Abstract
Hepatitis C virus (HCV) infection is a global public health problem. Chronic HCV infection is an important cause of chronic liver disease. Since the first reported association between HCV and membranoproliferative glomerulonephritis (MPGN) in 1993, HCV has been described with other types of glomerular diseases, although less frequently. Focal segmental glomerulosclerosis (FSGS) is one such glomerular disease that has been rarely reported in association with HCV. Antiviral therapy with interferon and ribavirin has been shown to be beneficial in HCV-associated MPGN. The optimal therapy of HCV-associated FSGS is not currently known. To our knowledge, long-term response to pegylated interferon monotherapy in treatment of HCV-associated FSGS has not been reported. We report an adult patient with HCV-associated FSGS who presented with nephrotic syndrome and renal failure. Treatment with pegylated interferon alfa-2a monotherapy resulted in sustained virological response with a clinical remission of nephrotic syndrome and stabilization of renal function. Patient continued to remain in clinical remission of nephrotic syndrome with stable renal function, 5 years after treatment. We also briefly review the literature on HCV-associated glomerular diseases, particularly HCV-associated FSGS.
Introduction
Hepatitis C virus (HCV) infection is the most common chronic blood borne infection in the United States.Citation1 Chronic HCV infection can lead to chronic liver disease, cirrhosis and hepatocellular carcinoma. Extrahepatic complications have also been reported in as much as 36% of HCV positive patients.Citation2 The exact incidence of glomerulonephritis in HCV infected patients is not known. Type I membranoproliferative glomerulonephritis (MPGN) associated with type II cryoglobulinemia has been recognized as the most common renal manifestation of HCV infection.Citation3 Less often HCV is associated with membranous nephropathy (MN),Citation4 IgA nephropathy,Citation5 fibrillary and immunotactoid glomerulopathyCitation6 and focal segmental glomerulosclerosis (FSGS).Citation7 While combination of antiviral therapy with interferon and ribavirin has demonstrated efficacy in treatment of HCV-associated MPGN, optimal treatment of HCV-associated FSGS is not known. Long-term response to antiviral therapy in HCV-associated FSGS is also unknown. We report a patient with HCV infection who presented with massive proteinuria and renal failure. Kidney biopsy revealed FSGS. Treatment with pegylated interferon in our patient was followed by complete clinical remission of the nephrotic syndrome as well as a dramatic decrease in HCV viral load. Patient remains in clinical remission of nephrotic syndrome with stable renal function several years after treatment with peginterferon.
Case
A 47-year-old Hispanic male was referred by his primary care physician for evaluation of nephrotic range proteinuria. He presented with 1 month history of worsening bilateral lower extremity edema. He denied any past history of diabetes, hypertension, hepatitis or blood transfusion. Review of systems was negative for fever, chills, dyspnea, gross hematuria, arthralgias or rash. He denied use of any medications, including non-steroidal anti-inflammatory drugs and herbal medications. There was no history of intravenous drug use. He was married but admitted to having multiple sexual partners.
On physical examination, his blood pressure was elevated at 146/100 mm Hg and there was 3+ pitting edema of his lower extremities. The rest of the examination was unremarkable. At the time of presentation, serum creatinine was 1.7 mg/dL, total protein was 4.3 g/dL, serum albumin was 1.9 g/dL, total cholesterol was 310 mg/dL, and LDL cholesterol was 197 mg/dL. Liver function tests and complete blood count were normal. A 24-h urine collection revealed 19.5 g of protein.
Work up for secondary causes of nephrotic syndrome revealed a positive HCV antibody. Quantitative HCV polymerase chain reaction (PCR) assay revealed 495,000 copies of viral RNA per mL. HCV genotype testing showed genotype 1a. Hepatitis B surface antigen, antinuclear antibody, cryoglobulins and human immunodeficiency virus (HIV) antibody were negative. Complement levels were normal. Sonogram revealed normal sized kidneys. An ultrasound assisted kidney biopsy was subsequently performed.
Kidney biopsy findings
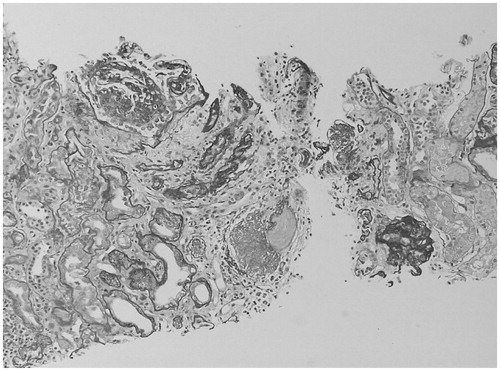
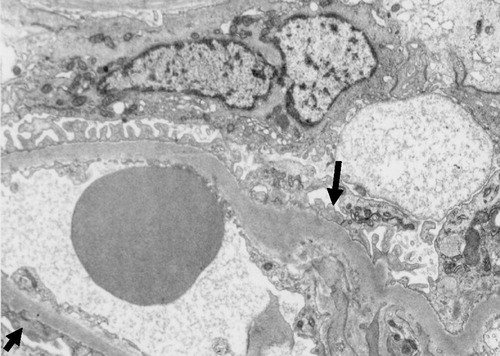
On renal biopsy, 22 glomeruli were identified. Four glomeruli were segmentally sclerosed while another four were globally sclerosed. There was extensive tubular atrophy () with increased interstitial infiltrate. Immunofluorescence was negative for immune complex deposition. Light microscopy and immunofluorescence findings were consistent with FSGS. Electron microscopy revealed focal effacement of podocyte foot processes () suggestive of a secondary cause of FSGS.
Clinical follow-up
The patient was initially started on furosemide for edema management. He was also started on atorvastatin and an angiotensin 2-receptor blocker. Lower extremity edema resolved in about 3 months. In view of positive HCV serology and kidney biopsy findings suggestive of secondary cause for FSGS, patient was referred to a hepatologist. Patient however refused to undergo a liver biopsy. Patient was subsequently started on subcutaneous peginterferon alfa-2a 180 micrograms weekly for 12 months. Before initiation of interferon therapy, his serum creatinine increased to 2.1 mg/dL. After 3 months of therapy, HCV RNA became undetectable. Spot urine total protein to creatinine (TP/CR) ratio started to decrease dramatically. At the completion of interferon treatment, spot urine total protein to creatinine ratio decreased to 1 and serum albumin returned to normal. His renal function continued to remain stable 5 years after completing interferon therapy with a serum creatinine of 2.1 mg/dL. His spot urine TP/CR ratio had further decreased to 0.2. His HCV RNA remained undetectable.
Discussion
HCV is a RNA virus belonging to flavivirus family. Since the discovery of HCV by molecular cloning many years ago,Citation8 it has been recognized as a major public health problem worldwide. According to the third National Health and Nutrition Examination Survey (NHANES), 3.9 million of the US civilian population have been infected with HCV, of whom 2.7 million (74%) have chronic infection.Citation1 It is most common among non-Caucasian men, ages 30 to 49 years.Citation1 HCV infection is responsible for chronic liver disease and a wide variety of extrahepatic manifestations such as kidney disease, porphyria cutanea tarda, cardiomyopathy, sialadenitis, diabetes mellitus and lymphoproliferative disorders.Citation2
There is a continuing controversy about positive HCV serology and development and progression of kidney disease but several surveys suggest that infection with HCV is associated with an increased risk of having or developing renal insufficiency or proteinuria. Noureddine et al.Citation9 evaluated cohort of patients with biopsy proven chronic glomerulonephritis and reported an increased risk of progression of CKD in patients with positive serology for HCV compared with HCV negative patients. A positive HCV serology was also noted to be an independent and significant risk factor for proteinuria.Citation10
The incidence and prevalence of HCV-associated glomerular disease is not well known. In a retrospective analysis from Europe of 284 patients with biopsy proven glomerulonephritis, prevalence of anti-HCV antibody was noted to be 13%.Citation11 The association between HCV and glomerular disease was first described by Johnson et al.Citation12 in 1993. Type I MPGN associated with Type II cryoglobulinemia remains the most frequently observed form of kidney disease in HCV infection.Citation3 Other less commonly seen glomerular lesions include MPGN without cryoglobulinemia, membranous nephropathy and IgA nephropathy.Citation5 Rarely, there have been reports of FSGS,Citation7 and fibrillary or immunotactoid glomerulopathies.Citation6 In addition to symptomatic renal disease, clinically silent glomerular disease has also been described in patients with HCV infection, primarily in those who undergo liver transplantation for cirrhosis due to chronic HCV infection.Citation13 The natural history of these HCV-associated nephropathies is characterized by remission and relapsing phases; however, the long term outcome is not well known.
Association between HCV and FSGS was first noted by Altraif et al.Citation7 in 1995 when patients with HCV cirrhosis underwent kidney biopsy for proteinuria. Subsequently, Ezaki et al.Citation14 reported a case of HCV and FSGS who responded to antiviral therapy. In this report, a 30-year-old male with HCV and nephrotic syndrome was found to have FSGS on renal biopsy. Nephrotic syndrome resolved and HCV RNA became undetectable after 6 months of interferon therapy. However, 5 months after stopping interferon therapy, HCV RNA became elevated with recurrence of nephrotic syndrome. This again responded to interferon therapy.Citation14 Bruchfeld et al.Citation15 reported a series of seven patients with HCV-associated glomerular disease and renal failure that were treated with interferon and ribavirin (five patients received interferon alfa-2b and two received pegylated interferon alfa-2b). Of the seven patients, five had MPGN, one had focal necrotizing glomerulonephritis, and only one had FSGS on kidney biopsy.Citation15 The patient with focal necrotizing glomerulonephritis and one of the five MPGN patients had cryoglobulinemia and manifestations of vasculitis. Six of the seven patients in the above series became HCV-RNA-PCR negative within 12 weeks of antiviral therapy. The remaining patient who did not achieve a viral response was the one who did not tolerate interferon therapy. Interestingly, this patient achieved renal remission with ribavirin monotherapy. Four of six patients (including the one with FSGS) that became HCV-RNA-PCR negative following combination antiviral therapy achieved and maintained renal remission.Citation15 Of the remaining two patients who responded to combination antiviral therapy, one had achieved only partial renal remission despite maintaining virological remission, while the other maintained renal remission despite having a virological relapse.Citation15
The pathogenesis of the glomerular injury in HCV infection is not well known. The pathogenesis of HCV-associated MPGN is believed to result from deposition of circulating immune complexes of HCV, anti-HCV IgG antibodies and rheumatoid factor at the site of injury.Citation16 However, it is not clear how glomerular injury occurs in other forms of glomerulonephritis where there is absence of immune complex deposition. Recently, it has been shown that overexpression of toll-like receptor 3 could have a pathogenic role in HCV positive patients with glomerulonephritis.Citation17 Recently, Sansonno et al. managed to isolate HCV RNA from kidney biopsy specimens of patients with HCV-associated glomerulonephritis using a laser capture microdissection.Citation18 However, it should also be kept in mind that isolation of viral particles from kidney biopsy specimen does not necessarily indicate that the HCV is the cause of renal injury.Citation19
Currently, standard treatment for HCV genotype 2 or 3 infection in patients with normal kidney function includes a combination of pegylated interferon alfa-2a plus ribavirin for 24 weeks regardless of the baseline viral load.Citation20 HCV genotype 1 is associated with lower rates of sustained virologic response compared to other genotypes and requires a longer duration of therapy.Citation20 As per the manufacturer recommendations, a creatinine clearance <50 mL/min is a contraindication to the use of ribavirin due to risk of life threatening hemolytic anemia. Interestingly, our patient who had HCV genotype 1a responded extremely well with sustained virologic response several years after pegylated interferon monotherapy. The use of antiviral therapy in HCV positive patients with glomerulonephritis is targeted at eliminating the virus and reducing the generation of HCV-related antibodies and immune complexes. Besides HCV antiviral therapy, renal protective measures such as blood pressure control and antiproteinuric agents like angiotensin converting enzyme inhibitors or angiotensin receptor blockers have been used to treat HCV-associated glomerular diseases.Citation21
The optimal therapy of HCV-associated FSGS is not currently known. Evidence of the effect of antiviral therapy in HCV-associated FSGS is difficult to interpret due to lack of controlled studies, small number of patients and variation in treatment regimen. Recently, combination therapy with interferon alfa-2a and ribavirin was reported to cause stabilization of HCV-associated collapsing FSGS.Citation22
To the best of our knowledge, long-term response to interferon monotherapy in HCV genotype 1-associated FSGS has not been reported. Treatment with pegylated interferon monotherapy in our patient resulted in both clearing of HCV viremia and complete clinical remission of nephrotic syndrome. His renal function also continued to remain stable, 5 years after completing interferon therapy. We therefore believe that HCV infection had a pathogenic role in development of FSGS in our patient as evidenced by dramatic improvement in the clinical condition following successful treatment of HCV. Nevertheless, further studies are required to investigate the exact pathogenesis and treatment of HCV-associated FSGS.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgements
Dr. Hitesh H. Shah is the Director of the Nephrology Fellowship Program at the Hofstra North Shore-LIJ School of Medicine. Dr. Chinmay Patel is a Nephrology Fellow at the Hofstra North Shore-LIJ School of Medicine. This case was presented as poster presentation at National Kidney Foundation 2011 Spring Clinical Meetings in Las Vegas, NV, in April 2011.
References
- Kim WR. The burden of hepatitis C in the United States. Hepatology. 2002;36:S30–S34
- Sterling RK, Bralow S. Extrahepatic manifestations of hepatitis C virus. Curr Gastroenterol Rep. 2006;8:53–59
- Fabrizi F, Dixit V, Martin P, Messa P. The evidence-based epidemiology of HCV-associated kidney disease. Int J Artif Organs. 2012;35:621–628
- Stehman-Breen C, Alpers CE, Couser W, et al. Hepatitis C virus associated membranous glomerulonephritis. Clin Nephrol. 1995;43:141–147
- Sumida K, Ubara Y, Hoshino J, Suwabe T, Nakanishi S, Hiramatsu R, et al. Hepatitis C virus-related kidney disease: various histological patterns. Clin Nephrol. 2010;74:446–456
- Markowitz GS, Cheng JT, Colvin RB, Trebbin WM. Hepatitis C viral infection is associated with fibrillary glomerulonephritis and immunotactoid glomerulopathy. J Am Soc Nephrol. 1998;9:2244–2252
- Altraif IH, Abdulla AS, al Sebayel MI, Said RA, al Suhaibani MO, Jones AA. Hepatitis C associated glomerulonephritis. Am J Nephrol. 1995;15:407–410
- Choo Q-L, Kuo G, Wener AJ, et al. Isolation of cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science. 1989;244:359–362
- Noureddine LA, Usman SA, Yu Z, Moorthi RN, Moe SM. Hepatitis C increases the risk of progression of chronic kidney disease in patients with glomerulonephritis. Am J Nephrol. 2010;32:311–316
- Fabrizi F, Martin P, Dixit V, Messa P. Hepatitis C virus infection and kidney disease: a meta-analysis. Clin J Am Soc Nephrol. 2012;7:549–557
- Fabrizi F, Pozzi C, Farina M, Dattolo P, Lunghi G, Badalamenti S, et al. Hepatitis C virus infection and acute or chronic glomerulonephritis: an epidemiological and clinical appraisal. Nephrol Dial Transplant. 1998;13:1991–1997
- Johnson RJ, Gretch DR, Yamabe H, et al. Membranoproliferative glomerulonephritis associated with hepatitis C infection. N Engl J Med. 1993;328:465–470
- McGuire BM, Julian BA, Bynon JS Jr, et al. Brief communication: glomerulonephritis in patients with hepatitis C cirrhosis undergoing liver transplantation. Ann Intern Med. 2006;144:735–741
- Ezaki Y, Tanaka U, Minoshima S, et al. FSGS associated with hepatitis C and decrement of proteinuria by interferon. Nippon Jinzo Gakkai. 1999;41:83–88
- Bruchfeld A, Lindahl K, Stahle L, et al. Interferon and ribavirin treatment in patients with hepatitis C associated renal disease and renal insufficiency. Nephrol Dial Transplant. 2003;18:1573–1580
- Yamabe H, Johnson RJ, Gretch Dr, et al. Hepatitis C virus infection and membranoproliferative glomerulonephritis in Japan. J Am Soc Nephrol. 1995;6:220–223
- Abou-Zeid AA, El-Sayegh HK. Toll-like receptor 3 gene expression in Egyptian patients with glomerulonephritis and hepatitis C virus infection. Scand J Clin Lab Invest. 2011;71:456–461
- Sansonno D, Lauletta G, Montrone M, et al. Hepatitis C virus RNA and core protein in kidney glomerular and tubular structures isolated with laser capture micro dissection. Clin Expt Immunology. 2005;140:498–506
- Motta M, Malaguarnera M, Restuccia N, Romano M, Vinci E, Pistone G. Focal segmental glomerulosclerosis and hepatitis C virus: a case report. Panminerva Med. 2001;43:49–52
- Mihm U, Herrmann E, Sarrazin C, Zeuzem S. Review article: predicting response in hepatitis C virus therapy. Aliment Pharmacol Ther. 2006;23:1043–1054
- Morales JM, Kamar N, Rostaing L. Hepatitis C and renal disease: epidemiology, diagnosis, pathogenesis and therapy. Contrib Nephrol. 2012;176:10–23
- Sperati J. Stabilization of Hepatitis C associated collapsing focal segmental glomerulosclerosis with interferon a-2a and ribavirin. Clin Nephrol 2012. doi 10.5414/CN107337