Abstract
Goodpasture’s syndrome complicating pregnancy is extremely rare and dialysis requiring anti GBM disease with renal recovery is uncommon. We report a case of a 23-year-old primi gravida who presented with Goodpasture’s syndrome during thirteenth week of pregnancy. She was initiated on steroids and cytotoxic drugs along with intensive plasma exchange and alternate day hemodialysis. Her pregnancy was terminated at 15 weeks. Patient improved dramatically with treatment, her renal functions normalized and her Anti GBM antibody titer became negative.
Introduction
There are only a few case reports of Anti GBM disease during pregnancy and in most of them renal failure was not dialysis requiring. In all cases of dialysis requiring renal failure patient reached end stage renal disease requiring long-term renal replacement therapy.Citation1–5 Even in general population renal recovery is very rare in dialysis requiring Anti GBM disease.Citation6
We describe a case of dialysis requiring Anti GBM disease that presented in early pregnancy and had dramatic improvement following termination of pregnancy.
Case Report
A 23-year-old primi gravida presented with history of breathlessness and generalized edema associated with reduced urine output in the thirteenth week of pregnancy. She had history of hyperemesis gravidarum from onset of pregnancy which was treated with antiemetics. She gave history of cough two weeks duration prior to admission and had an episode of cola coloured urine one week later. There was no fever, dysuria or oliguria at that time. She consulted a local hospital and urine analysis showed proteinuria, pyuria and microscopic hematuria. She was treated with amoxicillin suspecting urinary tract infection.
On clinical examination she was alert, afebrile, tachypneic, had pallor, bilateral pitting pedal edema and facial puffiness. Her pulse rate was 88/minute and blood pressure 110/70 mm Hg. Jugular venous pressure was elevated 6 cm above sternal angle. Chest examination revealed bilateral basal crepitations. Rest of system examination was within normal limits.
Laboratory Investigations on admission are shown in . Ultrasound abdomen showed right kidney 11.5 cm ×5 cm left kidney 11.2 cm × 5.4 cm with bilateral increased echogenicity and normal cortico medullary differentiation. There was mild hydroureteronephrosis on right side and single live intra uterine gestation.
Table 1. Laboratory investigations at presentation.
During the hospital stay her renal function deteriorated with blood urea of 112 mg% and serum creatinine 8.2 mg%. She was initiated on hemodialysis and underwent a renal biopsy on fifth day of admission.
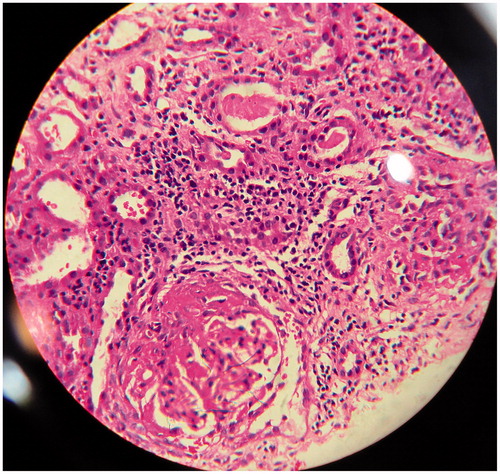
Renal biopsy revealed 20 glomeruli of which 4 were obsolescent. The obsolescent glomeruli were small and globally sclerotic. The viable glomeruli showed segmental necrosis with nuclear debris and hyaline thrombi within glomerular capillaries and hilar arterioles. There were crescents in 12 glomeruli (60%; cellular-8, fibrocelluar-4) (). The underlying tufts did not show significant endocapillary proliferation. The tubules showed focal denudation of the lining epithelium, hyaline cast and RBC casts. There was interstitial edema and mild diffuse interstitial inflammation. One hilar arteriole showed thrombi.
Immunofluorescence revealed linear 2 + IgG and C3 along glomerular capillary loops with 1 to 2 + mesangial IgA. IgM and C1q were negative.
A diagnosis of crescentic glomerulonephritis consistent with anti glomerular basement membrane disease with background IgA nephropathy with mild global glomerulosclerosis and moderate acute on chronic tubulointerstitial nephritis was made and she was treated with daily plasmapheresis for 2 weeks along with oral cyclophosphamide 100 mg daily. She was continued on alternate day hemodialysis. Since she was started on cytotoxic drugs, pregnancy was terminated at 15 weeks of gestation. Her urine output improved dramatically after termination of pregnancy and dialysis was discontinued. On review her renal function gradually improved with latest blood urea 42 mg% and serum creatinine 1.2 mg%. Her anti GBM antibody titre also decreased to 1.2 IU/mL.
Discussion
Rapidly progressive glomerulonephritis mediated by anti glomerular basement membrane (anti GBM) antibody deposition is a rare cause of renal insufficiency in association with pregnancy. There are only seven case reports of Goodpasture’s disease during pregnancy reported in literature.Citation1--Citation5,Citation7
Deubner et al. reported one case of a 21-year-old female who presented with glomerulonephritis during pregnancy. She had a flare of disease post delivery and potential role of placenta in amelioration of disease during pregnancy was suggested. It was postulated that placenta may serve as an adsorbent by providing abundant basement membrane surfaces for binding of circulating anti basement membrane antibodies.Citation1 In our case severe renal failure occurred while she was pregnant and had high titers of anti GBM antibody. Moreover, she had definite clinical improvement following termination of pregnancy. Hence, the protective role of placenta is doubtful.
Even though our patient had completed 5 sessions of plasma exchange and was on cyclophosphamide for 1 week before termination of pregnancy, she remained oligoanuric and dialysis dependent. But after termination of pregnancy her output improved dramatically. We hence consider the possibility of termination of pregnancy playing a role in her rapid recovery.
Al –Harbi et al described the case of a 30-year-old female with acute renal failure at 28 weeks of gestation, who was treated with intensive hemodialysis along with steroids and delivered at 34 weeks of gestation. Anti-glomerular basement membrane (GBM) antibody mediated crescentic glomerulonephritis was diagnosed 1 week post delivery. Anti GBM antibody which was negative during pregnancy became positive post delivery. But the patient never recovered renal function and required regular maintenance hemodialysis.Citation2 In our case, anti-GBM antibody titers were very high even during pregnancy and became negative after treatment. She also had very good renal recovery with aggressive immunosuppression along with intensive plasmapheresis and hemodialysis.
Nielssen et al. described a 19-year-old female who presented with acute glomerulonephritis in second trimester of pregnancy and had a stillbirth at 28 weeks of gestation. She developed acute dialysis requiring renal failure post partum. Renal biopsy showed crescentic glomerulonephritis with linear immune fluorescence. But in spite of treatment with plasma exchange, steroids and cyclophosphamide she became dialysis dependent.Citation3
Patients with crescentic glomerulonephritis having more than 50% crescents with severe dialysis dependent renal failure rarely recover renal function. Hence plasmapheresis and immunosuppression are not recommended if there is no active hemoptysisCitation8 Our patient however surprisingly had normalization of renal function with immunosuppression which shows that immunosuppression may have a beneficial role in dialysis requiring renal failure in pregnancy along with termination of pregnancy.
All patients with a preconceptional diagnosis of Goodpasture’s syndrome had preterm delivery due to several complications and most of them never recovered renal function and subsequently required renal transplantatation.Citation1–5 Our case is unique in that she recovered despite having dialysis dependent renal failure and that the improvement appeared to follow termination of pregnancy. The role of pregnancy in causing Anti-GBM disease and possible amelioration following termination of pregnancy is possible and needs further study whether the placenta or some other alterations caused by pregnancy are responsible.
Our patient had mesangial deposition of IgA in addition to linear IgG deposits. Wang et al. had described a case of anti-GBM disease with extensive IgA deposits in the mesangium and suggested ongoing glomerular pathological changes alter GBM components, triggering an autoimmune reaction to modified antigens as pathogenic mechanism of coexisting IgA nephropathy.Citation9,Citation10. Whether there was coexisting IgA nephropathy or whether IgA was an innocent bystander in our patient is not clear.
Even though our patient had overt hemoptysis it could not be substantiated with chest X-ray or CT scan due to risk of radiation exposure considering the fact that she was pregnant. DLCO rise was also not done as it was not available in our hospital. But she had a drop in her hemoglobin following hemoptysis. Later her pregnancy had to be terminated when her renal condition necessitated use of cytotoxic drugs. Her subsequent dramatic improvement raises the suspicion of a deleterious effect of pregnancy in our patient.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Deubner H, Wagnild JP, Wener MH, Alpers CE. Glomerulonephritis with anti glomerular basement membrane antibody during pregnancy: potential role of placenta in amelioration of disease. Am J Kidney Dis. 1995;25:330–335
- Al-Harbi A, Malik GH, Al-Mohaya SA, Akhtar M. Anti glomerular basement membrane antibody disease presenting as acute renal failure during pregnancy. Saudi J Kidney Dis Transplant. 2003;14:516–521
- Nilssen DE, Talseth T, Brodwall EK. The many faces of Goodpasture’s syndrome. Acta Med Scand. 1986;220:489–491
- Yankowitz J, Kuller JA, Thomas RL. Pregnancy complicated by good pastures syndrome. Obstet Gynecol. 1992;79:806–808
- Vasiliou DM, Maxwell C, Prakeshkumar S, Sermer M. Good Pastures syndrome in a pregnant woman. Obstet Gynecol. 2005;106:1196–1199
- Levy JB, Turne AN. Rees AJ, Pusey CD. Long-term outcome of anti–glomerular basement membrane antibody disease treated with plasma exchange and immunosuppression. Ann Intern Med. 2001;134:1033–1042
- Wells SR, Kuller JA, Thorp JM Jr. Pregnancy in a patient with good pastures syndrome and renal transplantation. Am J Perinatol. 1996;13:79–80
- KDIGO Clinical Practice Guidelines for Glomerulonephritis June 2012, volume 2, issue 2
- Fischer EG, Lager DL. Anti–glomerular basement membrane glomerulonephritis a morphologic study of 80 cases. Am J Clin Pathol. 2006;125:445–450
- Aifeng W, Yongping W, Guobao W, Zhanmei Z, Zhang X. Xiaohui Tan Mesangial IgA deposits indicate pathogenesis of anti-glomerular basement membrane disease. Mol Med Reports. 2012;5:1212–1214