of CL for IL-6 for HCO technique (HCO/HF) was 26.5 mL/min (refer ). CL using HCO techniques seemed to improve with increasing UF flows from 1 L/h to 2.5 L/h. HCO with continuous hemofiltration (HCO/HF) was comparable to continuous hemodialysis (HCO/HD) in terms of cytokine removal, however albumin loss was significantly different between these two modes (more than doubled with HF) when UF flows are increased from 1 L/h to 2.5 L/h. HCO techniques consistently showed high SC of close to unity for IL-6 and IL-1Ra. Albumin SC for HCO techniques was reported in one paper and found to be 0.026.Citation16 Among the cytokines studied, the SC for TNF-alpha using HCO techniques appear to be consistently very low.
There were no studies involving plasma filtration that provided clearance values. Plasma filtration showed a SC of around unity for IL-6 and G-CSF, and moderately high SC for leukemia inhibitory factor (LIF). This is however coupled with a SC of unity for albumin which is expected from the characteristics of the technique.Citation42 Another study found removal of 40% for IL-18 with plasma filtration, with or without added continuous hemodiafiltration.Citation47
For data on adsorption, perhaps due to the nature of the technique, only percentage removed data was reported; with direct hemoperfusion resulting in around 25% removal for IL-1β, IL-6 and IL-1Ra and about 50% removal for IL-8 and TNF-alpha.Citation46
Only one paper looked at cytokine clearance with ultrafiltration during cardiopulmonary bypass and zero CL was achieved for all cytokines studied.Citation28 Ultrafiltration techniques during CPB has reported unusual and implausible figures of SC exceeding 1 for TNF-alpha.Citation28,Citation30,Citation48 This may indicate extracorporeal-circuit-induced formation of TNF-alpha or an error with measurements. However, the overall removal of all other cytokines as measured by SC was poor (less than 0.1) with this technique. Only one study on this technique reported percentage removed and found 28% removal of IL-6 and 59% removal of IL-8.Citation31
Only clearance values were reported for the extracorporeal liver support systems. The molecular adsorption recycling system (MARS) and Prometheus were the only techniques overall which showed high CL for TNF-alpha ranging from 25 to 29 mL/min.Citation12 The Prometheus system also achieved high CL for IL-10 (46 mL/min) and moderately high CL for sTNFαRII (12 mL/min), while MARS achieved moderate CL with both IL-8 (17 mL/min) and IL-10 (16 mL/min).
Similarly not all measurements were reported for the hybrid techniques. Only one paper evaluated coupled plasma filtration adsorption (CPFA) and found excellent percentage removal for IL-10 and TNF-a (close to 100%).Citation32 There were a number of other hybrid techniques described.Citation14,Citation47,Citation50 Other hybrid techniques generally found low levels of cytokine removal. Standard hemodiafiltration using a filter capable of adsorption found low SC with the technique.Citation14 Standard HDF combined with plasma filtration found only 38.8% removal of IL-18 and zero removal of IL-6. SHEDD-fA (sustained high efficiency daily diafiltration using a mediator adsorbing membrane) which utilizes a combination of hemodiafiltration and adsorption found low levels of removal of IL-6 (21%) with single pass measurements, and this is only when levels of IL-6 in the blood were more than 50 pg/mL with zero removal with lower blood levels of IL-6.Citation50
Discussion
Key findings
We performed a systematic analysis of human clinical studies involving different techniques of EBP to determine their efficacy in the removal of cytokines. We found the high cut-off techniques consistently achieved moderate to high cytokine clearance as demonstrated by CL and SC values. In contrast, standard techniques or ultrafiltration techniques appeared to be inefficient or unreliable in removing cytokines even when coupled with high volume hemofiltration. Plasma filtration achieved high removal of cytokines, as expected, but this clearance was predictably coupled with high albumin loss. CPFA and adsorption techniques showed promising results based on percentage removed data, although only one paper for each technique of could be identified. Hemodiafiltration using filters capable of adsorbing mediators did not offer a high degree of removal through single pass and is largely understudied. Finally, extracorporeal liver support systems may also remove cytokines.
Relation to previous literature
To our knowledge, there are no other reviews of all human studies in the literature which have assessed objective, technical measurements of cytokine removal such as CL, SC and percentage removed for comparison. We had earlier published two systematic reviews on the same topic focusing on ex-vivo cytokine removal and cytokine removal in animal studies respectively.Citation53,Citation54 The findings of the human studies reported here are broadly consistent with the findings of these two previous systematic reviews.
Significance of study findings
Despite an appreciable number of publications studying EBP techniques or devices in ex-vivo, animal experiments and human studies, details of the ideal operative characteristics to ensure the highest efficacy of cytokine removal have not been clearly outlined. Our reviews suggest that high cut-off techniques may be most consistent in offering moderate to high cytokine removal regardless of operating characteristics. Other techniques which also offer significant cytokine clearance includes extracorporeal liver support, plasma filtration and adsorption techniques but their complexity is greater and the number of studies less. Some of these complex techniques require expertise, special equipment, are expensive and cannot be employed around the clock. High cut-off techniques on the other hand use standard hemodialysis or hemofiltration equipment and standard flows of ultrafiltrate (all of which are widely available worldwide) with the only difference being the use of a filter with larger pores. The operating characteristics and the expertise required to initiate this treatment, although remains essential, are largely similar to that employed during standard continuous renal replacement therapies providing advantages for the use of high cut-off technique in terms of feasibility. More importantly, high cut-off techniques also appear to be one of the safest at a clinical level. High volume hemofiltration for example can result in hypophosphatemia, and loss of circuit in CPFA which occurs due to clotting, especially if recurrent, can result in significant blood loss. Albumin loss caused by the high cut-off techniques on the other hand, can be replaced by infusing albumin solutions.
Strengths and limitations
The strength of this review is that it is the first to comprehensively assess all techniques of EBP for their ability to remove cytokines in humans. This information is crucial for the further evolution of blood purification technology as a potential tool to modulate inflammation in sepsis. The limitations of this review include exclusion of articles in languages other than English and the inability to perform statistical comparisons due to the paucity of studies. Some techniques such as adsorption are under-represented as measures relating to clearance and sieving are not relevant to these techniques. The studies included have marked variability in other aspects of treatment and clinical circumstances as well as limited numbers of patients studied. Thus the external validity of our findings is limited. Finally, the clinical significance of cytokine removal like that of electrolyte changesCitation55,Citation56 remains unknown.
Conclusions
In conclusion, our systematic review on EBP techniques found that HCO techniques, plasma filtration and extracorporeal liver support system are able to significantly remove cytokines. Adsorption and CPFA techniques show promise although the data on these techniques are limited. Because of the technical simplicity of HCO techniques, they may represent the most appropriate technique for randomized controlled trials of cytokine removal by EBP.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Beale R, Reinhart K, Brunkhorst F, Dobb G, Levy M, Martin G. Promoting global research excellence in severe sepsis (PROGRESS): lessons from an International Sepsis Registry. Infection. 2009;37:222–232
- Cabre L, Mancebo J, Solsona JF, et al. Multicenter study of the multiple organ dysfunction syndrome in intensive care units: the usefulness of Sequential Organ Failure Assessment scores in decision making. Intensive Care Med. 2005;31:927–933
- Bone RC. Sir Isaac Newton, sepsis, SIRS, and CARS. Crit Care Med. 1996;24:1125–1128
- Cinel I, Opal SM. Molecular biology of inflammation and sepsis: a primer. Crit Care Med. 2009;37:291–304
- Schefold JC, Hasper D, Jörres A. Organ crosstalk in critically ill patients: hemofiltration and immunomodulation in sepsis. Blood Purif. 2009;28:116–123
- Ronco C, Tetta C, Mariano F, et al. Interpreting the mechanisms of continuous renal replacement therapy in sepsis: the peak concentration hypothesis. Artificial Organs. 2003;27:792–801
- Fisher CJ Jr, Dhainaut JF, Opal SM, et al. Recombinant human interleukin 1 receptor antagonist in the treatment of patients with sepsis syndrome. Results from a randomized, double-blind, placebo-controlled trial. Phase III rhIL-1ra Sepsis Syndrome Study Group. J Am Med Assoc. 1994;271:1836–1843
- Opal SM, Fisher CJ Jr, Dhainaut JF, et al. Confirmatory interleukin-1 receptor antagonist trial in severe sepsis: a phase III, randomized, doubleblind, placebo-controlled, multicenter trial. The Interleukin-1 Receptor Antagonist Sepsis Investigator Group. Crit Care Med. 1997;25:1115–1124
- Kellum JA, Bellomo R, Mehta R, Ronco C. Blood purification in non-renal critical illness. Blood Purif. 2003;21:6–13
- Venkataraman R, Subramanian S, Kellum JA. Clinical review: extracorporeal blood purification in severe sepsis. Crit Care. 2003;7:139–145
- Ronco C, Inguaggiato P, D'Intini V, et al. The role of extracorporeal therapies in sepsis. J Nephrol. 2003;16(Suppl 7):S34–S41
- Stadlbauer V, Krisper P, Aigner R, et al. Effect of extracorporeal liver support by MARS and Prometheus on serum cytokines in acute-on-chronic liver failure. Crit Care. 2006;10:R169--R175
- Morgera S, Haase M, Kuss T, et al. Pilot study on the effects of high cutoff hemofiltration on the need for norepinephrine in septic patients with acute renal failure. Crit Care Med. 2006;34:2099–2104
- Peng Y, Yuan Z, Li H. Removal of inflammatory cytokines and endotoxin by veno-venous continuous renal replacement therapy for burned patients with sepsis. Burns. 2005;31:623–628
- Morgera S, Slowinski T, Melzer C, et al. Renal replacement therapy with high-cutoff hemofilters: impact of convection and diffusion on cytokine clearances and protein status. Am J Kidney Dis. 2004;43:444–453
- Morgera S, Rocktäschel J, Haase M, et al. Intermittent high permeability hemofiltration in septic patients with acute renal failure. Intensive Care Med. 2003;29:1989–1995
- Dahaba AA, Elawady GA, Rehak PH, List WF. Procalcitonin and proinflammatory cytokine clearance during continuous venovenous hemofiltration in septic patients. Anaesth Intensive Care. 2002;30:269–274
- Kellum JA, Johnson JP, Kramer D, Palevsky P, Brady JJ, Pinsky MR. Diffusive vs. convective therapy: effects on mediators of inflammation in patient with severe systemic inflammatory response syndrome. Crit Care Med. 1998;26:1995–2000
- Sanchez-Izquierdo JA, Perez Vela JL, Lozano Quintana MJ, Alted Lopez E, Ortuño de Solo B, Ambros Checa A. Cytokines clearance during venovenous hemofiltration in the trauma patient. Am J Kidney Dis. 1997;30:483–488
- Sander A, Armbruster W, Sander B, Daul AE, Lange R, Peters J. Hemofiltration increases IL-6 clearance in early systemic inflammatory response syndrome but does not alter IL-6 and TNF alpha plasma concentrations. Intensive Care Med. 1997;23:878–884
- van Bommel EF, Hesse CJ, Jutte NH, Zietse R, Bruining HA, Weimar W. Impact of continuous hemofiltration on cytokines and cytokine inhibitors in oliguric patients suffering from systemic inflammatory response syndrome. Ren Fail. 1997;19:443–454
- Heering P, Morgera S, Schmitz FJ, et al. Cytokine removal and cardiovascular hemodynamics in septic patients with continuous venovenous hemofiltration. Intensive Care Med. 1997;23:288–296
- Hoffmann JN, Hartl WH, Deppisch R, Faist E, Jochum M, Inthorn D. Effect of hemofiltration on hemodynamics and systemic concentrations of anaphylatoxins and cytokines in human sepsis. Intensive Care Med. 1996;22:1360–1367
- Bellomo R, Tipping P, Boyce N. Interleukin-6 and interleukin-8 extraction during continuous venovenous hemodiafiltration in septic acute renal failure. Ren Fail. 1995;17:457–466
- van Bommel EF, Hesse CJ, Jutte NH, Zietse R, Bruining HA, Weimar W. Cytokine kinetics (TNF-alpha, IL-1 beta, IL-6) during continuous hemofiltration: a laboratory and clinical study. Contrib Nephrol. 1995;116:62–75
- Bellomo R, Tipping P, Boyce N. Continuous veno-venous hemofiltration with dialysis removes cytokines from the circulation of septic patients. Crit Care Med. 1993;21:522–526
- Byrick RJ, Goldstein MB, Wong PY. Increased plasma tumor necrosis factor concentration in severe rhabdomyolysis is not reduced by continuous arteriovenous hemodialysis. Crit Care Med. 1992;20:1483–1486
- Antunes N, Dragosavc D, Petrucci Junior O, et al. The use of ultrafiltration for inflammatory mediators removal during cardiopulmonary bypass in coronary artery bypass graf surgery. Rev Bras Cir Cardiovasc. 2008;23:175–182
- Brancaccio G, Villa E, Girolami E, et al. Inflammatory cytokines in pediatric cardiac surgery and variable effect of the hemofiltration process. Perfusion. 2005;20:263–268
- Berdat PA, Eichenberger E, Ebell J, et al. Elimination of proinflammatory cytokines in pediatric cardiac surgery: analysis of ultrafiltration method and filter type. J Thorac Cardiovasc Surg. 2004;127:1688–1696
- Dittrich S, Aktuerk D, Seitz S, et al. Effects of ultrafiltration and peritoneal dialysis on proinflammatory cytokines during cardiopulmonary bypass surgery in newborns and infants. Eur J Cardiothorac Surg. 2004;25:935–940
- Ronco C, Brendolan A, Lonnemann G, et al. A pilot study of coupled plasma filtration with adsorption in septic shock. Crit Care Med. 2002;30:1250–1255
- Kiziltepe U, Uysalel A, Corapcioglu T, Dalva K, Akan H, Akalin H. Effects of combined conventional and modified ultrafiltration in adult patients. Ann Thorac Surg. 2001;71:684–693
- Bogă M, Islamoğlu F, Badak I, et al. The effects of modified hemofiltration on inflammatory mediators and cardiac performance in coronary artery bypass grafting. Perfusion. 2000;15:143–150
- Hoffmann JN, Werdan K, Hartl WH, Jochum M, Faist E, Inthorn D. Hemofiltrate from patients with severe sepsis and depressed left ventricular contractility contains cardiotoxic compounds. Shock. 1999;12:174–180
- Toft P, Kehler D, Brandslund I I, Tønnsen E. The immunological effects of continuous veno-venous hemodiafiltration in critically ill patients. Crit Care. 1999;3:159–165
- Watanabe T, Sakai Y, Mayumi T, et al. Effect of ultrafiltration during cardiopulmonary bypass for pediatric cardiac surgery. Artif Organs. 1998;22:1052–1055
- Wang W, Huang HM, Zhu DM, Chen H, Su ZK, Ding WX. Modified ultrafiltration in paediatric cardiopulmonary bypass. Perfusion. 1998;13:304–310
- Hoffmann JN, Faist E, Deppisch R, Hartl WH, Inthorn D. Hemofiltration in human sepsis: evidence for elimination of immunomodulatory substances. Contrib Nephrol. 1995;116:76–79
- Xie H, Ji D, Gong D, et al. Continuous veno venous hemofiltration in treatment of acute necrotizing pancreatitis. Chin Med J (Engl). 2003;116:549–553
- Mariano F, Tetta C, Guida G, Triolo G, Camussi G. Hemofiltration reduces the serum priming activity on neutrophil chemiluminescence in septic patients. Kidney Int. 2001;60:1598–1605
- Reeves JH, Butt WW, Shann F, et al. Continuous plasma filtration in sepsis syndrome. Plasma filtration in Sepsis Study Group. Crit Care Med. 1999;27:2096–2104
- De Vriese AS, Colardyn FA, Philippé JJ, Vanholder RC, De Sutter JH, Lameire NH. Cytokine removal during continuous hemofiltration in septic patients. J Am Soc Nephrol. 1999;10:846–853
- Clar A, Bowers MC, Larson DF. Derivation of sieving coefficients to determine the efficacy of the hemoconcentrator in removal of four inflammatory mediators produced during cardiopulmonary bypass. ASAIO J. 1997;43:163–170
- Hoffmann JN, Hartl WH, Deppisch R, Faist E, Jochum M, Inthorn D. Hemofiltration in human sepsis: evidence for elimination of immunomodulatory substances. Kidney Int. 1995;48:1563–1570
- Tsuchida K, Takemoto Y, Sugimura K, Yoshimura R, Nakatani T. Direct hemoperfusion by using Lixelle column for the treatment of systemic inflammatory response syndrome. Int J Mol Med. 2002;10:485–488
- Yonekawa C, Nakae H, Tajimi K, Asanuma Y. Effectiveness of combining plasma exchange and continuous hemodiafiltration in patients with postoperative liver failure. Artif Organs. 2005;29:324–328
- Tallman RD, Dumond M, Brown D. Inflammatory mediator removal by zero-balance ultrafiltration during cardiopulmonary bypass. Perfusion. 2002;17:111–115
- Cole L, Bellomo R, Journois D, Davenport P, Baldwin I, Tipping P. High-volume hemofiltration in human septic shock. Intensive Care Med. 2001;27:978–986
- Nishida O, Nakamura T, Kuriyama N, et al. Sustained high-efficiency daily diafiltration using a mediator-adsorbing membrane (SHEDD-fA) in the treatment of patients with severe sepsis. Contrib Nephrol. 2011;173:172–181
- Schilder L, Nurmohamed SA, ter Wee PM, et al. Effect of anticoagulation regimens on handling of interleukin-6 and -8 during continuous venovenous hemofiltration in critically ill patients with acute kidney injury. Cytokine. 2012;60:601–607
- Oishi K, Mimura-Kimura Y, Miyasho T, et al. Association between cytokine removal by polymyxin B hemoperfusion and improved pulmonary oxygenation in patients with acute exacerbation of idiopathic pulmonary fibrosis. Cytokine. 2013;61:84–89
- Atan R, Crosbie D, Bellomo R. Techniques of extracorporeal cytokine removal: a systematic review of the literature. Blood Purif. 2012;33:88–100
- Atan R, Crosbie D, Bellomo R. Techniques of extracorporeal cytokine removal: a systematic review of the literature on animal experimental studies. Int J Artif Organs. 2013;36:149–158
- Brain M, Anderson M, Parkes S, Fowler P. Magnesium flux during continuous venous hemodiafiltration with heparin and citrate anticoagulation. Crit Care Resusc. 2012;14:274–282
- Brain M, Parkes S, Fowler P, Robertson I, Brown A. Calcium flux in continuous venovneous hemodiafiltration with heparin and citrate anticoagulation. Crit Care Resusc. 2011;13:72–81