Abstract
Intravascular lymphoma (IVL) is a rare extra nodal subtype (usually of B-cell origin) presenting with infiltration of large neoplastic lymphocytes into lumina of blood vessels, leading to vascular occlusion. The early diagnosis is very crucial, however it is usually diagnosed postmortem investigation in most of the cases. A 56-year-old female presented with elevated creatinine level, and anasarca-type edema that superimposed with hard, indurated, erythematous plaques extending to inguinal region, abdomen, anterior aspect of chest, and face. B-cell IVL was confirmed with skin biopsy. The patient had some degree of clinical improvement following chemotherapy. B-cell IVL presenting with anasarca edema was not previously reported in the literature. Even if its rarity, IVL should be considered in the differential diagnosis of renal failure with anasarca edema.
Introduction
Intravascular lymphoma (IVL) is a subtype of extra nodal non-Hodgkin lymphoma (usually of B-cell origin), with an incidence of less than one case per million.Citation1 Intravascular large B-cell lymphoma (B-cell IVL) is an aggressive, disseminated and systemic disease presenting with massive proliferation of large tumor cells within the lumina of small to medium-sized vessels.Citation2 The overall mortality rate ranges from 50% to 80 % in postmortem studies.Citation1
The diagnosis of IVL can be challenging due to its propensity to mimic other diseases. An antemortem diagnosis of IVL is very difficult; therefore a postmortem diagnosis of IVL can be made in most cases. However, the median survival is approximately 5 years in the cases with early diagnosis.Citation3 A patient was reported with a diagnosis of IVL manifesting with unexplained renal failure, and anasarca type edema that superimposed with a skin eruption.
Case
A 56-year-old female presented to the medicine clinic for anasarca edema extending eyelids, and whole body. She was diagnosed with acute renal failure, and admitted to the hospital for further investigation. The symptoms were started one month ago. The edema with redness first started in the abdomen and eyelid that worsening progressively.
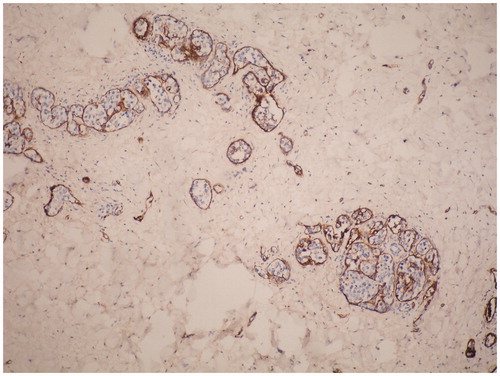
The laboratory investigations revealed elevated levels of creatinine 4.54 mg/dL (normal: 0.7–1.3 mg/dL), BUN 58 mg/dL (normal: 0–50 mg/dL), urea 123 mg/dL (normal: 0–50 mg/dL), uric acid 7.61 mg/dL (normal: 0–5.7 mg/dL), erythrocyte sedimentation rate 42 mm/h (normal: 1–20 mm/h), C-reactive protein 105 mg/L (normal: 0–5 mg/L); and decreased levels of total protein 5.1 g/dL (normal: 6.6–8.7 g/dL) and albumin 3.46 g/dL (normal: 3.5–5.2 g/dL) levels. The other laboratory tests including complete blood count were within normal limits. The abdomen computed tomography showed a right pleural effusion (the thickest part was 24 mm size); subsegmental atelectasia in the right lung lower zone; hepatomegaly with 168 mm size; subcutaneous and cutaneous edema on the anterior abdomen; and inguinal lymph nodes (the biggest one was 14 × 7 mm diameter). The echocardiogram demonstrated a left ventricle diastolic dysfunction. She had decreased glomerular filtration rate 5 mL/min (normal range: 90–120 mL/min), oliguria and developed oliguric symptoms. Thus she underwent hemodialysis. Low central venous pressure was detected even if having anasarca edema. She was consulted to dermatology because of skin findings. The dermatological examination showed anasarca edema extending to the abdomen, inguinal region and face (); and non-pitting, indurated, light erythematous diffuse plaques with orange peel-like appearance on the abdomen (). The histological examination of abdominal skin biopsy showed large atypical lymphocytes within capillaries and larger blood vessels in the middle and reticular dermis (). The immunohistochemical analysis was positive for CD20 (), Factor-8 () and leukocyte common antigen (LCA) (CD45); and negative for CD3, CD30, HMB45, S100, CD117, cytokeratin, CK7, CK20, CEA, and EMA. A diagnosis of large B-cell IVL was made based on the clinical and histopathological findings.
Figure 1. (a) Diffuse anasarca-type edema on the abdomen, chest, and face. (b) Mild erythematous, indurated, hard, diffuse plaques.

Figure 2. Intravascular large B-cell lymphoma. The large tumor cells fill the vessels in the skin biopsy (H&E stain, original magnification × 4 objective).
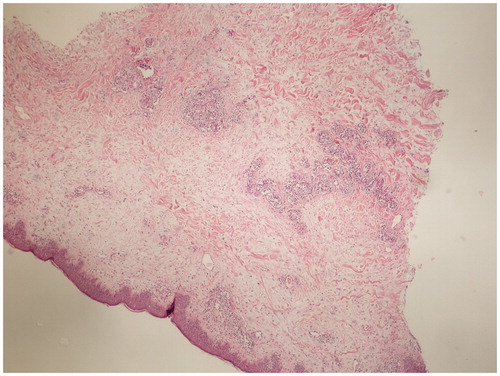
Figure 3. Intravascular large B-cell lymphoma. The tumor cells are highlighted by staining for CD 20 (Immunoperoxidase stain, original magnification × 10 objective).
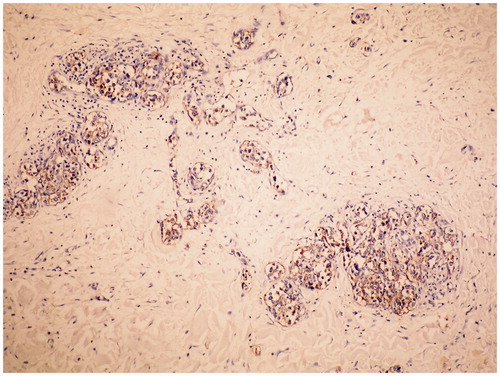
Figure 4. Intravascular large B-cell lymphoma. The vessels that filling with the tumor cells are highlighted by staining for Factor VIII (Immunoperoxidase stain, original magnification × 10 objective).
A treatment with R-CHOP (rituximab, vincristine, doxorubicin, cyclophosphamide and prednisolone) chemotherapy was initiated. After the first cycle of treatment, the skin lesions were clinically resolved. After lowering creatinine level, resolving of edema, and increasing of urine output, the hemodialysis sessions were terminated. The chemotherapy cure was continued for 11 months following the diagnosis ().
Discussion
Based on WHO classification, B-cell IVL is classified as a rare subtype of extra nodal diffuse large B-cell lymphoma and an independent disease entity.Citation4 IVL is a relatively rare disease presenting with multifocal proliferation of lymphoma cells in the small blood vessels.Citation5 The first case of B-cell IVL was described in 1959,Citation6 more than 300 cases have been reported to date in literature.Citation7 B-cell IVL can occur at any age, but is more frequently seen in the seventh decade of life.Citation3 Male-to-female ratio ranges from 1:1 to 3:1.Citation3,Citation8 The age of patient was 56 years in our case.
IVL presents with an intravascular lymphoid infiltrate that mainly affects the skin and central nervous system. However, an intravascular lymphoid infiltrate can involve multiple organ systems, including the lungs, kidneys, liver, heart, and adrenal glands. IVL is a subtype of lymphoma, but not causing any mass effect.Citation3 One-third of IVL cases present skin involvement. The cutaneous manifestations involve erythematous to purpuric papules, nodules, and plaques that are often distributed on the lower extremities and lower abdomen.Citation5 The cutaneous lesions show variation in appearance, and can include painful indurated erythematous eruptions, poorly circumscribed violaceous plaques, large solitary plaques, erythematous, and desquamative plaques, peau d’orange change, cellulitis, painful blue-red palpable nodular discolorations, ulcerated nodules, palpable purpura, or small red palpable spots.Citation9 Our patient presented with anasarca-type edema and hard indurated generalized plaques on the abdomen, thigh, and face. In our case, we assumed the edema was linked to the renal involvement. However, the renal findings and edema were related to the intravascular involvement rather than the renal involvement. We postulated that intravascular involvement might cause extravasation from the vascular bed that decreasing renal blood circulation. In our case, the primary problem was edema and the secondary problem was skin plaques. The edema and plaques were resolved following the treatment in our patient.
Two main subtypes of B-cell IVL have been described: the Western variant and the Asian variant. The most common subtype is western or classical variant in North America and Europe, and predominantly presents with neurologic and dermatologic findings during its course. The cutaneous features include telangiectasias, diffuse erythematous streaks, purpuric macules, and nodules. The cutaneous variant of the western variant class is less aggressive subtype than the other subtypes of B-cell IVL. It usually affects pre-menopausal females. The Asian or hemophagocytic variant is a subtype of B-cell IVL presenting anemia, thrombocytopenia, hemophagocytosis, bone marrow involvement, and respiratory symptoms, B-symptoms (fever, night-sweats, hypoalbuminemia and hepatosplenomegaly). The neurological symptoms (27%) and cutaneous lesions (15%) are less common in the Asian variant than the Western variant.Citation8 Our patient had western variant of B-cell IVL with unusual presentation. In addition, the patient developed light erythematous, hard, indurated, unclear margin generalized plaques with orange peel-like appearance (that is also seen in the classic variant). The patient with B-cell IVL manifesting with anasarca edema has not previously reported in the literature. The patient did not have any other organ involvement. The etiology of this condition is unclear, although it has been claimed that it may be related to Epstein–Barr virus and human T-cell lymphocyte virus. However, viral agents are not detected in all cases.Citation1 The postulated pathogenic mechanism for the intravascular localization of IVL may be the presence of defective adhesive molecules such as CD44 antigen and the absence of CD18 surface molecules functioning in lymphocyte extravasation. Due to similarities to other diseases, the diagnosis of IVL is performed particularly based on clinical findings. The final diagnosis is made with biopsy. However, many cases are first diagnosed with autopsy investigation. Immunohistochemical staining is positive for B-cell markers such as CD45, CD22, and CD20.Citation3 In our case, the immunohistochemical staining is positive for CD45 and CD20.
A B-cell IVL is a chemosensitive with high relapse rate, but is usually fatal. Current available treatments options include irradiation, high-dose corticosteroids, and chemotherapy. Rituximab, an anti-CD20 monoclonal antibody, is commonly administered for the treatment of B-cell IVL with skin and solid organ involvements.Citation3,Citation4 The combination chemotherapies in IVL are effective and include CHOP (cyclophosphamide, doxorubicin, Oncovin [vincristine], and prednisone), ProMACE-CytaBOM (cyclophosphamide, doxorubicin, etoposide, and prednisone/cytarabine, bleomycin, vincristine, methotrexate, and leucovorin), and ICE (ifosfamide [Ifex], mesna [Mesnex], cisplatin, and etoposide).Citation3 Alternative treatment such as allogenic peripheral blood stem cell transplant can be performed when the chemotherapy treatments are failed.Citation10 In spite of the treatments, the prognosis continues to be poor.Citation3 Our patient was treated with R-CHOP chemotherapy with remarkable clinical improvement. She did not have any recurrence during 11 months follow ups. She was still under our care while submitting the case report.
In conclusion, B-cell IVL is rare and life threatening disease. Early skin biopsy is important for early diagnosis and to start early treatment. Besides classic skin lesions, various primary and secondary clinical presentations that can be seen are related to a site of the tumor cell infiltrations. However, B-cell IVL presenting with anasarca edema was not previously reported. Even if its rarity, intravascular malign infiltration should be considered in the differential diagnosis of anasarca edema and renal failure.
Declaration of interest
There are no conflicts of interest among all authors regarding this article.
References
- Wahie S, Dayala S, Husain A, Summerfield G, Hervey V, Langtry JA. Cutaneous features of intravascular lymphoma. Clin Exp Dermatol. 2011;36(3):288–291
- Murase T, Yamaguchi M, Suzuki R, et al. Intravascular large B-cell lymphoma (IVLBCL): a clinicopathologic study of 96 cases with special reference to the immunophenotypic heterogeneity of CD5. Blood. 2007;109(2):478–485
- Satti S, Castillo R. Intravascular B-cell lymphoma. Commun Oncol. 2005;2:55–58
- Shimada K, Kinoshita T, Naoe T, Nakamura S. Presentation and management of intravascular large B-cell lymphoma. Lancet Oncol. 2009;10(9):895–902
- Kenji A, Fujimoto W, Yoshino T, et al. Intravascular lymphomatosis of the skin as a manifestation of recurrent B-cell lymphoma. J Am Acad Dermatol. 2003;48(2 Suppl):S1–S4
- Pfleger VL, Tappeiner J. On the recognition of systematized endotheliomatosis of the cutaneous blood vessels (reticuloendotheliosis)? Hautarzt. 1959;10:359–363
- Ishii W, Ito S, Kondo Y, et al. Intravascular large B-cell lymphoma with acute abdomen as a presenting symptom in a patient with systemic lupus erythematosus. J Clin Oncol. 2008;26(9):1553–1555
- Geyer H, Karlin N, Palen B, Mesa R. Asian-variant intravascular lymphoma in the African race. Rare Tumors. 2012;4:e10:26–29
- Orwatt DE, Batalis NI. Intravascular large B-cell lymphoma. Arch Pathol Lab Med. 2012;136:333–338
- Adam DN, Beleznay KM, Randhawa RS, Marton M, Zhou Y. Review of intravascular lymphoma with a report of treatment with allogenic peripheral blood stem cell transplant. Cutis. 2008;82:267–272

